File - Sarah Elizabeth Ossler, Genetic Counseling Student
advertisement

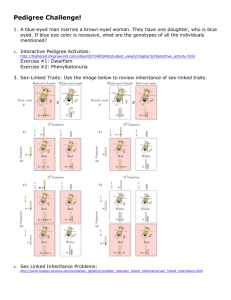
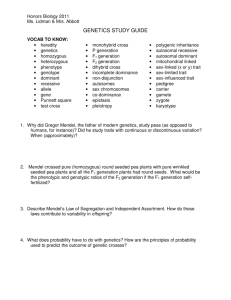
GENE MAPPING AND IDENTIFICATION: CASE STUDIES SARAH OSSLER SARAH.OSSLER@CCHMC.ORG LEARNING OBJECTIVES • Understand inheritance patterns, such as autosomal recessive inheritance and autosomal dominant inheritance • Be able to interpret and create a family history using appropriate symbols • Identify when more information is needed to make a differential diagnosis for a patient • Recall important details about genetic conditions that may be applicable to the patient • Apply knowledge of genetic conditions to the patients’ medical and family history to make a diagnosis MENDEL’S PRINCIPLES • Principle of Dominance • One allele masked another, one allele is dominant over the other • Principle of Segregation • When gametes are formed, the pairs of hereditary factors (genes) become separated, so that each sex cell (egg/sperm) receives only one kind of gene • Principle of Independent Assortment • “Members of one gene pair segregate independently from other gene pairs during gamete formation” FAMILY HISTORY • You can learn a lot from taking a family history • May make it clear to you if a certain mode of inheritance is present in a family • Three common modes of inheritance • Autosomal recessive • Autosomal dominant • X-linked AUTOSOMAL RECESSIVE EXAMPLE • Examples: Hearing loss Hemochromatosis PKU Spinal muscular atrophy • Tay Sachs • • • • AUTOSOMAL DOMINANT EXAMPLE What are some common autosomal dominant conditions? X-LINKED EXAMPLE • Fragile X Syndrome • Caused by trinucleotide repeats • What is the normal range of CGG repeats, premutation, and mutation range? • Hemophilia ACTIVITY • Now you will draw your own family tree! • Do not have to include any medical information • Do three generations (you/cousins, your parents/aunts/uncles, grandparents) • Please let me know if you have questions drawing something! WHY DO WE CARE ABOUT GENE MAPPING? • Diagnosing patients • Allows us to: • • • • Perform prenatal diagnoses Personalize medicine with pharmacogenomics Direct psychosocial counseling May aid in prevention of disease CASE STUDIES • 3 case studies • • • • Clinical description for each Ask questions about the patient Create a differential diagnosis Think of testing you could offer the patient PATIENT 1 • Patient is a 14 year old female. She went to the hospital complaining of a cold that was worsening. Her BMI was in the underweight range. The physicians gave her a chest radiograph and sputum culture, CBC panel, RPR, and Chem 16. They then diagnosed her with pneumonia. ABNORMAL LABS Abnormal Lab Normal value Her value Transferrin 250-380 219 Magnesium 1.8-3 1.6 HbA1C 3.9-5.2 6.3 WBC 4.8-11.8 13 HGB 12-15 11.5 HCT 37-47 33 Ferritin 20-120 19 Activity: Research what each of these levels mean WHAT OTHER INFORMATION DO YOU WANT ABOUT THE PATIENT IN ORDER TO MAKE A DIFFERENTIAL DIAGNOSIS? DIFFERENTIAL DIAGNOSIS • Alpha-1 antitrypsin deficiency • Activated P13K-δ Syndrome (APDS) • http://www.cam.ac.uk/research/news/scientists-discovergenetic-disease-which-causes-recurrent-respiratoryinfections • • • • Cystic Fibrosis Asthma Primary immunodeficiency This is not an exhaustive list! CYSTIC FIBROSIS • Thick mucous secretions from the epithelial surfaces of several organ systems including the respiratory tract, gastrointestinal tract, liver, genitourinary system, and sweat glands • Autosomal recessive • Delta F508 is the most common mutation WHAT TESTS WOULD YOU ORDER ON THE BASIS OF COST/BENEFIT? • Options: • Sweat chloride test • Positive test= ≥60 mEq/L • Pancreatic function tests • Pulmonary function tests • Gene testing • Most common approach- screening for the two most common mutations • If not found, can sequence the CFTR gene • Newborn Screening • Can also detect carriers, may cause extra stress in families • Activity: in groups, find costs and their diagnostic ability for the above tests MATH. PATIENT 2 • Patient is a 2 year old male. His mother is concerned that he is not meeting his developmental milestones, and wanted a consultation with her pediatrician. The pediatrician noticed several brown patches on the patients’ skin, and referred the family to genetics. WHAT OTHER INFORMATION DO YOU WANT ABOUT THE PATIENT TO MAKE A DIFFERENTIAL DIAGNOSIS? DIFFERENTIAL DIAGNOSIS • • • • • • NF1 NF2 McCune-Albright syndrome Tuberous sclerosis Fanconi Anemia Again, not an exhaustive list! NEUROFIBROMATOSIS TYPE 1 • Characterized by multiple café au lait spots • Axillary and inguinal freckling • Multiple cutaneous neurofibromas • Lisch nodules • 50% of individuals have learning disabilities • Other manifestations: • plexiform neurofibromas • optic nerve and other central nervous system gliomas • malignant peripheral nerve sheath tumors • scoliosis • tibial dysplasia • Vasculopathy • Autosomal dominant, about 50% of cases are de novo • http://www.ncbi.nlm.nih.gov/books/NBK1109/ DIAGNOSTIC CRITERIA • individual who has two or more of the following features: Six or more café au lait spots Two or more neurofibromas Freckling in the axillary or inguinal regions Optic glioma Two or more Lisch nodules (iris hamartomas) A distinctive osseous lesion such as sphenoid dysplasia or tibial pseudarthrosis • A first degree relative (parent, sibling, or offspring) with NF1 • • • • • • WHAT TESTS WOULD YOU ORDER? • Generally, mutation analysis is not needed to confirm a diagnosis in a patient. • When would you need to have a confirmed diagnosis by mutation analysis? • Mutation analysis of NF1can be useful • Sequence variants= ~90% mutation detection • Deletion/duplication analysis= ~5% • Large scale rearrangements= ~1% PATIENT 3 (THIS IS A TOUGH ONE!) • A 5 year old Caucasian female, who is previously healthy, presents to the ED with a 3 day history of vomiting and diarrhea such that she is only able to keep down a small amount of water. On exam she is clearly dehydrated, with rapid pulse and elevated respiratory rate. Initial labs show glucose of 40 (normal 45-120), as well as evidence of dehydration. Urine demonstrates a large amount of ketones. Of note, all previous medical exams and studies were normal. WHAT OTHER INFORMATION DO YOU WANT ABOUT THE PATIENT TO MAKE A DIFFERENTIAL DIAGNOSIS? DIFFERENTIAL DIAGNOSIS • • • • • • Pyloric stenosis Hyperthyroidism Organic acidemias Aminoacidemia Urea Cycle Disorder Other • Since this one is so tough, look up these conditions and see if any of them fit! DIAGNOSIS • Nongenetic! • The baby was sick with the flu LESSON • We are trained as geneticists when we hear hoof steps, we think of the Zebra instead of the horse • ALWAYS keep in mind the possibility a patient is presenting with a non-genetic illness SUMMARY • Discussed inheritance patterns, such as autosomal recessive inheritance and autosomal dominant inheritance • interpreted and created family histories using appropriate symbols • Identified when more information was needed to make a differential diagnosis for a patient • Recalled important details about genetic conditions that may be applicable to the patient • Applied knowledge of genetic conditions to the patients’ medical and family history to make a diagnosis ASSIGNMENT • Keep a food journal for about one week • Can write down the information, or use an app like my fitness pal • Keep track of calories and protein • Write a one page reflection about how you felt doing this exercise and what you learned • Full assignment is posted on Blackboard • See how many calories you can buy with $5 • You can go anywhere (grocery store, fast food restaurant, etc.) • It has to be a food that would normally be eaten (you cannot buy a ton of olive oil!) • Full assignment posted on Blackboard • Both are due for the Fetal Programming and Obesity lecture (March 11th) • Required reading: Chapter 12, Multifactorial Inheritance and Common Diseases • If you are having issues or have questions, please feel free to email me at sarah.ossler@cchmc.org!! QUESTIONS?