Nerves and Muscles Vivas
advertisement

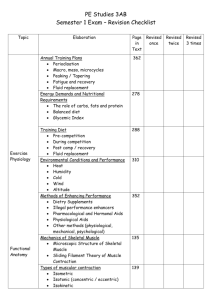
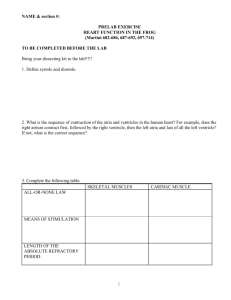
NERVES AND MUSCLES VIVAS Nerves 2011-2, 2010-1 Describe the resting membrane potential of a cell - There is difference in electronic charge across a cell membrane - The inside is negative compared to the outside - Resting MP results from separation of positive and negative charges across a cell membrane - Neuron average RMP -70 mV (about the equilibrium potential for K+) What conditions are required to create a resting membrane potential Across the lipid bilayer: 1. Must be an unequal distribution of ions across the membrane (creating a concentration gradient) 2. The membrane must be permeable to one or more of those ions (i.e. ion channels) In a neuron what ions are involved and how is the concentration gradient produced - K+ and Na+ - K+ is primarily intracellular and Na+ extracellular - Passive movement of ions occur via selective ion channels - More (leak) K+ channels open at rest so K+ is prime determinant of the RMP - Na-K ATPase actively move ions against their electrochemical gradient to maintain RMP 2007-2, 2005-1, 2003-1 Draw and label an action potential of a neuron 1. RMP(-70mV); 2. Firing potential (-55mV) 3. Voltage gated Na channels open –> Depolarisation and overshoot: 0mV -> +35mV 4. Na+ channels close (inactivated state) and voltage gated K+ channels open (slower to open) 5. Na+ back to resting state 6. After-hyperpolarization (K+ channels slower to close) 7. K+ channels close -> RMP 2010-1, 2007-2 Describe the ionic fluxes during the action potential Fast voltage gated Na channels - influx - Rapid increase due to positive feedback - Then repolarization by: 1. Rapidly to inactivated state (ARP) 2. Gradient reversed during overshoot 3. K+ channels open Slower voltage gated K+ channels - efflux - Negative feedback - Slower to open and close - Causes hyperpolarisation - (which de-inactivates the Na-channels) - Hyperpolarisation = RRP 2007-2 Where are ion channels distributed in myelinated neurons - Voltage gated Na+ concentrated at nodes of Ranvier and initial segment of myelinated neuron - Na+ channels are flanked by K+ channels involved in repolarization 2003-1 Discuss the factors that affect conduction Myelinated vs unmyelinated - Myelin, a protein–lipid complex that is wrapped around the axon - Peripheral nervous system: Schwann cell wraps its membrane around an axon up to 100 times - CNS most neurons are myelinated by oligodendrocytes rather than Schwann cells - Unmyelinated: surrounded by Schwann cells without the wrapping of the Schwann cell membrane A, B are mylenated, C are unmyelinated Saltatory vs non-saltatory - Myelinated nerves can conduct up to 50x faster - The AP will jump (via a current sink) from node to node (of Ranvier) Size - Larger diameter = faster conduction - Larger: proprioception, somatic motor function, conscious touch, pressure - Smaller: pain and temp, autonomic function Direction of the conduction - Orthodromic conduction is natural synapse/receptor -> along axon -> to termination - Antidromic is in the opposite direction – prevented by synapses (conduction only permited in one direction) Extra: “All-or-none” law - Once the AP is generated it will have constant amplitude and form, no increase in stimuli will change the AP (note- this is for a single neuron, no a nerve containing many) Extras: - Theshold intensity varies with duration - weaker need longer, stronger less time, as per strengthduration curve - Slowly rising current may fail to generate AP due to adaptation - Local response: subthreshold stimuli -> local electrotonic potentials - Excitability is the reciprocal of threshold - Absolute refractory period “occurs from the time of firing until repolarization is about 1/3 complete) - Mixed nerves contain neurons of many sizes w/ different thresholds, a small stimulus -> small AP, maximal stimulus -> maximal AP 2011-1 What are the different types of nerve fibres (What classifications are there) Myelinated vs un myelinated - Myelin, a protein–lipid complex that is wrapped around the axon - Peripheral nervous system: Schwann cell wraps its membrane around an axon up to 100 times - CNS most neurons are myelinated by oligodendrocytes rather than Schwann cells - Unmyelinated: surrounded by Schwann cells without the wrapping of the Schwann cell membrane A, B are mylenated, C are unmyelinated Saltatory vs non-saltatory - Myelinated nerves can conduct up to 50x faster - The AP will jump (via a current sink) from node to node (of Ranvier) Size - Larger diameter = faster conduction - Larger: proprioception, somatic motor function, conscious touch, pressure - Smaller: pain and temp, autonomic function Classifications Gasser ABC (A – αβγδ), A and B myelinated, C unmyelinated Numerical (sensory neuron) Ia, Ib, II, III, IV - Aα (Ia) are large myelinated somatic motor or proprioception - Aδ (III) are smaller pain and temp fibers What is the clinical relevance to emergency medicine Pain fibres are smaller and better penetrated by local anaesthetic leading to loss of pain before loss of touch or proprioception Susceptibilty to: Hypoxia Pressure Local anaesthetic Most A B C Intermediate B A B Least C C A Skeletal muscle Definitions and Facts Thick filament – myosin II, cross bridges w/ actin and have a catalytic site that hydolyses ATP Thin filament – Actin in long double helix, w/ troponmyosin convering binding site at rest Troponin T – binds the troponin to tropomyosin Troponin I – inhibits the interaction of actin with myosin Troponin C – contains the binding site for Ca2+ RMP of muscle -90mV AP lasts 2-4ms, conducted at 5m/s, ARP 1-3ms, prolonged after-polarization Sacroplasmic reticulum – membrane around cell, carries AP, stored Ca2+, involved in metabolism T tubules – part of sarcotubular system, carries AP between the individual fibrils Terminal cisterns – in close contact T tubules near A-I band junction Isometric contraction – same length contraction Isotonic contraction – same force Eccentric contraction – the muscle lengthens as they contract Because work = force x distance isometric does no work (and does negative work if eccentric) Fibrillations – single fiber contraction due to denervation and increased sensitivity to circulating Ach Fasiculations – contractions of a group of fibers due to pathologic discharge of spinal motor neurons Motor unit – a single motor neuron and all the muscle is innervates (will be of the same type) Size principal – recruitment is ordered, S before FR before FF Metabolism: O2 Debt - Anaerobic metabolism allows more work (6x) to be done than could otherwise if completely dependent on O2 delivery - After the period of exertion, the accumulated lactate will be broken down and ATP replenished by increased O2 consumption - If lactate builds too high then enzyme inhibiting pH will develop Also: Creatine (rest/exercise) phophorylcreatine creatinine 2009-2, 2008-2, 2005-1 Describe the sequence of events in contraction and relaxation of skeletal muscle 2008-2, 2007-2 What is summation of contractions 1. The electrical response of a muscle fiber to repeated stimulation 2. Contractile mechanism does not have a refractory period, so repeated stimulation before relaxation has occurred produces additional activation and a response added to the contraction already present 3. With rapidly repeated stimulation, individual responses fuse into one continuous contraction (tetanus; tetanic contraction) 4. Complete tetanus: no relaxation between stimuli; tension developed ~ 4 times that of an individual twitch contraction 5. Incomplete tetanus: periods of incomplete relaxation between summated stimuli Nb: stimulation frequency determined by the twitch duration - so if twitch duration = 10ms, <100/s discrete responses, >100/s will cause summation How does tetanus differ from Treppe 2007-2 Treppe (which means staircase in German) - Series of maximal stimuli at a frequency just below tetanizing -> increasing tension between each twitch - Due to increased Ca2+ availability in sarcoplasm - Cause for the force-frequency relationship in myocardial contractility What are the major differences in types of skeletal muscle 2007-2 - slow and fast, containing a mixture of type I, IIa and IIb - fast fibers may have twitch duration ~7.5ms, for fine, rapid precise movements - slow fibres may have twitch duration up to 100ms, for strong, gross sustained movements Other name Colour Myosin ATPase Ca2+ pumping Diameter Glycolytic Capacity Oxidative Capacity Motor Unit Type I (SO) Slow oxidative red Red Slow Moderate Small Moderate High Slow (S) Type IIa (FOG) Fast oxidative glycolytic Red Type IIb (FG) Fast glycolytic White Fast High Large High Moderate Low Fast fatigue resistant (FR) Fast fatigable (FF) Cardiac muscle RMP -90mV AP – depolarization 2ms, but very long plateau and repolarization 200ms (contraction half over) Intercalcated disks – Connect interdigitated cells for strength Gap junctions - Low resistance bridges for excitation as a syncytium (but no cytoplasmic connection) T tubules are at Z lines (c.f. skeletal at A-I junction) 0 - Rapid depolarization, INa opens, fast Na+ influx 1 - Rapid initial depolarization, INa closes 2 - Plateau phase, Ca2+ influx (slow) 3 - Slow repolarization, IK , K+ efflux (slow) 4 - RMP ARP is thus long – 200ms, and RRP until phase 4 This prevents tetany Smooth muscle 2007-1 Describe the sequence of events in contraction and relaxation of visceral smooth muscle Smooth muscle (vs skeletal) - No striations, instead dense bodies - Tropomyosin, no troponin - Isoforms of actin and myosin are different - Unitary (visceral): large sheets, gap junctions, syncytial (e.g. hollow viscera: intestine, uterus, ureters) - Multiunit: individual units, no gaps, en passant nerve endings to each cell, for fine (non-voluntary) control (e.g. iris of eye) Tone - Maintained in partial state of contraction - No true RMP (-20 to -65mV), higher if active, lower if inhibited Force generation - Despite 20% less myosin and 100 fold less ATP useage… - Can generate as much tension as skeletal m. per cross-section - Contractions are much slower Plasticity - If stretched, initially tension increases - After time it relaxes and tension falls (possibly even below initial) (e.g. the bladder wall w/ increased volume) Contraction of unitary SMCs stimulated by: 1. Stretch muscle causes contraction in the absence of innervation (membrane potential spikes) 2. Cold increases activity 3. ACh decreases smooth muscle potential and increases spike frequency so resulting in more active muscle 4. Adrenaline and noradrenaline increase smooth muscle potential and decrease spike frequency causing decreased muscle activity 5. Neural Synaptic and Junctional Transmission Definitions and Facts EPSP – excitatory post synaptic potential, begins 0.5ms, peaks 11.5ms, declines exponentially, due to openings of Na+ or Ca2+ channels, not enough for generation of a full action potential, but can summate IPSP – the opposite, due to increased Cl- or opening K+ channels or closure Na+ or Ca2+ channels Temporal summation – repeated EPSPs prior to decay Spacial summation – if activity present at more than one synaptic knob - the EPSP is not an “all-or-none” response, but a graded proportional response to the strength of afferent stimulus Occlusion – the sharing of post-synaptic neurons results in a decrease in expected response Slow synaptic potentials – in autonomic ganglia, cardiac m. SMC, cortical neurons, latency 100500ms last several seconds, due to K+ conductance 2010-1, 2006-2 In the synapse where can inhibition occur 1. Post-synaptic (direct due to IPSP, or indirect due to previous post synaptic discharge) - E.g. in the spinal cord the reflex contraction to the agonists at the same time caused inhibition of the antagonists (reciprocal innervation via interposed inhibitory neuron) 2. Pre-synaptic - Via neuron that ends on excitatory endings (axoaxonal synapse) - By 3 mechanisms: i. GABA -> intracellular Cl- -> decreasing AP, of Ca2+ and therefore transmitter release ii. Voltage gated K+ channels -> also decreases Ca2+ entry iii. Direct inhibition independent of Ca2+ Neuromuscluar transmission Neuromuscular junction: endfeet containing vesicles with acetylcholine insert into junctional folds on the motor endplate AP -> increased permeability to Ca2+ -> triggers exocytosis of acetylcholine vesicles -> diffuses to nicotinic receptors -> increased Na+ and K+ conductance -> depolarizing endplate potential The acetylcholine then removed by acetylcholinesterase (high conc in NMJ) Smooth and Cardiac muscle - Multiple branches of noradrenergic (?cholinergic) are beaded with varicosities allowing 1 discharge to innervated many effector cells - Synapse en passant: the neuron make synapses, then passes on to make more synapses – supplying many muscle fibres - EJPs: excitatory junctional potentials are seen by stimulation with the neurotransmitter (noradrenaline or acetylcholine depending on tissue) as discrete potentials (like endplate potentials) and can summate with repeated stimuli - IJPs: the opposite, hyperpolarizing, seen in tissues inhibited by noradrenaline Denervation hypersensitivity - Increased sensitivity to acetylcholine after dennervation - Skeletal m. atrophies also, SMCs don’t, but become hypersensitive to activating mediator - Limited to the structures immediately innervated by destroyed neurons, i.e. supra segmental spinal lesion doesn’t cause hypersensitivity to paralysed skeletal muscle - Multiple causes: upregulation of receptors, and reduction in mediator reuptake