A Brief History of Microbiology
advertisement

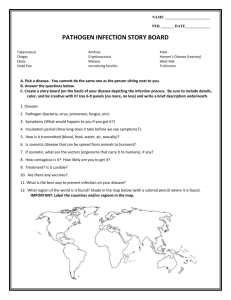
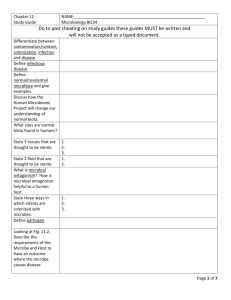
Microbe-Human Interactions: Infection and Disease Chapter 13 Copyright © The McGraw-Hill Companies, Inc) Permission required for reproduction or display. 13.1 The Human Host • Pathology – science of study of disease • Body surfaces are constantly exposed to microbes • Leads to infection - pathogenic microorganisms penetrate the host defenses, enter the tissues, and multiply • Infectious disease: the disruption of a tissue or organ caused by microbes or their products Resident Biota • Normal (resident) biota • Cell for cell, microbes on the human body outnumber human cells at least ten to one • Ex: S. epidermidis on skin, E. coli in intestine • Commensalism – one benefits, other unaffected; can become opportunistic (cause disease when given opportunity) • Mutualism – both benefit (ex. E. coli produces vit K, we provide the habitat) Acquiring the Normal Microbiota • Birth canal • Food • Breathing • Natural succession • Lactobacilli • Coliforms • Anaerobes Impact of the Normal Flora • Biological success (their “perspective”) • Exclude potential pathogens • Provide some nutrition to the host • Can improve host nutrition • Immune stimulation • Also have potential negative impacts Sites Thought to be Sterile • Sterilization • Removes all viable microorganisms including viruses and bacterial endospores • Material is said to be sterile 13.2 The Progress of an Infection • Pathogen: a microbe whose relationship with its host is parasitic and results in infection and disease • Type and severity of infection depend on pathogenicity of the organism and the condition of its host Factors that Increase Susceptibility Definition of a Terms • Pathogen: A microbe that can cause disease is a susceptible individual • Virulence: The ability of a microbe to cause disease in another organism, how quickly they infecti • Infection: The colonization of an organism by a microorganism - with or without disease • Communicable: The ability of a disease-causing organism to be spread between individuals • Virulence Factors: factors that cause disease or aid in spread of disease quickly in host or other hosts Pathogenicity • Pathogenicity: an organism’s potential to cause infection or disease • True pathogens • Opportunistic pathogens Virulence • The degree of pathogenicity • Determined by its ability to • Establish itself in the host • Cause damage • Virulence factor: any characteristic or structure of the microbe that contributes to its virulence • Different healthy individuals have widely varying responses to the same microorganism: hosts evolve • Pathogen: actual agent of disease, MRSA – S. aureus • BACTERIAL, VIRAL, FUNGAL, HELMINTH • Carrier: Infected healthy individual, no symptoms (asymptomatic), or very mild form of disease, yet they both can spread disease to others – many bacterial and viral pathogens • Classic case was typhoid Mary (look it up) Microbiology – Chapter 13 Reservoir: Where pathogen is maintained , can be in an organism (animal), in the environment (stagnant water - Legionella), or even in soil (Clostridia) Vector: Agent that spreads pathogens from host to host 1. Arthropod: flea; mosquito, tick 2. Inanimate: things, toys, dirty hands, needles, (sometimes called “fomites”) • Mechanical vectors • Passive carriers • Pathogens external • Biological vector • Vector is infected • Pathogens internal Stages in Infections Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Finding a Portal of Entry Attaching Firmly Surviving Host Defenses Causing Damage (Disease) Skin Fimbriae Directdamage GI tract Capsules Avoiding phagocytosis Respiratory tract Surface proteins Urogenital tract Viral spikes Endogenous biota Avoiding death Inside phagocyte Absence of specific immunity Toxins and/or enzymes Indirect damage Inducing inappropriate, excessive host response Exiting Host Portals of exit Respiratory tract, salivary glands Skin cells Fecal matter Urogenital tract Blood Becoming Established: Step OnePortals of Entry • Microbe enters the tissues of the body by a portal of entry • Usually a cutaneous or membranous boundary • Normally the same anatomical regions that support normal biota Infectious Agents that Enter the Skin • Nicks, abrasions, and punctures • Intact skin is very tough- few microbes can penetrate • Some create their own passageways using digestive enzymes or bites • Examples • Staphylococcus aureus • Streptococcus pyogenes, Haemophilus aegyptius • Chalmydia trachomatis • Neisseria gonorrhoeae The Gastrointestinal Tract as Portal • Pathogens contained in food, drink, and other ingested substances • Adapted to survive digestive enzymes and pH changes • Examples • Salmonella, Shigella, Vibrio, Certain strains of Escherichia coli, Poliovirus, Hepatitis A virus, Echovirus, Rotavirus, Entamoeba histolytica, Giardia lamblia The Respiratory Portal of Entry • The portal of entry for the greatest number of pathogens • Respiratory droplets: cough, sneeze, air-born droplet • Examples • Flu, colds, strept throat, staph infections of wounds Urogenital Portals of Entry • Sexually transmitted diseases (STDs) • Enter skin or mucosa of penis, external genitalia, vagina, cervix, and urethra • Some can penetrate an unbroken surface • Examples • Syphilis • Genital warts • Chlamydia • Herpes Sexually Transmitted Diseases Pathogens that Infect During Pregnancy and Birth • Horizontal: Mother to infant • Prenatal - can cross the placenta (ex. the syphilis spirochete, HIV) • Perinatal - when the child is contaminated by the birth canal at birth • STDs like gonorrhea and syphilis,chlamydia blindness Becoming Established: Step TwoAttaching to the Host (Adhesion) Figure 13.4 Becoming Established: Step ThreeSurviving Host Defenses • Phagocytes -WBCs that engulf and destroy pathogens • Antiphagocytic factors: used by some pathogens to avoid phagocytes • Leukocidins: toxic to white blood cells, produced by Streptococcus and Staphylococcus • Extracellular surface layer: makes it difficult for the phagocyte to engulf them, for example- Streptococcus pneumonia, Salmonella typhi, Neisseria meningitides, and Cryptococcus neoformans • Some can survive inside phagocytes after ingestion: Legionella, Mycobacterium, and many rickettsias Causing Disease: How Virulence Factors Contribute to Tissue Damage Figure 13.5 Extracellular Enzymes • Break down and inflict damage on tissues or dissolve the host’s defense barriers • Examples • Mucinase • Collagenase – brks down collagen to allow spread • Hyaluronidase – brk down hyluranic acid, the sugar that holds some cells together • Some react with components of the blood (coagulase – cause blood clots, and hemolysin – lyses RBCs) • Enzymes: Collagenase, Hyaluronidase - Causes necrosis and blackening of tissue (inches of progression in hours) Bacterial Toxins • Specific chemical product that diffuse into tissue causing damage/ enhance invasion/ avoid defenses • Exotoxin – excreted outside of cell, Gram +/bacteria • Ex: C. botulimun – powerful neurotoxin, Necrotoxin of flesh eating Strep • Endotoxin – released by Gram (-) bacteria when cells lyse • Ex. Lipid A – Shigella can cause high fevers and even shock Endotoxin - Lipid A – raises fever, and shock in Gram (-) pathogens Endotoxins and Exotoxins Figure 13.6 The Process of Infection and Disease • Establishment, Spread, and Pathologic Effects • Microbes eventually settle in a particular target organ and continue to cause damage at the site • Frequently weakens host tissues • Necrosis: accumulated damage leads to cell and tissue death • Patterns of Infection Establishment and Location of Infection Figure 13.7 Stages in Infections Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Finding a Portal of Entry Attaching Firmly Surviving Host Defenses Causing Damage (Disease) Skin Fimbriae Directdamage GI tract Capsules Avoiding phagocytosis Respiratory tract Surface proteins Urogenital tract Viral spikes Endogenous biota Avoiding death Inside phagocyte Absence of specific immunity Toxins and/or enzymes Indirect damage Inducing inappropriate, excessive host response Exiting Host Portals of exit Respiratory tract, salivary glands Skin cells Fecal matter Urogenital tract Blood The Portal of Exit: Vacating the Host Figure 13.9 The Persistence of Microbes and Pathologic Conditions • Latency: a dormant state • The microbe can periodically become active and produce a recurrent disease • Examples • Herpes simplex, Hepatitis B, AIDS, EpsteinBarr • Sequelae: long-term or permanent damage to tissues or organs Acquisition and Transmission of Infectious Agents • Communicable disease: when an infected host can transmit the infectious agent to another host and establish infection in that host • Transmission can be direct or indirect • Contagious agent: highly communicable • Noncommunicable disease: does not arise through transmission of the infectious agent from host to host • Acquired through some other, special circumstance • Compromised person invaded by his or her own microbiota • Individual has accidental contact with a microbe in a nonliving reservoir Patterns of Transmission in Communicable Diseases Figure 13.12 Transmission • Contact transmission • Indirect transmission • Vehicle: any inanimate material commonly used by humans that can transmit infectious agents (food, water, biological products, fomites) • Contaminated objects (doorknobs, telephones, etc.) • Food poisoning • Oral-fecal route • Air as a vehicle • Indoor air • Droplet nuclei • Aerosols Direct Contact • Touching Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. • Kissing Umbilical cord • Sexual Intercourse • Vertical transmission • prenatal -- across placenta (a) • perinatal -- during or shortly after birth Placenta Nosocomial Infections: The Hospital as a Source of Disease • Nosocomial infections: infectious diseases that are acquired or develop during a hospital stay • 2-4 million cases a year • The importance of medical asepsis •Asepsis: any practice that prevents the entry of infectious agents into sterile tissues Universal Blood and Body Fluid Precautions • Universal precautions (UPs): guidelines from the Centers for Disease Control and Prevention • Assume that all patient specimens could harbor infectious agents • Include body substance isolation (BSI)techniques to be used in known cases of infection