HC-MPTs_20May2015
advertisement

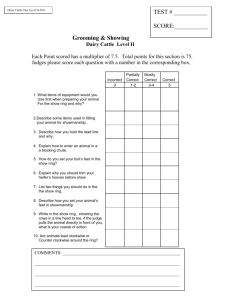
CCTN and MPT Stakeholder Round Table on Hormonal Contraception (HC) in MPTs 20 May 2015 Rockville, Maryland Welcome & Introductions Diana Blithe (NICHD) Bethany Young Holt (CAMI Health) Round Table on HC in MPTs – 20 May 2015 – Rockville, MD MPTs in the Pipeline Drug combinations Drug/Device combinations Multipurpose injectables Bacterial therapeutics Nanoparticles Round Table on HC in MPTs 20 May 2015 – Rockville, MD Initiative for MPTs (IMPT) Contraception Science HIV Prevention Women’s Voices & Access STI Prevention Funder Collaboration Advocacy & Market Development Round Table on HC in MPTs 20 May 2015 – Rockville, MD September 2014 – HC in MPTs Meeting Objectives Unite experts in contraception and MPT development to discuss relevant contraceptive research to help guide MPT development and investment decisions. Inform product developers and supporting agencies about expert recommendations for the use of hormonal contraception (HC) in MPT products. Discuss appropriate strategies for including HC into MPT products between contraceptive experts and MPT developers. Round Table on HC in MPTs 20 May 2015 – Rockville, MD Objectives for the Day Review gaps and challenges identified at the September 2014 HC in MPTs meeting. Review preliminary results of the online HC and MPT prioritization survey. Assess the status of CCTN member MPT research in relation to priorities and gaps. Discuss bleeding patterns and acceptability associated with specific hormone combinations and dosing regimens. Discuss key questions that may help inform successful MPT development and uptake. Round Table on HC in MPTs 20 May 2015 – Rockville, MD IMPT Priority Issues Survey on HC in MPTs Chairs: Diana Blithe (NICHD), Bethany Young Holt (CAMI Health) Discussants: All Round Table on HC in MPTs – 20 May 2015 – Rockville, MD IMPT Priority Issues Survey on HC in MPTs Objective: Review gaps and challenges identified at September 2014 HC in MPTs meeting and prioritize activities for IMPT follow-up. Format – Likert scale ranking: High, Medium, Low, and No Opinion – Are you, or others you are aware of, actively addressing this issues Round Table on HC in MPTs 20 May 2015 – Rockville, MD IMPT Priority Issues for HC in MPTs Q1. Systemic effects: Association of HC plasma levels and anovulation and contraceptive efficacy (57.1%) Q2. Topical effects: Systematic investigation of Mechanisms of Action (MoA) for contraception other than ovulation (57.1%) Q3. Data on HCs other than LNG suitable for MPTs (57.1%) Q4. Contraceptive efficacy in women with high BMI through systemic or topical MOA (14%) Q5. Surrogate markers for effectiveness to determine PK and PD and interaction of HC with other APIs. (57.1%) Q6. Understanding relationship between bleeding and acceptability of HC options (14%) Q7. Role of Cytochrome P450 enzyme for drug metabolism for Pis and NNRTIs. (0%) Q8. Beyond IVRs, development of on-demand and long-acting formulations for MPTs combining HC and ART. (71.4%) Q9. Novel robust acceptability and commercial feasibility measures for key MPT user groups. (57.1%) Q10. Other contraceptive research for the MPT field. (57.1%) HC in MPTs Gaps/Challenges Survey High Priority Areas Q8. Beyond IVRs, development of on-demand and long-acting formulations for MPTs combining HC and ART. Q3. Data on HCs other than LNG suitable for MPTs Q1. Systemic effects: Association of HC plasma levels and anovulation and contraceptive efficacy Round Table on HC in MPTs 20 May 2015 – Rockville, MD HC in MPTs Gaps/Challenges Survey High Priority Areas Q2. Topical effects: Systematic investigation of Mechanisms of Action (MoA) for contraception other than ovulation – protection by: • Cervical mucus • Endometrial thickening, thinning, dilatation • Uterine tubal junction (sperm entry) • Inhibition of sperm function • Other – LNG to date the HC with most data? Q5. Surrogate markers for effectiveness to determine PK and PD and interaction of HC with other APIs. – Pregnancy as main outcome measure historically – To determine PK and PD and interaction with other APIs, new markers and meaningful thresholds needed Round Table on HC in MPTs 20 May 2015 – Rockville, MD HC in MPTs Gaps/Challenges Survey High Priority Areas Q9. Novel robust acceptability and commercial feasibility measures for key MPT user groups. Q10. Other contraceptive research for the MPT field. Round Table on HC in MPTs 20 May 2015 – Rockville, MD HC in MPTs Gaps/Challenges Survey Lower Priority Areas Q4. Contraceptive efficacy in women with high BMI through systemic or topical MOA Q6. Understanding relationship between bleeding and acceptability of HC options – Will discuss further in later session Q7. Role of Cytochrome P450 enzyme for drug metabolism for Pis and NNRTIs. Round Table on HC in MPTs 20 May 2015 – Rockville, MD Status of Ongoing Work Chair: Beatrice Chen (Magee-Womens Research Institute) Discussants: Sharon Achilles (Magee-Womens Research Institute), Annie Thurman (CONRAD), Phil Darney (UCSF) Round Table on HC in MPTs – 20 May 2015 – Rockville, MD Status of Ongoing Work Objective: Assess the status of CCTN member MPT research in relation to identified research priorities and gaps. Round Table on HC in MPTs 20 May 2015 – Rockville, MD Sharon Achilles, MD, PhD UNIVERSITY OF PITTSBURGH Revisiting the IMPT Priority Issues for HC in MPTs Q1. Systemic effects: Association of HC plasma levels and anovulation and contraceptive efficacy Q2. Topical effects: Systematic investigation of Mechanisms of Action (MoA) for contraception other than ovulation Q3. Data on HCs other than LNG suitable for MPTs Q4. Contraceptive efficacy in women with high BMI through systemic or topical MOA Q5. Surrogate markers for effectiveness to determine PK and PD and interaction of HC with other APIs. Q6. Understanding relationship between bleeding and acceptability of HC options Q7. Role of Cytochrome P450 enzyme for drug metabolism for PIs and NNRTIs. Q8. Beyond IVRs, development of on-demand and long-acting formulations for MPTs combining HC and ART. Q9. Novel robust acceptability and commercial feasibility measures for key MPT user groups. Q10. Other contraceptive research for the MPT field. Round Table on HC in MPTs 20 May 2015 – Rockville, MD DRUG-DRUG INTERACTIONS Q7. Role of Cytochrome P450 enzyme for drug metabolism for PIs and NNRTIs. Contraceptive Pharmacokinetics COCs DMPA LNG-IUD ENG-I Vaginal Ring [Serum Progestin] ng/mL 7 6 5 4 3 2 1 Contraceptive efficacy 0 3mo 3yr Achilles, SL. 2014 Background: WHO Antiretroviral Therapy (ART) Recommendations EFV = Efavirenz NVP = Nevirapine CYP3A4 inducers CYP = cytochrome P450 Progestin CYP3A4 Round Table on HC in MPTs 20 May 2015 – Rockville, MD Progestin Studies of Combined use of Contraceptive Implants and NNRTI-based ART 6 cases of pregnancy with combined use of the ENG implant and EFV1 Retrospective chart review of HIV+ women in Swaziland using LNG implant (Jadelle): • 15 (12.4%) of 121 women using EFV-based ART became pregnant (no pregnancies with NVP) Mean time to pregnancy after implant insertion was 16.4 months2 1Matiluko A, et al. J Fam Plann Reprod Health Care. 2007; McCarty EJ, et al. Int J STD AIDS. 2011; Likhi N, et al. J Fam Plann Reprod Heath care. 2010; Leticee N. et al. Contraception. 2011. 2Perry SH, et al. AIDS. 2014. Round Table on HC in MPTs 20 May 2015 – Rockville, MD • PK study of EFV and ritonovirboosted lopinavir (LPV/r) and ENG implant • EFV – decreased ENG AUC by 63.4% • LPV/r – increased ENG AUG by 52.0% LPV/r Control EFV Vieira CS, et al. JAIDS. 2014 Results: PK Study of EFV and LNG Implant Control group (pg/mL) NVP group (pg/mL) Week 1 1003 (702, 1286) 1326 (1073, 1579) 1.32 (1.22, 1.49) 462 (370, 553) 0.46 (0.43, 0.51) Week 4 629 (496, 761) 866 (737, 995) 1.38 (1.31, 1.48) 349 (268, 429) 0.55 (0.54, 0.56) Week 12 547 (433, 661) 758 (656, 860) 1.39 (1.30, 1.52) 326 (268, 286) 0.60 (0.58, 0.62) Week 36 500 (394, 605) 679 (596, 709) 1.36 (1.30, 1.44) 280 (208, 353) 0.56 (0.53, 0.58) Scarsi KK. International AIDS Society. 2015 NVP:Control EFV group EFV:control GM Ratio (pg/mL) GM ratio (90% CI) (90% CI) Unintended Pregnancies with Jadelle 3 pregnancies observed in the EFV group None in the control group or NVP group Pregnancy 1 Pregnancy 2 Pregnancy 3 (pg/mL) (pg/mL) (pg/mL) Over Week 1 the 48 weeks 693 of combined 501LNG-EFV use 185 • LNG were reduced by 45-57% Week 4 concentrations 631 411 201 • LNG AUC was reduced by 48% Week 12 348 363 125 Week 24 297 268 150 Week 36 299 303 122 Scarsi K. CROI. 2015 A Pharmacokinetic Evaluation of the Etonogestrel Implant and Non-Nucleoside Reverse Transcriptase Inhibitor-Based Antiretroviral Therapy in Ugandan Women Catherine Chappell, MD MSc Fellowship in Family Planning Annual Meeting May 3, 2015 HIV+ women desiring an implant Research Design No ART (Control) (13/20 participants) 6 months (ENG) NVP-based ART (20/20 participants) Implant EFV-based ART (17/20 participants) Round Table on HC in MPTs 20 May 2015 – Rockville, MD HORMONE CONCENTRATIONS Q1. Systemic effects: Association of HC plasma levels and anovulation and contraceptive efficacy Q2. Topical effects: Systematic investigation of Mechanisms of Action (MoA) for contraception other than ovulation Q3. Data on HCs other than LNG suitable for MPTs Contraceptive Hormone Induced Changes (CHIC) Two “sister” studies – CHIC-II (Pittsburgh, PA, USA) – Zim CHIC (Harare, Zimbabwe) Evaluation before and after initiation of HC – – – – immune cell populations (systemic and genital) microbiota innate immune factors Contraceptive hormone concentrations in blood and genital tract Round Table on HC in MPTs 20 May 2015 – Rockville, MD Sister Studies Designed to Understand Immunologic, Biomic and Inflammatory Impacts of Contraceptive Use CHIC-II (Pittsburgh, Zim CHIC (Harare, PA) Zim) Funded by NIAID Funded by BMGF (04/2012) (09/2012) US population Sub-Saharan population Low HIV prevalence area High HIV prevalence area Contraceptives: – DMPA (MPA inject) Contraceptives: – – – – – ENG-I (ENG implant) Cu-IUD (IUD-no hormone) COCs (oral LNG+E2) LNG-IUD (LNG IUD) Control (no hormone) Round Table on HC in MPTs 20 May 2015 – Rockville, MD – – – – – – DMPA (MPA inject) ENG-I (ENG implant) Cu-IUD (IUD-no hormone) MPA/E2 (MPA inject+E2) Net-En (norethisterone inject) LNG-I (LNG implant) Study design Prospective parallel cohort studies Given individual variation in endpoints – Normally cycling women without exogenous hormone use are enrolled in follicular phase • baseline samples collected • Initiated on contraceptive – Follow-up visits at 1*, 3, and 6 months • Repeat sample collection at each visit and results compared to baseline to assess individual change • Women serve as own controls to eliminate individual variation *Zim CHIC only Round Table on HC in MPTs 20 May 2015 – Rockville, MD Current Participants by Method As of May 14, 2015 Zim CHIC CHIC II Round Table on HC in MPTs 20 May 2015 – Rockville, MD Serum Hormone Assays Pre-planned serum hormone assessment Collaborative effort with the Small Molecule Biomarker Core to develop liquid chromotography/tandem mass spectrometry (UPLC-MS/MS) assays – Estrogen: estradiol and ethinyl estradiol – Progestogen: progesterone, LNG, ENG, norethindrone, MPA • Panels developed and validated for blood and CVL • Immunoassays are simpler but – cross-reactivity with structurally similar metabolites-> decreased specificity – Inability to measure multiple analytes simultaneously Round Table on HC in MPTs 20 May 2015 – Rockville, MD UPLC/MS/MS for Quantification Advantages – Multiple analytes simultaneously – Highly sensitive and SPECIFIC method – Linearity of calibration curves for more accurate quantification – Good inter-day reproducibility Disadvantages – More expensive than typical immunoassays – More time intensive than immunoassays – Need parent compound and Ideally requires a deuterated (d3 or greater) of the analyte Round Table on HC in MPTs 20 May 2015 – Rockville, MD Plasma Progestin Concentrations 30, 90, and 180 days after Initiation of Use 1500 1000 500 Contraceptive Round Table on HC in MPTs 20 May 2015 – Rockville, MD -I G EN LN G -I N -E et N M PA /E 2 0 D M PA Median pg/mL 2000 More data coming soon… Increased numbers from the Zimbabwe cohorts • Starting soon UPLC/MS/MS testing of Pittsburgh cohorts • • • • • • LNG-based COCs DMPA LNG-IUD ENG-I Vaginal hormone concentrations from Zimbabwe and Pittsburgh cohorts Round Table on HC in MPTs 20 May 2015 – Rockville, MD MTN-030/IPM 041 MTN-IPM RING COLLABORATION Q1. Systemic effects: Association of HC plasma levels and anovulation and contraceptive efficacy Q2. Topical effects: Systematic investigation of Mechanisms of Action (MoA) for contraception other than ovulation Key Product Characteristics • Matrix ring of the same dimensions as the Dapivirine Vaginal Ring • Silicone Polymer: Pt-catalysed (addition-cured) • Developed for 90-days of use • Stable for at least 36 months for SSA environment Slide courtesy of J. Holt Levonorgestrel Dose?? What is the goal? Load of drug in the ring Amount of drug delivered by the ring – Dependent on the load and the in vivo release rate Plasma drug levels achieved Local drug levels achieved Contraceptive efficacy! Round Table on HC in MPTs 20 May 2015 – Rockville, MD Levonorgestrel Dose?? • Multiple components considered o Extrapolation from literature on vaginal PK in women (Landgren ‘85, ’86, ’94; Brache ’07, Sitruk-Ware ‘09,’09; Kives ‘05; Devoto ‘05) o In vitro release rates in high solvent (IPA:water) and “physiologic” (acetate buffer/solutol) conditions o Sheep PK –does not appear predictive for human PK o Limited CHIC data available to date Slide courtesy of J. Holt Effective Levonorgestrel Concentration in Plasma Pharmacokinetic targets derived from literature – Low dose: > 250 pg/mL in plasma – High dose: > 1000 pg/mL in plasma – Steady state in COC users ~2000 pg/mL Round Table on HC in MPTs 20 May 2015 – Rockville, MD MTN-030/IPM 041 PK Study of Vaginal Rings Containing Dapivirine and Levonorgestrel used for 90 days – Dapivirine 200mg ring – Dapivirine 200mg/LNG 32mg ring – Dapivirine 200mg/LNG 320mg ring Randomized 6 women per group (N=18 total) – 3 women of BMI <30 and 3 women of BMI 30-35/group – Sampling: 24h, 48h, 72h, 7d, 14d, 21d, 28d, 60d and 90d Serum & vaginal drug levels What is the lowest acceptable LNG concentration? 200pg/mL? 250pg/mL? Round Table on HC in MPTs 20 May 2015 – Rockville, MD CCTN and MPT Stakeholder Round Table HCs and MPTs Bethesda, MD May 20, 2015 Multipurpose Intravaginal Ring: Tenofovir / Levonorgestrel Andrea Thurman, MD Highlights • CONRAD tenofovir/levonorgestrel ring: – Choice of LNG – Ring design – Preclinical testing – Clinical study design Use of Levonorgestrel • Synthetic progestin used in many contraceptives: Systemic Oral Implant LNG-only LNG + estrogen Daily “mini-pill” 0.03 mg Emergency contraception Daily combined pill Emergency contraception Pericoital pill Norplant Jadelle Sino-Implant Transdermal Genital tract Intrauterine Intravaginal LNG patch LNG + ethinyl estradiol patch Mirena IUS – 20 µg/day Skyla IUS – 14 µg/day LNG ring - 20 µg/day LNG + estradiol ring LNG/carraguard Gel (Bold = commercially available. Others investigational or discontinued) Use of Levonorgestrel • Synthetic progestin used in many contraceptives: Systemic Oral Implant LNG-only LNG + estrogen Daily “mini-pill” Emergency contraception Daily combined pill Emergency contraception Pericoital pill Norplant Jadelle Sino-Implant Transdermal Genital tract Intrauterine Intravaginal LNG patch LNG + ethinyl estradiol patch Mirena IUS – 20 µg/day Skyla IUS – 14 µg/day LNG ring - 20 µg/day LNG + estradiol ring LNG/carraguard Gel (Bold = commercially available. Others investigational or discontinued) Systemic vs genital delivery of LNG • Genital delivery lower plasma levels and higher genital tract levels1 • Distribution beyond endometrium facilitated by large uterine, vaginal arteries anastomoses2 • Genital tract effects from genital delivery may differ from those seen after systemic delivery 1Devoto 2005 Fertil Steril 84(1):46-51 2Lete 2010 Curr Drug Met 11:839-49 Suppression of ovulation Greater chance of irregular bleeding • No development of the ovarian follicle (and therefore no ovulation) • Some follicular development but no ovulation and no increase in progesterone • Follicular development with luteinized unruptured follicle and progesterone production • Normal ovulation Less chance of ovulation • Complete suppression of ovulation not needed for a contraceptive effect. • Alterations in endocrine profile can provide contraception while maintaining normal bleeding patterns: • If ovulation does occur, changes in cervical mucus prevent pregnancy Complete suppression of ovulation not needed for contraception • Mirena: – Mirena: ~50% of cycles are ovulatory in the 1st year, and about 75% in the 4th year, but pregnancy rate is 0.7% over 5 years • Norplant: – 20% of cycles are ovulatory in the 1st year, and 50% in the 5th year, but still contraceptive LNG’s effect on Cervical Mucus • Cervical mucus protects uterine cavity from pathogens; controls sperm migration • Before ovulation: Estrogen secretion and water easier sperm migration • “Quality” assessed via volume, viscosity, spreadability (Spinnbarkeit), crystallization pattern (ferning), and cellularity – Score of ≥ 10 out of 15 considered “good” • Even in ovulatory cycles, LNG thick mucus with poor sperm penetration – Happens quickly: • Norplant: 3 days after insertion, sperm penetration becomes poor despite high estradiol levels1 • Mirena users: Cervical mucus becomes poor in 7 out of 10 one day after insertion, in 10 out of 10 by third day2 – Effect is profound: • In Mirena 20 µg users, no sperm migration despite ovulation3 • LNG 20 µg ring: Inhibition of sperm migration in 92% of post-coital tests4 – Happens at low dose • Seen with lower LNG dose in IUS – Skyla (14 µg)5 1 Dunson 1998 Fertil Steril 69: 258-66 2Natavio 2012 Contraception 87(4):426-31 3Lewis 2010 Contraception 82(6):491-6 4WHO J Steroid Biochem 1979;11(1B): 461-467 5 Apter 2014 Fert Ster 101(6):1656-62 Efficacy of 20 µg LNG ring shown in 2 trials • Efficacy of silicone ring releasing 20 µg/day studied in 1980s: – 90-day ring used for 1 – 2 years – WHO study (n = 1005) • Pregnancy rate at 1 year: 3.5 per 100 women (95% CI 2.2-5.0) – UK study (n = 1591) • Pregnancy rate: – At 1 year: 5.1 per 100 women (95% CI 3.6-6.6) – At 2 years: 6.5 per 100 women (95% CI 4.4-8.6) – Within range of other user-controlled hormonal methods • Suppression of ovulation correlated with irregular bleeding among ring users – # days with bleeding and spotting significantly higher in segments with suppressed ovulation vs normal ovulation1 • Development discontinued until now 1Landgren et al Contraception 1982 26(6): 567-585. The CONRAD TFV/LNG ring: Design challenges • Goal: meet 2 target release profiles not achieved using any other ring platform: – Approximately 10 mg/d TFV for ≥ 90 days – 20 µg/d LNG for ≥ 90 days • Challenges: 1) Release 2 very different drugs • TFV: hydrophilic, poorly released from traditional silicone or EVA rings • LNG: hydrophobic 2) At very different rates • TFV: about 10 milligrams/day • Requires high drug loading (>1 gram TFV in a 4.5 gram ring) • LNG: 20 micrograms/day 3) At a steady rate over time (zero order) for ≥ 90 days The CONRAD TFV/LNG Ring: Solutions • • Developed in collaboration with Patrick Kiser, Northwestern University Polyurethane reservoir rings: – Using commercially available biomedical grade polyurethanes that range from hydrophilic to hydrophobic • Suitable for 2 different drugs using 2 different segments, releasing at 2 different rates: • TFV segment: • Hollow-core reservoir using hydrophilic polyurethane • High loading capacity and rate of release • LNG segment: • Solid-core reservoir using hydrophobic polyurethane • Similar to NuvaRing (EVA) design • Result: tightly controlled steady release for long duration • Suitable for one or more drugs (similar or diverse) Clark et al, PLoS ONE (2014) 9: e88509 The CONRAD TFV/LNG ring: In vitro target release profiles met Clark 2014 PLoS ONE 9(3):e88509 The CONRAD TFV/LNG ring: Animal PK studies, TFV Sheep Pigtail Macaques Vaginal fluid Vaginal fluid Vaginal tissue Vaginal tissue Plasma Plasma Median TFV-DP in macaque vaginal tissue: 1.7-7.4x104 fmol/mg Time-independent TFV release from ring. Median levels similar to gel. Johnson et al, AAC 2012 (56): 6272-83; Moss et al, AAC 2012 (56):5952-5960 Ongoing CONRAD study • First multipurpose ring in clinical trials: – Phase I One-Month Safety, Pharmacokinetic, Pharmacodynamic, and Acceptability Study of Intravaginal Rings Releasing Tenofovir and Levonorgestrel or Tenofovir Alone (Protocol A13-128) • 100 women consented to complete 50 across 2 sites: – Eastern Virginia Medical School, Norfolk, VA: Annie Thurman, PI – Profamilia, Santo Domingo, Dominican Republic: Vivian Brache, PI • 3 treatment groups, randomized 2:2:1 – TFV-only ring (n=20) – TFV/LNG ring (n=20) – Placebo ring (n=10) • About 1 month of 90-day ring use, total 3 months participation • 8 or 9 visits and 1 follow-up contact Objectives • Primary: – Genital and systemic safety • Secondary: – Pharmacokinetics (PK) of LNG and TFV • Tertiary: – Pharmacodynamics (PD) of LNG and TFV – Acceptability Selected entry criteria • Ovulatory baseline cycle (progesterone ≥3 ng/ml) • Protected from pregnancy by one of the following nonhormonal methods: – Sterilization of either partner – Willing to abstain from vaginal intercourse • BMI <30 kg • May not use drugs that affect CYP3A4 Overall study design Screening/ Enrollment Pre-treatment cycle to document ovulation Ring in place After ring removal Relationship of ring days to cycle days Screening/ Enrollment Visit # Ring Day Cycle Day Visit 1 Pre-treatment cycle to document ovulation Visit 2 Visit 3 Ring in place After ring removal Visit 4 Visit 5 Visit 6 Visit 7 Visit 8 Visit 9 Ring insertion (24 hrs after Visit 4) At ovulation* Ring removal (24 hrs after Visit 7) (72 hrs after Visit 7) NA ~ -14 ~ -10 1 2 ~8 ~16-18 ~17-19 ~19-21 Any day 21 24 7 8 ~14 ~22-24 ~23-25 ~25-27 • As determined by ovulation predictor kit. • Expect to see greatest effects of LNG at Visit 6: • Less favorable cervical mucus and poorer sperm migration Safety endpoints Visit # Visit 4 Visit 5 Ring insertion (24 hrs after Visit 4) At ovulation Ring removal 8 2 ~14 ~8 (8-10 days after Visit 6) ~22-24 ~16-18 Cycle Day Ring Day Soluble immune mediators in CVL Microflora Tissue: Histology* Epithelial integrity* Target cell phenotype/activation status Markers of mucosal inflammation (gene expression) Microbial growth on and in returned rings Serum chemistries, CBC, lipids 7 1 Colposcopy AEs * = EVMS only Ring in place Visit 6 Visit 7 After ring removal Visit 8 Visit 9 (24 hrs after Visit 7) (72 hrs after Visit 7) ~23-25 ~17-19 ~25-27 ~19-21 TFV and LNG PK endpoints Visit # Visit 4 Ring insertion Cycle Day Ring Day TFV & LNG in blood TFV in genital fluids (aspirates, swabs) TFV & TFV-DP in tissue LNG in genital fluids (swabs) LNG in cervical mucus Amount of drug in returned rings Ring in place Visit 5 Visit 6 (24 hrs after Visit 4) At ovulation 7 1 8 2 ~14 ~8 (1, 2, 4, & 8 hrs) (1, 2, 4, or 8 hrs) Visit 7 Ring removal (24 hrs after Visit 7) (72 hrs after Visit 7) ~22-24 ~16-18 Also TFV-DP in PBMCs ~23-25 ~17-19 ~25-27 ~19-21 ½ (8-10 days after Visit 6) After ring removal Visit 8 Visit 9 ½ LNG PD endpoints Visit # Cycle Day Ring Day Cervical mucus: quality and sperm migration Blood: estradiol (follicular development) Visit 4 Ring in place Visit 5 Visit 6 Ring insertion (24 hrs after At Visit 4) ovulation 7 1 8 2 ~14 ~8 Visit 7 Ring removal (8-10 days after Visit 6) ~22-24 ~16-18 Blood: progesterone (ovulation) Endometrium: thickness and histology (latter EVMS only) After ring removal Visit 8 Visit 9 (24 hrs after (72 hrs after Visit 7) Visit 7) ~23-25 ~17-19 ~25-27 ~19-21 TFV PD endpoints Ring in place Visit # Visit 4 Ring insertion Visit 5 Visit 6 After ring removal Visit 7 Visit 8 Visit 9 (24 hrs after At Ring removal (24 hrs after (72 hrs after Visit 4) ovulation (8-10 days Visit 7) Visit 7) after Visit 6) Cycle Day 7 8 ~14 ~22-24 ~23-25 ~25-27 Ring Day 1 2 ~8 ~16-18 ~17-19 ~19-21 Anti-HIV & anti-HSV in genital fluid Anti-HIV activity in explants (EVMS only) Study status • As of March 13, 2015: – Participants enrolled: 59 – Participants completed (goal 50): 25 • Interim analysis underway: – To obtain early indication of ring performance: • TFV and LNG PK • LNG PD • TFV PD (explants) – Results expected in mid-May 2015 • Estimated date of last participant visit: January 2016 • Data available Q2 2016 Challenges • Ring design: – Sustained release for 90 days of 2 very different drugs at 2 very different rates, that would meet our preclinical benchmarks • Study design: – Assessing PK and PD of 2 different drugs – Example: Visit 7 (ring removal) – 10 specimens collected (including 5 cervicovaginal biopsies and 1 endometrial biopsy) and sent to 7 labs – Transvaginal ultrasound – Colposcopy – Multiple procedures on removed ring • Regulatory approach: – 2 indications – 2 INDs Acknowledgements A Novel Multi-purpose Technology: ARV and Progestin-eluting Cervical Cap MPT Roundtable, 20 May, 2015, NICHD Philip D. Darney, MD, MSc Distinguished Professor Obstetrics, Gynecology and Reproductive Sciences 67 Global Problem Unintended pregnancies and HIV infection are the leading causes of death in women of reproductive age globally. The contribution of unintended pregnancy to female mortality, along with the devastating consequences of the HIV epidemic to women of reproductive age, urges a convergence in pregnancy and HIV prevention. Drug eluting rings do not protect the cervix to augment HIV and pregnancy prevention Gel microbicide compounds limit compliance Proposed Solution Utilize approved, disposable cervical barrier cap to develop an extended use, discrete, safe, comfortable, women controlled means of contraception and HIV protection Cervical Barrier Cap Annular ring of polymers integrated into proprietary cervical barrier cap for pregnancy prevention and HIV protection. Levonorgestrel and a dual antiretroviral compound, Tenofovir to elude in a controlled, time released manner. UCSF expertise in elution of compounds from polymers incorporated into stents or rings San Francisco General Hospital University of California, San Francisco THANK YOU, philip.darney@ucsf.edu UCSF Bixby Center for Global Reproductive Health Revisiting the IMPT Priority Issues Chairs: Diana Blithe (NICHD), Bethany Young Holt (CAMI Health) Discussants: All Round Table on HC in MPTs – 20 May 2015 – Rockville, MD IMPT Priority Issues for HC in MPTs Q1. Systemic effects: Association of HC plasma levels and anovulation and contraceptive efficacy (57.1%) Q2. Topical effects: Systematic investigation of Mechanisms of Action (MoA) for contraception other than ovulation (57.1%) Q3. Data on HCs other than LNG suitable for MPTs (57.1%) Q4. Contraceptive efficacy in women with high BMI through systemic or topical MOA (14%) Q5. Surrogate markers for effectiveness to determine PK and PD and interaction of HC with other APIs. (57.1%) Q6. Understanding relationship between bleeding and acceptability of HC options (14%) Q7. Role of Cytochrome P450 enzyme for drug metabolism for Pis and NNRTIs. (0%) Q8. Beyond IVRs, development of on-demand and long-acting formulations for MPTs combining HC and ART. (71.4%) Q9. Novel robust acceptability and commercial feasibility measures for key MPT user groups. (57.1%) Q10. Other contraceptive research for the MPT field. (57.1%) Bleeding patterns: Perspectives Relevant to MPT Development Chair: Alicia Christy (NICHD) Discussants: Cynthia Woodsong (IPM), Betsy Tolley (FHI 360), Diana Green Foster (UCSF) Round Table on HC in MPTs – 20 May 2015 – Rockville, MD Bleeding patterns: Perspectives relevant to MPT development Objective: Address biological and social-behavioral questions related to bleeding patterns for HC in MPTs. Round Table on HC in MPTs 20 May 2015 – Rockville, MD Review of Literature Cynthia Woodsong (IPM) Round Table on HC in MPTs – 20 May 2015 – Rockville, MD Relevant Literature Microbicide acceptability & adherence – Clinical trials, hypothetical (non-use) studies Contraceptive preferences & discontinuation Menstrual practices, preferences, beliefs Research methods for collecting data on these topics Round Table on HCs in MPTs 20 May 2015 – Rockville, MD Relevant “social and behavioral” Literature Microbicide acceptability & adherence Cross-cultural Contraceptive preferences & differences discontinuation throughout Menstrual practices, preferences, these issues. beliefs Counseling Research methods for collecting data on these topics Round Table on HCs in MPTs 20 May 2015 – Rockville, MD Microbicide acceptability & adherence Clinical trials & hypothetical (non-use) studies – Non-adherence is common in trials, & frequently due to concerns about side effects Clinical trial participants are required to be using highly effective contraceptive Most data methods; a large number of participants • from subdo not have menses; pregnancies and Saharan Africa method switching may provide relevant & U.S. data Vaginal ring (Africa): most common reason for removal is menses-related (e.g., doesn’t want to wear during menses, wants to clean the ring after menses) Round Table on HCs in MPTs 20 May 2015 – Rockville, MD • focus largely on vaginal gels Contraceptive preferences & discontinuation Highest increase in uptake has been for injectables, but this method also has highest rates of discontinuation Menses disruption is biggest reason for method-related discontinuation Preferences for high contraceptive efficacy may be tempered by tolerance for side effects (use the “least worst” method) Acceptability is positively correlated with adherence Individuals’ perceptions and reactions to their physical responses to contraceptive products are highly variable Round Table on HCs in MPTs 20 May 2015 – Rockville, MD Menstrual practices, preferences, beliefs Cross-cultural differences in views on importance of menses – – – – – Menses is natural/normal/healthy Menses cleanses the uterus/vagina Menses indicates woman is not pregnant Menses is “God’s will” Taboos & contamination beliefs Preferences for menses – Variability in preferences: Menses can be inconvenient, costly, uncomfortable/PMS, male partner issues, etc. Some women prefer to not have menses for these reasons. – African women may be less accepting of amenorrhea Practices for menses management, and sex during menses – vaginal practices during and after menses (includes microbicide trial data); scant data available on sex during menses indicates no/little sex (especially in sub-Saharan Africa) Adolescents – Concerns about “normal,” lack of information/education about menses, schoolgirls’ privacy/hygiene Round Table on HCs in MPTs 20 May 2015 – Rockville, MD Counseling Cochrane review (2014) indicates little clear evidence for best counseling to improve contraceptive adherence – Intensive counseling plus reminders show promise Clinical trial counseling often stresses unknown safety & efficacy of study products, which may affect adherence General consensus is that women need clear information about – what to expect for bleeding disruptions – duration of bleeding effects and long-term effects – reproductive system basics Round Table on HCs in MPTs 20 May 2015 – Rockville, MD Research methods Settings: clinical trials, service delivery, general population – impact findings Definitions/measurement of bleeding – menses, spotting, “normal,” time periods, volume – self-report in interviews, diaries Quantitative – Scales & Questionnaires (e.g., Menstrual Attitudes Q., Menstrual Experiences and Behaviors Q., Menstrual Education and Preparedness Q.) Qualitative – Interviews, Focus groups, photo-voice, body imaging, etc. Mixed methods Translation issues (slang, metaphors, etc.) Social desirability bias Round Table on HCs in MPTs 20 May 2015 – Rockville, MD Factors impacting acceptability research gaps Diana Foster Greene (UCSF) Round Table on HCs in MPTs – 20 May 2015 – Rockville, MD Features of contraceptive methods Stopping the method I can stop using the method at any time. I can get pregnant immediately after I stop using it. Using the method The method is easy to use. I don’t have to remember to use the method each time I have sex. I use the method only when I have sex. Getting the method The method is easy for me to get. The method is affordable. I can get the method without seeing a doctor or going to a clinic. Side effects and health concerns The method has few or no side effects. The method doesn’t detract from my sexual enjoyment. The method doesn’t detract from my partner’s sexual enjoyment. The method has a health benefit. The method protects against STI’s. The method does not change my menstrual periods. The method is very effective at preventing pregnancy. Control and Privacy I am responsible for using the method and not my partner. I have control over when and whether to use method. No one can tell that I’m using the method. Round Table on HC in MPTs 20 May 2015 – Rockville, MD Percentage of women saying this feature is very Contraceptive important Features The method is very effective at preventing pregnancy. The method has few or no side effects. The method is affordable The method is easy for me to get. The method is easy to use. I have control over when and whether to use method. I am responsible for using the method and not my partner. I don’t have to remember to use the method each time I have sex. The method doesn’t detract from my sexual enjoyment. The method doesn’t detract from my partner’s sexual enjoyment. The method protects against STI’s. No one can tell that I’m using the method. The method has a health benefit. The method does not change my menstrual periods. I can stop using the method at any time. I can get pregnant immediately after I stop using it. I can get the method without seeing a doctor or going to a clinic. I use the method only when I have sex. total 85% 79% 77% 76% 74% 71% 70% 66% 65% 62% 62% 58% 57% 52% 51% 51% 44% 36% UI likely in > 3 UI in next three previous 3 months months 71% 70% 61% 63% 63% 73% 56% 54% 54% Percent of features matched: Once and future MOC no method over the counter pill over the counter pericoital pill ring sponge EC pericoital pill diaphragm patch self removable IUD pills IUD shot implant steriliz ation condom withdrawal 71% 71% 68% 67% 67% 66% 64% 63% 62% 61% 60% 56% 51% 51% 51% 49% 37% Round Table on HC in MPTs 20 May 2015 – Rockville, MD For 90% of women there is no contraceptive method that has all the features they think are “extremely important” Strategies to increase acceptability of bleeding patterns for MPTs Betsy Tolley (FHI 360) Round Table on HCs in MPTs – 20 May 2015 – Rockville, MD Overview Strategies to increase acceptability of bleeding patterns for MPTs – Clinic Level Strategies – Shaping Preferences Research Gaps Round Table on HCs in MPTs 20 May 2015 – Rockville, MD Provider-Client Disconnect Providers Prescribe methods that fit perceptions of client needs & abilities Focus on medical info on SEs versus experience of SEs – Amenorrhea reduces anemia – Break-through bleeding is not menses May provide inaccurate or incomplete information about method-related menstrual SEs Some hold similar misperceptions about menstrual SEs Clients Have little understanding of how methods would fit their needs Have misperceptions – Non-pregnancy amenorrhea unhealthy, linked to infertility or cancer or vaginal dryness Worry about “clusters” of SEs – Long RTF explained by too little or too much bleeding, other SEs Round Table on HCs in MPTs 20 May 2015 – Rockville, MD Focus on how SEs impact lifestyle, rather than medical info – Prolonged spotting disrupts normal routines Counseling Strategies Structured information about DMPA, including information on hormonal effects, shown to increase continuation and effectiveness compared to routine counseling – De Cetina 2001 (350 Mexican women randomly assigned to structured versus routine) – Halpern Cochrane Review Women in OC RCT evaluating continuous versus cyclic use preferred the method they were randomized to use. Counseling should: – Identify and address user questions and concerns – Describe the range of possible menstrual (and other) changes – Consider how bleeding and other SEs will influence women’s lifestyles and relationships Round Table on HCs in MPTs 20 May 2015 – Rockville, MD Management of Menstrual Changes Waiting for women to return to the clinic may be too late – Egypt study, DMPA users with concerns about their method reported seeing private doctors, rather than returning to the FP clinic Simply-worded but detailed information about side effects may be sufficient Simple treatments for some hormonal side effects may ease concerns – COCs and estrogen-only treatments – Non-steroidal anti-inflammatory drugs (NSAIDS) Over-the-counter products to manage bleeding like menstrual pads may help (but not always accessible) Other methods to verify non-pregnancy when amenorrheic Round Table on HCs in MPTs 20 May 2015 – Rockville, MD Shaping Preferences Persuasive messages have a specific behavioral objective and are tailored to needs and concerns of a specific audience – Message must be salient to target group – Channels for information dissemination will also vary – Using multiple channels and targeting primary audiences and those who influence them increases effectiveness Messages – Amenorrhea acceptable during pregnancy and expected after menopause, but how to communicate its health benefits during other life stages? – How to delink amenorrhea from infertility?* – How to communicate about patterns that change over time? Channels – Mobile phones and social media – Mass media formats – Interpersonal communications How to target men? Round Table on HCs in MPTs 20 May 2015 – Rockville, MD Research Gaps Understanding how to best counsel about menstrual changes related to different methods: – i.e., What is the relative effect of providing “structured information” on menstrual effects versus “client-centered questions” on method continuation? Determining how to best support management of menstrual side effects: counseling vs medical treatment vs other management Identifying best channels and messages to enhance/shape provider and user acceptability of method-included menstrual changes – These will vary by audience (age, lifestyle and stage of life, geographic setting, method) Round Table on HCs in MPTs 20 May 2015 – Rockville, MD MPT Stakeholder Questions & Discussion Chair: Joe Romano (NWJ Group/ IMPT Senior Scientific Advisor) Discussants: Jim Turpin (NIAID), other Round Table on HC in MPTs – 20 May 2015 – Rockville, MD MPT Stakeholder Questions & Discussion Objectives: – Provide overview of DAIDS research program to members of the CCTN – Obtain input from CCTN members on HC and MPT relevant questions from MPT Stakeholders (funders, product developers) Round Table on HC in MPTs 20 May 2015 – Rockville, MD CCTN and MPT Stakeholder Roundtable on HCs and MPTs Jim A. Turpin, Ph.D., Chief Preclinical Microbicides and Prevention Research Branch (PMPRB) Prevention Sciences Program Division of AIDS NIAID/NIH May 20, 2015 Purpose of Presentation Provide an overview of PMPRB’s research portfolio involving hormonal contraceptives Agenda: 1. Rationale for and focus of PMPRB’s portfolio involving hormonal contraceptives 2. Summary of funded grants---No data since ongoing grants The views expressed are those of the presenter and do not necessarily reflect the official policies of the Department of Health and Human Services (HHS), nor does mention of trade names, commercial practices, or organizations imply endorsement by the U.S. Government PMPRB’s Focus Charged with preclinical discovery, development and early clinical testing of non-vaccine biomedical prevention strategies: topical microbicides, topical and systemic PrEP and MPTs. PMPRB Approach Objective: Development of a sustainable and effective non-vaccine biomedical prevention pipeline of strategies (topical microbicides, topical and systemic PrEP and MPTs). The Problem: Achieving the Objective requires not only drug development, but also an understanding of the complexity of the male and female genital and GI tract physiology and biology, and how these factors impact susceptibility to HIV infection, and safety and efficacy of the prevention products and their delivery vehicles. Critical Question: What are the effects of endogenous and exogenous factors on HIV susceptibility, and what product/strategy adjustments are needed to sustain the safety and efficacy of clinically successful prevention strategies following licensure? HIV Susceptibility HIV susceptibility is controlled by multiple factors which in aggregate determine the overall degree of susceptibility to infection Defining the HIV Infection Susceptibility Gap Development of effective and safe global use prevention strategies must be informed by the biology and physiology of the male and female genital and GI tracts. 1. Role of the life cycle in HIV susceptibility. How does age and maturation of the genital and GI system and tissues influence HIV susceptibility? 2. Role of the immune system and inflammation in HIV susceptibility. How do the adaptive and innate immune systems control resistance and susceptibility to HIV infection? 3. Role of the microbiome and its impact on HIV susceptibility. What is the role of the microbiome in product safety and efficacy? 4. Role of genital secretions and hormones (endogenous and exogenous) in HIV susceptibility. What is the relationship between endogenous and exogenous factors expression and the safety and efficacy of prevention products and their delivery systems? 5. Role of tissue responses to prevention agents and their vehicles on HIV susceptibility. How do drug and vehicle alterations in target cell homing, activation, inflammation, innate and adaptive immunity and drug PK/PD/metabolism control susceptibility to infection during use of a prevention strategy? Mapping Program Objective: Map mucosal function and responses in the context of HIV -1 prevention. Funding Mechanism DAIDS Awards/ Projected Awards 6 of 9 DAIDS Awards to New Investigators * NICHD: Prevention of HIV Transmission/Acquisition through a better understanding of Reproductive Health Integration of the Mapping Program into the Non-vaccine Biomedical Prevention Program Prevention of HIV Transmission/Acquisition through a better understanding of Reproductive Health (DAIDS Funded) • CHIC II:Effect of COCs, DMPA, LNG-IUD and Cu-IUD on immune cell activation and the microbiome in the cervicovagina and endometrium in U.S. Women. Companion study in Zimbabwe (Zim CHIC) funded by Bill and Melinda Gates Foundation • Exploration of the cellular and hormonal factors controlling the susceptibility to HIV infection during the menstrual cycle. “Window of Vulnerability” hypothesis posits that HIV susceptibility is controlled by endogenous hormone expression in the female reproductive tract (FRT). • Relationship of medroxyprogesterone, levonorgestestrel and ectonorgestrel serum/tissue concentrations to HIV target cell numbers, phenotype and innate immune factor expression in ecto-, endocervical and rectosigmoid mucosa. (ex vivo studies) Prevention of HIV Transmission/Acquisition through a better understanding of Reproductive Health (DAIDS Funded) Cont. • Impact of DMPA on TDF/FTC concentrations in vaginal and cervical tissues. Targets drug transporters and nucleotide phosphorylation and metabolism in CD4+T cells. • Longitudinal study of the impact of Depo-Provera on cervicovaginal and colonic microbiomes and the systemic and mucosal immune system. Uses ex vivo determinations of HIV susceptibility. • Hypothesizes that the type of progestin and its local concentration are important in determining the susceptibility of the tissue to HIV infection. Compares the effect of the DMPA and LNG (IUD) on a number of immune and cellular markers, including transport of HIV in mucus and in vitro anti-HIV activity of secretions. Mucosal Environment and HIV Prevention (MEHP) • Uses additional analysis of Partners in PrEP samples to correlate DMPA use, BV presence and HIV infection (+/- PrEP). • Characterize the relationship between immune activation and the FRT biome (viral, fungal, archeal and bacterial communities, weekly for 2 years) in highrisk women in sub-Saharan Africa in the FRESH trial. Quantitates systemic progesterone, estradiol, and medroxyprogesterone acetate (~20% Women on DMPA) in plasma and cervicovaginal secretions (LC-MS). • Assessment of the endocervical inflammatory effects of Intrauterine devices (Cu-IUD, Mirena, LNG-IUD vs. oral LNG users). Focused on determining HC effects on immune cell activation and pro-inflammatory programmed cell death (Pyroptosis) of HIV target cells. Other Activities of interest • Reengineering the Cu-IUD to delivery an ARV • Interaction of hormonal contraceptives and Tenofovir (TFV), and Tenofovir Alafenamide (TAF) in HIV target cells in the upper and lower female reproductive tract (FRT). In vivo and ex vivo effect of hormones on drug metabolizing enzymes (NRTI activating and degrading), and innate immune signaling/mediator expression • Virus/cervical mucous interactions. Discussion Questions: HC and HIV Risk Is the link between specific HC-receptor binding and induction of inflammation adequately understood to assess HIV risk? Are the receptor binding profiles between different HC options adequately characterized and understood? Is there evidence of specific HC suppression or activation of the adaptive or innate immune systems? What is known about the effects of hormones on immune cell trafficking in the FRT? Are “normal” endogenous hormone (P, E, LH, FSH) levels adequately understood to serve as markers for HIV infection vulnerability? Round Table on HC in MPTs 20 May 2015 – Rockville, MD Discussion Questions: HC Dose Can animal models be used to define topical or systemic HC dose levels for contraceptive efficacy in an MPT? Is a single topical dose of HC viable to accommodate any BMI? – Will BMI variability likely dictate the need for MPT with multiple HC doses? Round Table on HC in MPTs 20 May 2015 – Rockville, MD Discussion Questions: Topical Effects & DDI Topical Effects: What is the relevance of systemic vs local FRT tissue levels of HC on mechanism of action and contraceptive efficacy DDI HC and cellular uptake, activation, egress of ARVs? – HC and induction/suppression of cellular transporters? – HC induction of nucleotide pools and metabolism? Round Table on HC in MPTs 20 May 2015 – Rockville, MD Discussion Questions: General Considerations/Risks Can pairing ARVs with HC in an MPT negatively effect end user perception of the product for contraception? What are the major risks associated with MPT implementation/delivery from the FP perspective? What are the major biological issues/risks with the combination of HC with ARV? Are there specific HC options that currently make more sense than others for an MPT? Round Table on HC in MPTs 20 May 2015 – Rockville, MD Concluding Question “Adding an ARV for HIV prevention to an established contraceptive method will boost uptake and sustained use of an HIV prevention intervention” Is this hypothesis sufficiently reasonable to justify MPT development investment? If yes, what are the priority issues to be addressed first? If not, what unknowns must be addressed to achieve justification? Round Table on HC in MPTs 20 May 2015 – Rockville, MD Bridging the silos between contraception & HIV prevention Round Table on HC in MPTs 20 May 2015 – Rockville, MD Acknowledgments Bill & Melinda Gates Foundation Mary Wohlford Foundation NIH NICHD USAID Round Table on HC in MPTs 20 May 2015 – Rockville, MD The Initiative for Multipurpose Prevention Technologies Round Table on HC in MPTs 20 May 2015 – Rockville, MD Thank You! Support for this project is made possible by the generous support of the American people through the United States Agency for International Development (USAID) under the terms of the HealthTech Cooperative Agreement #AID-OAA-A-11-00051, managed by PATH. The contents are the responsibility of CAMI/PHI and its partners and do not necessarily reflect the views of USAID or the US Government. Round Table on HC in MPTs 20 May 2015 – Rockville, MD