16th
Conference on
Retroviruses and
Opportunistic Infections,
Montreal, 2009
Correspondence to:
Dr. Adrian Smith,
Department of Public Health,
Old Road Campus,
University of Oxford, OX7 7AG
+44 1865 289239
adrian.smith@dphpc.ox.ac.uk
Role Versatility and Female Partnerships amongst MSM Sex Workers in Mombasa, Kenya
A. D. Smith1, A. Ferguson2, D. Kowuor3 , E. van der Elst 3, C. Agwanda 3, A. Muhaari 3, A.Davies3 , S.M.Graham4 , E.J.Sanders3
1. Department of Public Health, University of Oxford, UK 2. HIV and AIDS Prevention and Care Project, Kenya 3. Centre for Geographic Medicine Research-Coast, Kenya 4. University of Washington, Seattle, USA
METHODS
METHODS
Abstract W-169
•81 MSM-SW participated in the study. They recorded 1738 sexual
prospective sexual behaviour diaries (see below) and a computer assisted
encounters with 1212 different partners over 6 weeks follow up in 2007.
questionnaire recording sociodemographic information, recall of lifetime and
recent sexual behaviour, and detailed characteristics of three most recent
sexual relationships.
Table 3. Sexual behaviours with men and women (diary)
MSM-SW with male
MSM-SW with male
partners only
and female partners
Gender exclusivity
Encounters
n
(% total )
•Most MSM-SW reported both male and female partners (i.e. non-exclusive),
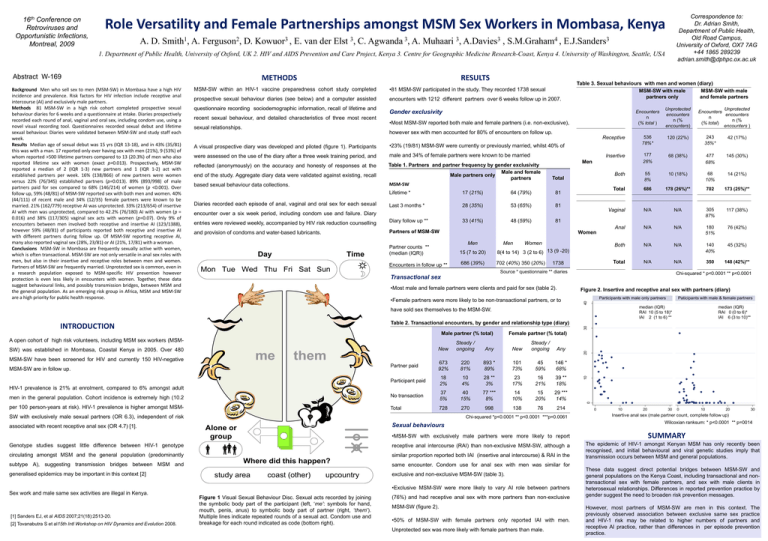
A visual prospective diary was developed and piloted (figure 1). Participants
•23% (19/81) MSM-SW were currently or previously married, whilst 40% of
were assessed on the use of the diary after a three week training period, and
male and 34% of female partners were known to be married
reflected (anonymously) on the accuracy and honesty of responses at the
end of the study. Aggregate diary data were validated against existing, recall
based sexual behaviour data collections.
Table 1. Partners and partner frequency by gender exclusivity
Male and female
Male partners only
partners
MSM-SW
Total
17 (21%)
64 (79%)
81
Last 3 months *
28 (35%)
53 (65%)
81
entries were reviewed weekly, accompanied by HIV risk reduction counselling
Diary follow up **
33 (41%)
48 (59%)
81
and provision of condoms and water-based lubricants.
Partners of MSM-SW
Diaries recorded each episode of anal, vaginal and oral sex for each sexual
encounter over a six week period, including condom use and failure. Diary
Day
Time
Mon Tue Wed Thu Fri Sat Sun
Receptive
536
78%*
120 (22%)
243
35%*
42 (17%)
Insertive
177
26%
68 (38%)
477
68%
145 (30%)
Both
55
8%
10 (18%)
68
10%
14 (21%)
Total
686
178 (26%)**
702
173 (25%)**
Vaginal
N/A
N/A
305
87%
117 (38%)
Anal
N/A
N/A
180
51%
76 (42%)
Both
N/A
N/A
140
40%
45 (32%)
Total
N/A
N/A
350
148 (42%)**
Men
Lifetime *
Women
Men
Men
Women
Partner counts **
(median (IQR))
15 (7 to 20)
8(4 to 14) 3 (2 to 6) 13 (9 -20)
Encounters in follow up **
686 (39%)
702 (40%) 350 (20%)
1738
Source * questionnaire ** diaries
Chi-squared * p<0.0001 ** p<0.0001
Transactional sex
•Most male and female partners were clients and paid for sex (table 2).
•Female partners were more likely to be non-transactional partners, or to
Figure 2. Insertive and receptive anal sex with partners (diary)
Participants with male only partners
median (IQR)
RAI 10 (5 to 18)*
IAI 2 (1 to 6) **
me
MSM-SW have been screened for HIV and currently 150 HIV-negative
them
Partner paid
MSM-SW are in follow up.
30
Male partner (% total)
New
Steady /
ongoing
Any
673
92%
220
81%
2%
New
Steady /
ongoing
Any
893 *
89%
101
73%
45
59%
146 *
68%
4%
28 **
3%
23
17%
16
21%
39 **
18%
40
15%
77 ***
8%
14
10%
15
20%
29 ***
14%
270
998
138
76
214
CONCLUSIONS
18
10
Participant paid
HIV-1 prevalence is 21% at enrolment, compared to 6% amongst adult
No transaction
per 100 person-years at risk). HIV-1 prevalence is higher amongst MSM-
Total
728
0
men in the general population. Cohort incidence is extremely high (10.2
37
5%
Female partner (% total)
SW with exclusively male sexual partners (OR 6.3), independent of risk
Chi-squared *p<0.0001 ** p<0.0001 ***p=0.0061
Sexual behaviours
Alone or
group
•MSM-SW with exclusively male partners were more likely to report
Genotype studies suggest little difference between HIV-1 genotype
receptive anal intercourse (RAI) than non-exclusive MSM-SW, although a
CONCLUSIONS
circulating amongst MSM and the general population (predominantly
similar proportion reported both IAI (insertive anal intercourse) & RAI in the
Where did this happen?
study area
coast (other)
upcountry
same encounter. Condom use for anal sex with men was similar for
exclusive and non-exclusive MSM-SW (table 3).
•Exclusive MSM-SW were more likely to vary AI role between partners
Sex work and male same sex activities are illegal in Kenya.
[1] Sanders EJ, et al AIDS 2007;21(18):2513-20.
ABSTRACT
[2] Tovanabutra
S et al15th Intl Workshop on HIV Dynamics and Evolution 2008.
REFERENCES
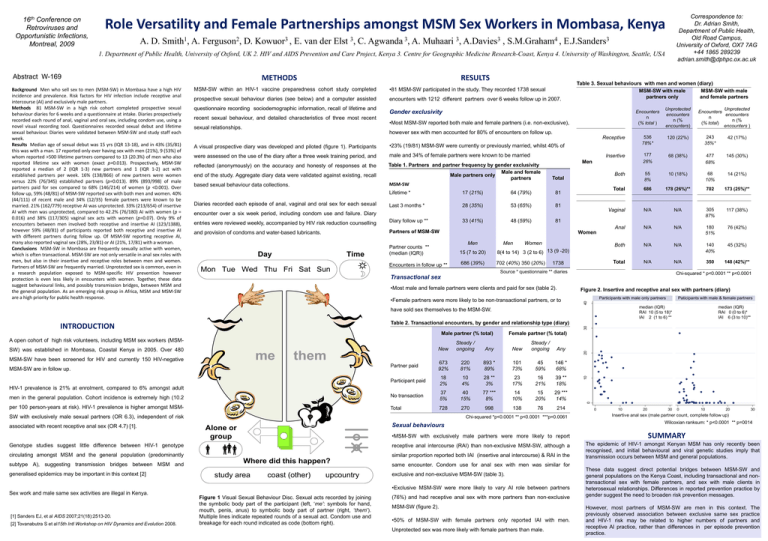
Figure 1 Visual Sexual Behaviour Disc. Sexual acts recorded by joining
the symbolic body part of the participant (left, ‘me’: symbols for hand,
mouth, penis, anus) to symbolic body part of partner (right, ‘them’).
Multiple lines indicate repeated rounds of a sexual act. Condom use and
breakage for each round indicated as code (bottom right).
20
SW) was established in Mombasa, Coastal Kenya in 2005. Over 480
generalised epidemics may be important in this context [2]
median (IQR)
RAI 0 (0 to 6)*
IAI 6 (3 to 10)**
10
A open cohort of high risk volunteers, including MSM sex workers (MSM-
subtype A), suggesting transmission bridges between MSM and
Paticipants with male & female partners
Table 2. Transactional encounters, by gender and relationship type (diary)
INTRODUCTION
associated with recent receptive anal sex (OR 4.7) [1].
Unprotected
Encounters
encounters
n
n (%
(% total)
encounters )
however sex with men accounted for 80% of encounters on follow up.
have sold sex themselves to the MSM-SW.
METHODS
Unprotected
encounters
n (%
encounters)
40
BACKGROUND
MSM-SW within an HIV-1 vaccine preparedness cohort study completed
Receptive anal sex (male partner count, complete follow up)
Background Men who sell sex to men (MSM-SW) in Mombasa have a high HIV
incidence and prevalence. Risk factors for HIV infection include receptive anal
intercourse (AI) and exclusively male partners.
Methods 81 MSM-SW in a high risk cohort completed prospective sexual
behaviour diaries for 6 weeks and a questionnaire at intake. Diaries prospectively
recorded each round of anal, vaginal and oral sex, including condom use, using a
novel visual recording tool. Questionnaires recorded sexual debut and lifetime
sexual behaviour. Diaries were validated between MSM-SW and study staff each
week.
Results Median age of sexual debut was 15 yrs (IQR 13-18), and in 43% (35/81)
this was with a man. 17 reported only ever having sex with men (21%), 9 (53%) of
whom reported >500 lifetime partners compared to 13 (20.3%) of men who also
reported lifetime sex with women (exact p=0.013). Prospectively, MSM-SW
reported a median of 2 (IQR 1-3) new partners and 1 (IQR 1-2) act with
established partners per week. 16% (138/866) of new partners were women
versus 22% (76/345) established partners (p=0.013). 89% (893/998) of male
partners paid for sex compared to 68% (146/214) of women (p <0.001). Over
follow up, 59% (48/81) of MSM-SW reported sex with both men and women. 40%
(44/111) of recent male and 34% (12/35) female partners were known to be
married. 21% (162/779) receptive AI was unprotected. 33% (213/654) of insertive
AI with men was unprotected, compared to 42.2% (76/180) AI with women (p =
0.016) and 38% (117/305) vaginal sex acts with women (p=0.07). Only 9% of
encounters between men involved both receptive and insertive AI (123/1388),
however 59% (48/81) of participants reported both receptive and insertive AI
with different partners during follow up. Of MSM-SW reporting receptive AI,
many also reported vaginal sex (28%, 23/81) or AI (21%, 17/81) with a woman.
Conclusions MSM-SW in Mombasa are frequently sexually active with women,
which is often transactional. MSM-SW are not only versatile in anal sex roles with
men, but also in their insertive and receptive roles between men and women.
Partners of MSM-SW are frequently married. Unprotected sex is common, even in
a research population exposed to MSM-specific HIV prevention however
protection is even less likely in encounters with women. Together, these data
suggest behavioural links, and possibly transmission bridges, between MSM and
the general population. As an emerging risk group in Africa, MSM and MSM-SW
are a high priority for public health response.
RESULTS
(76%) and had receptive anal sex with more partners than non-exclusive
MSM-SW (figure 2).
•50% of MSM-SW with female partners only reported IAI with men.
REFERENCES
Unprotected sex was more likely with female partners than male.
0
10
20
30
0
10
20
30
Insertive anal sex (male partner count, complete follow up)
Wilcoxian ranksum: * p<0.0001 ** p=0014
SUMMARY
The epidemic of HIV-1 amongst Kenyan MSM has only recently been
recognised, and initial behavioural and viral genetic studies imply that
transmission occurs between MSM and general populations.
These data suggest direct potential bridges between MSM-SW and
general populations on the Kenya Coast, including transactional and nontransactional sex with female partners, and sex with male clients in
heterosexual relationships. Differences in reported prevention practice by
gender suggest the need to broaden risk prevention messages.
However, most partners of MSM-SW are men in this context. The
previously observed association between exclusive same sex practice
and HIV-1 risk may be related to higher numbers of partners and
receptive AI practice, rather than differences in per episode prevention
practice.