3. Dolan LA, Sabesan V, Weinstein SL, et al. Preference assessment
advertisement

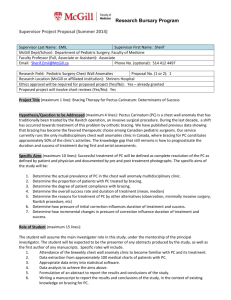
BrAIST design: supplement Supplemental Material NIH R21 Planning Grant Development of the science and infrastructure for BrAIST began in 2001. The first critical step was to collaborate with the Clinical Trials and Statistical Data Management Center (DMC) at the University of Iowa. Established in 1989, the DMC had significant experience designing infrastructure for the development, conduct, management, administration and statistical analysis of clinical trials. Specific areas of expertise include clinical data management, case report form design, database design and biostatistical analysis. We sought input from physicians who supported bracing, and from those who actively questioned its effectiveness, in order to produce a protocol that would not be biased in favor of one treatment arm or the other. Eight such clinicians, all with expertise in the study and practice of pediatric spine care, comprised the Protocol Development Committee. The Committee produced a preliminary protocol outlining the inclusion/exclusion criteria, necessary radiographic measurements, appropriate endpoints, and informed consent procedures. The Committee also discussed side effects of treatment, estimated the prevalence of certain risk factors and came to consensus concerning the clinically important effect size. 1 BrAIST design: supplement The preliminary protocol was included in a NIAMS Clinical Trial Planning Grant application. 1 The general objective of this NIAMS program is to address preliminary design and methodological elements essential to the conduct of a successful Phase III clinical trial, particularly one that involves multiple centers. The expected product of the program is a detailed clinical trial research plan including a complete manual of operations and procedures (MOOP). The grant was submitted in 2001 and was awarded in September 2002 (R21 AR49587). The BrAIST planning grant had four general goals: 1) appointing key personnel and creating the structural organization of the trial; 2) developing procedures for data management and safety monitoring; 3) developing materials, methods and the data analysis plan; and 4) recruiting participating institutions. Beyond these goals, most resources during the planning grant phase were directed at demonstrating feasibility: establishing the ethics of randomization, the willingness of subjects to enroll into a randomized trial, required effect size, availability of an adequate number of participating sites, and determining the reliability and validity of the brace wear monitoring system. Ethics Although many of our colleagues were enthusiastic and supported randomized allocation, we also encountered resistance to the idea of a 2 BrAIST design: supplement randomized trial. Colleagues questioned the ethics of randomizing to the observation arm (essentially a placebo treatment), given that some centers consider bracing as the standard of care. Knowing that the question of ethics may influence grant funding as well as physician and patient participation, we designed a survey to evaluate the degree to which pediatric orthopaedists agree on the relative benefits of bracing and observation as an indirect measure of community equipoise. 2 Clinicians had widely varying opinions concerning the risk reduction attributable to bracing. For example, given the same set of presenting characteristics (thoracic curve, Cobb angle <35 degrees and pre-menarchal at presentation) physicians indicated the attributable risk reduction would range from 0 to 70 percent. These results suggest bracing is not supported by a reasonably definitive research literature or by agreement among those who prescribe the standard. Therefore, we concluded that under the guidelines set down by the Declaration of Helsinki, it was ethical to randomize patients either bracing or observation, given there was no community consensus concerning the relative benefits of the treatments. Enrollment The most common and potentially threatening issue to face clinical trials, especially randomized trials, is enrollment. Estimating enrollment is not 3 BrAIST design: supplement straightforward. Investigators need to define the patient population, estimate the willingness of patients to participate, get accurate estimates of the availability of potential subjects at each potential center, and obtain signed commitments to participate. Once the Protocol Development Committee defined the population of interest, the treatments and the data collection protocol, we put together a synopsis of the project and presented it to both potential subjects and physician collaborators. Patient Willingness to Participate and Required Effect Size Because the percentage of subjects agreeing to randomization is central to the feasibility of the trial, one of our priorities during our pre-trial planning phase was to gather direct estimates of the participation rate. We conducted a randomization simulation 3 based on previous work by Llewellyn-Thomas. 4-7 Adolescents and their parents read an education module about AIS, including the natural history, long-term outcomes, surgical and conservative treatments, and about the characteristics of a randomized trial. They were then asked to imagine they were approached about a study where they would be randomized to either bracing or observation. Overall, 56% of the parents and 48% of the children stated they would agree to participate. Importantly, 32% of parents and children jointly agreed that they would participate. Based on these data, we estimated 4 BrAIST design: supplement that 25% of all patient/parent pairs approached during the actual study would agree to participate. The average required risk reduction of parents with children with scoliosis was 50% (i.e., a decrease in risk of surgery from 60% to 30%). Data from this simulation contributed to our calculations of subject accrual and effect size. Center Recruitment The study synopsis was sent to more than 40 physicians who regularly treat children with spinal deformity in the United States and Canada. Invitations to participate were based on several factors, including past involvement in research, size of clinical population, and geography. Investigators at 32 institutions expressed interest in participating. All had to confirm they were in equipoise concerning the options of bracing and observation for the target population. To estimate how many eligible subjects would be encountered at each institution, potential sites were asked to perform a chart review of all AIS patients meeting BrAIST inclusion criteria who were seen in a recent and representative 3month period of time. Investigators recorded the following information on a standard datasheet: sex, age, curve type, Cobb angle, Risser sign, menstrual status, and language spoken. The number of patients ranged from 4 to 25 per 3- 5 BrAIST design: supplement month period. These data indicated that the 20 centers with the highest volume would encounter approximately 1200 eligible patients in a 12-month period. To determine the duration of data collection, we created algorithms based on patient characteristics. For example, under the null hypothesis of no risk reduction due to bracing, we estimated that a Risser 0 premenstrual female with a thoracic curve of 35 degrees or greater would meet a study endpoint 6 months after recruitment. These algorithms were then applied to the patient data submitted by the potential centers. Based on these calculations, we determined that in order to finish data collection within 4 years, we would have to complete recruitment within the first 18 months of the grant, and that approximately 20 centers would be needed. The MOOP was developed in accordance with NIAMS guidelines. 8 The MOOP covers all operational aspects of the trial in detail in order to promote standardization across all participating sites. An outline of the contents of the MOOP is presented in Table I. Objective Dose Monitoring In 2002, methods for the objective monitoring of brace wear were just starting to emerge. Electronic measurement instruments had been designed using different modalities, such as skin temperature, pressure, motion, and 6 BrAIST design: supplement galvanic skin response, but none had been used in a clinical trial. We conducted accuracy and reliability experiments using various temperature loggers (HOBO, TidbiT and Stowaway) manufactured by the Onset Computer Company (Onset Computer, Bourne, Massachusetts) as an indirect measure of brace wear time. The logger was tested using AIS patients from four medical centers. Twenty-three subjects who were undergoing bracing were recruited and asked to wear their brace at least 16 hours/day. All subjects kept standardized diaries of wear time and activity for four weeks. The loggers measured the temperature every ten minutes and the raw temperature data, date and time were downloaded and converted to on/off (worn/not worn) indicators using multiple logistic modeling for each individual. These regression models yielded the temperature range within which the brace had the highest likelihood of actually being worn. These ranges were then averaged over the entire group and a single temperature range was set. The brace was coded as being worn when the temperature reading was between 83.30 and 98.02 degrees F. Average wear time and the agreement between the logger and the diaries were evaluated for each patient, hospital and the group overall, as well as for day and nighttime hours. The average wear time per day was 11.80 hours (range 0 to 24.00) according to the diaries, and 11.82 according to the logger (range 0 to 24.00). The average difference between log 7 BrAIST design: supplement and logger readings was -0.004 hours overall (range –2.17 to 1.64), and there were no significant differences for any individual subjects. Thus, the temperature logger and algorithm developed were an accurate and reliable proxy for log data over both day and night wear, and across four different sites. There was large variability in wear time across subjects: some subjects, despite being monitored, rarely wore their braces, while others wore them consistently greater than 18 hours per day. Therefore, this study documented the variation in wear time (dose) necessary to establish the relationship between dose and curve response in future studies. Protocol Violations Deviations from the protocol were submitted to the DMC, tabled by site and provided to the Data Safety Monitoring Board for review. Major protocol violations included failure to follow approved informed consent procedures, enrollment of an ineligible patient, change from one treatment arm to another, failure to obtain x-rays, height measurements and/or temperature monitor data, missed study visits and termination from the study by the investigator without prior approval of the CCC. 8 BrAIST design: supplement Adverse Events (AEs) There are no known major physical side-effects associated with brace wear. However, mild skin irritation is frequent. Rare, but possible, side-effects reported in the literature include transient decreases in glomerular filtration rate, abnormal breast development, and slight decreases in lung capacity while wearing the brace. Other examples of AEs include back pain, anxiety, sleeping problems, depression, and problems with skin on the trunk such as bruising, lacerations, ulcers, pressure sores or rash. Adverse event report forms were sent to the DMC with 5 days of discovery. A Serious Adverse Event was any adverse experience associated with the protocol that results in any of the following outcomes: death, a life-threatening adverse experience, inpatient hospitalization or prolongation of existing hospitalization, a persistent or significant disability/incapacity. All serious adverse events were reported to the CCC and the medical monitor within 24 hours of discovery. AEs were included in monthly reports and reported to the Data Safety and Monitoring Board. Data Sharing Plan In compliance with the NIH Data Sharing Plan, data from all screened patients and enrolled subjects will eventually be available to the public. The data 9 BrAIST design: supplement and associated documentation will be available to users under a data-sharing agreement that provides for: (1) a commitment to using the data only for research purposes and not to identify any individual participant; (2) a commitment to securing the data using appropriate computer technology; and (3) a commitment to destroying or returning the data after analyses are completed. The dataset will become available after all major findings have been published. 10 BrAIST design: supplement Table I. Contents of the Manual of Operations and Procedures 1) Introduction 2) History and Background of the Problem 3) Study Organization, Centers, Committees 4) Institutional Review Board Approval Procedures 5) Study Protocol i) Design: Phase III, prospective, partially randomized preference design ii) Participating Sites iii) Subject Population iv) Inclusion and Exclusion Criteria v) Screening Process and Baseline Evaluation vi) BrAIST Education Module and Informed Consent Procedures vii) Treatment Assignment Plan: Randomization and Preference viii) Bracing Treatment Protocol and Temperature Monitoring Instructions ix) Observation Treatment Protocol x) Schedule of Visits and Evaluations xi) Procedures for Film Acquisition xii) Follow-up Visits (1) Monthly Telephone Calls (2) Schedule of Office Visits (3) Procedure for Missed Appointments 11 BrAIST design: supplement (4) Non-Compliance and Subject Initiated Treatment Change (Crossover) xiii) Endpoints (1) Curve Progression to ≥50 Degrees (2) Skeletal Maturity (3) Subject Withdrawal 6) Data Collection and Study Forms a) Clinical, Radiographic and Orthotic Evaluation b) Recording Data on Case Report Forms c) Radiographic and Form Completion Schedule – Bracing Treatment d) Radiographic and Form Completion Schedule – Observation Treatment e) Subject Handout – Instructions for Completing Questionnaires 7) Statistical Plan 8) Payment Plan 9) Data Sharing Plan 10) Data Quality, Safety and Monitoring Activities a) Data Safety and Monitoring Board Membership and Process b) Bracing Evaluation Committee Membership and Process c) Internal Safety Review d) Onsite Monitoring e) Adverse Events f) Protocol Violations g) Data Management Procedures at the DMC 12 BrAIST design: supplement References 1. NIAMS Clinical Trial Planning Grant Cooperative Agreement (U34) PAR-11- 169]. Available at: http://grants.nih.gov/grants/guide/pa-files/PAR-11-169.html. 2. Dolan LA, Weinstein SL. Surgical rates after observation and bracing for adolescent idiopathic scoliosis: an evidence-based review. Spine 2007;32:S91S100. 3. Dolan LA, Sabesan V, Weinstein SL, et al. Preference assessment of recruitment into a randomized trial for adolescent idiopathic scoliosis. J Bone and Joint Surg. 2008;90:2594-605. 4. Llewellyn-Thomas H, Sutherland HJ, Tibshirani R, et al. The measurement of patients' values in medicine. Medical Decision Making. 1982;2:449-62. 5. Llewellyn-Thomas HA. Investigating patients' preferences for different treatment options. Canadian Journal of Nursing Research. 1997;29:45-64. 6. Llewellyn-Thomas HA, Thiel EC, Clark RM. Patients versus surrogates: whose opinion counts on ethics review panels? Clinical Research. 1989;37:501-5. 13 BrAIST design: supplement 7. Llewellyn-Thomas HA, Thiel EC, Sem FW, et al. Presenting clinical trial information: a comparison of methods. Patient Education & Counseling. 1995;25:97-107. 8. Guidelines for Developing a Manual of Operations and Procedures (MOOP)]. Available at: http://www.niams.nih.gov/Funding/Clinical_Research/NIAMS_guidelines.asp. 14