Rapidly Progressive Lethargy and Altered Mental Status: GI Etiology?
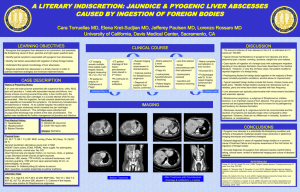
advertisement

Tim Ridgway MD FACP Associate Professor of Medicine University of South Dakota Sanford School of Medicine A 63 year old female presents with increasing lethargy and altered mental status over the previous 2 days. She also complained of nonspecific colicky abdominal pain over the past 3 weeks. On the evening prior to admission, she noted shaking chills. The following day she developed increasing shortness of breath, prompting evaluation locally and transfer to our facility. Hypertension Anxiety Osteoarthritis with predominant knee involvement No surgeries Amlodipine 2.5mg daily Omeprazole 20mg daily (recently started) Temazepam 30mg nightly Diclofenac 75mg bid Paroxetine 40mg daily Quetiapine 100mg nightly Losarten-hydrochlorothiazide 100-25mg daily Admitted to the Intensive Care Unit appearing acutely ill Temp 97.6 RR25 BP 87/63 Pulse 101 Oxygen saturation 70% on room air Lungs: Tachypneic with decreased breath sounds bilaterally without wheezes Cardiac: Hyperdynamic precordium without murmurs. No JVD Abdomen: Nondistended and soft. Bowel sounds present but decreased. No focal tenderness to palpation Neurologic: Disoriented and minimally responsive. No focal neurologic deficit noted WBC 15.7 (90% neutrophils and 24% bands) Hemoglobin 9.8 g/dl Hematocrit 29% AST 67 U/L, ALT 49 U/L Alk Phos 522 U/L, Total bili 3.8 mg/dl ABG: pH 7.3, pCO2 48mm Hg, pO2 65mm Hg Bicarbonate 20 meq/L, Lactate 1.7mmol/L Electrolytes unremarkable Creatinine 1.8 g/dl Progressive respiratory failure requiring endotracheal intubation Progressive neurologic deterioration leading to unresponsiveness Marked hypotension requiring pressor support Broad spectrum antibiotics started after appropriate cultures Abdominal Ultrasound: Contracted gallbladder with wall thickening and pericholecystic inflammatory changes suggestive of cholecystitis. No gallstones or CBD stones seen. CBD 4.2mm diameter CT Chest: Mild pleural effusions bilaterally and bilateral lower lung infiltrates suggestive of bilateral pneumonia CT Head: No focal abnormality noted Gradual clinical improvement leading to weaning of pressors and extubation Streptococcus Intermedius bacteremia Liver abscess developed in area adjacent to pnumobilia-percutaneous drainage performed F/U EGD on 11th hospital day: Severely deformed gastric antrum and deep necrotic ulcer along anterior wall of duodenal bulb Biopsies negative for H. Pylori Biliary stent removed Operative intervention-15th hospital day Fistulous connection between duodenal bulb and left lateral segment of liver (hepatoduodenal fistula) Liver abscess adjacent to gallbladder Left lateral segment abscess/mass Drainage of liver abscess Cholecystectomy Repair of duodenal ulcer/fistula with a Graham patch Open hepatic segmentectomy (segment 3) Liver segment: Liver parenchyma with abscess/fistula tract (containing fecal/vegetable material Left lateral segment mass: Necrotic tissue with acute and chronic inflammation Gallbladder: Mild chronic cholecystitis with adjacent focal abscess formation Bilateral septic emboli to lungs-resolved Respiratory failure-resolved Acute Kidney Injury-resolving Central Nervous System dysfunction-resolved Liver abscesses-resolved Discharge on hospital day 30 IV Vancomycin additional 2 weeks Completed course of Vancomycin Eventual bilateral Total Knee Arthroplasty Full recovery! < 20 cases reported in the medical literature GI bleeding most common presentation Most are diagnosed by histologic exam of endoscopic biopsies or at surgery This is the only known case which presented as sepsis NSAIDS highest risk for perforation and penetration Few cases resolve without surgical management Complications include GI bleeding and hepatic abscess A thick gallbladder wall seen on imaging is a nonspecific finding Chronic NSAID use-BEWARE! Pneumobilia without previous interventionSERIOUS! Sepsis presentation-you have a narrow window of opportunity