ppt of male systems slides
advertisement

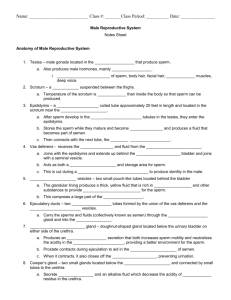
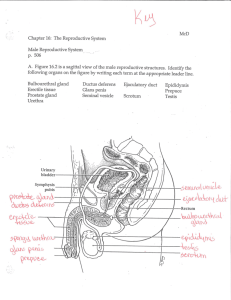
Anatomy and Physiology of the Male Topics • • • • • Anatomy Physiology Spermatogenesis Hormonal regulation Development Anatomy • • • • Scrotum Testes Penis Glands Scrotum • Maintains 34°C (93.2°F) • Dartos muscle – wrinkles the skin • Cremaster muscles – draw scrotum toward abdomen Testes • Coverings • Tunica vaginalis • Tunica albuginea • Lobules • Seminiferous tubules • Tubulus rectus • Rete testis • Epididymis Testes Blood Supply • Countercurrent heat exchange • Testicular artery • Pampiniform venous plexus Testes Blood Supply • Varicocele • Varicose vein like condition • 15-20% of males • 40% of infertile males Penis external anatomy • Foreskin • 60% in US are circumcised • 15% worldwide • Shaft • Glans penis Penis internal anatomy • Corpus spongiosum • Bulb of penis • Corpora cavernosum • Crura of the penis Male Duct System • Epididymus • 20 feet! • 20 days for sperm to mature • Smooth muscles expel sperm during ejaculation • Cells have Male Duct System • Epididymus • Smooth muscles expel sperm during ejaculation • Cells have microvilli Male Duct System • Ductus (vas) deferens • 18” • Very muscular • Ampulla Male Duct System • Vasectomy • Almost 100% effective • Reversal about 50% success rate Male Duct System • Ejaculatory duct • Urethra • Conveys both urine and semen • Prostatic • Membranous • Penile • Urethral glands secrete mucus prior to ejaculation • Seminal vesicles • Size of little finger • Surrounded by smooth muscle • Seminal fluid • Fructose • Ascorbic acid • Coagulating enzyme • Prostaglandins • Other factors that enhance Glands • Prostate • Size of peach pit • Several ducts into the prostatic urethra • Surrounded by smooth muscle • Secretions • Citrate • Enzymes (fibrinolysin, hyaluronidase, acid phosphatase) • Prostate specific antigen (PSA) • activate sperm Glands Glands • Bulbourethral glands • Pea sized • Mucus • Lubrication • Neutralizes acidic urine prior to ejaculation Semen • 2-5ml • Composed of • Sperm (10%) • Testicular fluid • Gland secretions • Functions • • • • • • • • • Semen Transport, activation and protective medium Nutrients for sperm (fructose) Neutralizes vaginal tract Prostaglandins reduce viscosity of mucus at cervix Enzymes enhance motility Antibiotics Chemicals that suppress the female immune system Clotting factors that coagulate semen so it sticks to vagina Fibrinolysin then dissolves that mass Physiology • Erection • NO (nitric oxide) released (in penis tissue) • Causes arterioles (normally constricted) to relax/dilate • Blood flows into the corpora cavernosa • Compresses veins to prevent flow out • Corpus spongiosum also expands but maintains open urethra • Bulbourethral glands secrete lubricant Physiology • Ejaculation • Spinal reflex • Bladder sphincter muscle constricts • Reproductive ducts and glands contract • Contents enter urethra • Muscles around the blub of penis – series of rapid contractions • Other systemic changes • Rapid heartbeat • Elevated blood pressure • Generalized muscle contraction Erectile dysfunction • Deficient NO release • Viagara, Cialis and Levitra increase effects of NO • Possible factors • Psychological factors • Alcohol or drugs • Antihypertensives, Antidepressants • • • • Diabetes mellitus Arteriosclerosis Varicose veins Nervous system issues Spermatogenesis Spermatogenesis • Meiosis • Sertoli cells • Nourish and “clean” • Secrete testicular fluid • androgens • Tight junction • Blood-testis barrier • prevents sperm antigens from the immune Spermatogenesis Spermatogenesis • Spermatogenic cell • 64-72 days Infertility • 1/7 of Americans; most due to sperm issues • Estrogen-like compounds • Antibiotics (tetracycline) • Compounds that lead to abnormal sperm • Radiation, marijuana, lack of selenium, alcohol • Lack of a specific Ca++ channel (for motility) • Anatomical obstruction • Hormonal imbalance Hormonal Regulation • HypothalamicPituitary-Gonadal Axis • Hypothalamus • Anterior pituitary • Testes Hypothalamic-Pituitary-Gonadal Axis • Hypothalamus • GnRH – gonadotropin releasing hormone • Stimulates the anterior pituitary Hypothalamic-Pituitary-Gonadal Axis • Anterior Pituitary • LH – luteinizing hormone • Released in response to GnRH • Stimulates interstitial cells (Leydig cells) to secrete testosterone Hypothalamic-Pituitary-Gonadal Axis • Anterior Pituitary • FSH – follicle stimulating hormone • Released in response to GnRH • Stimulates Sertoli cells • ABP – androgenbinding protein: Keeps concentration of testosterone high Hypothalamic-Pituitary-Gonadal Axis • Testosterone • meiosis of spermatogenic cells • development and maintenance of secondary sex characteristics • Libido • Feed back to pituitary and hypothalamus Hypothalamic-Pituitary-Gonadal Axis • Inhibin • Secreted by Sertoli cells • produced in response to sperm count • Inhibits release of GnRH and FSH Hypothalamic-Pituitary-Gonadal Axis • Absence of GnRH, FSH and LH • Testicular atrophy • Accessory organs atrophy • Testosterone production declines (or ceases) Secondary sex characteristics • • • • • • • • • Pubic and axillary hair Facial and chest hair Larynx enlarges Skin thickens and becomes oilier Bones grow and increase density Skeletal muscle increases Basal metabolic rate increases Development of libido Brain development Reproductive System Development 5 weeks •gonadal ridges •Mullerian ducts – female •Wolffian duct – male Germ cells migrate to gonad Reproductive System Development 7 weeks – ductus deferens forms •Seminiferous tubules form in gonadal ridges •Join the Wolffian ducts •Testes secrete MIF – Mullerian Inhibitory factor •Mullerian ducts degenerate Reproductive System Development 8 weeks – presence of testosterone •Genital tubercle enlarges • forms penis •Urethral folds fuse • Forms spongy urethra •Labioscrotal swellings fuse • Form scrotum Reproductive System Development • • Gubernaculum (G) (blue) – connects testis to floor of scrotum • At 7 months G stops growing and becomes fibrous • Rapid growth of fetus causes G to pull testis into the scrotum