Chapter 26
advertisement

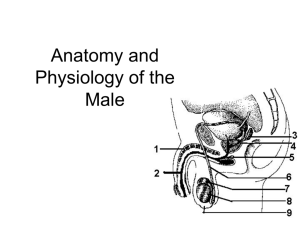
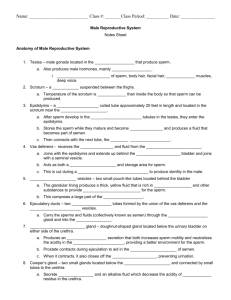
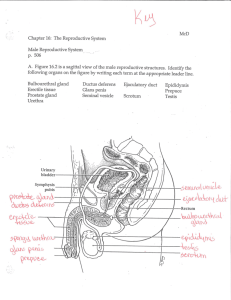
Chapter 26 Male reproductive system Primary & secondary sex organs Testes are the primary sex organ of the male reproductive system. They manufacture and store spermatozoa for fertilization of ova and reproduction of the species. Produce the sex cells or gametes = spermatozoa in males Produce testosterone Secondary or accessory sex organs include: – The scrotum, epididymis, ductus (vas) deferens, urethra, ejaculatory duct, prostate gland, bulbourethral gland, seminal vesicles, and penis. Male reproductive organs Scrotum Divided pouch of skin that contains the testes and is suspended outside of the body where it keeps the temp ~ 3.5 degrees cooler and prevents the sperm from dying. Covered with stratified squamous epithelium and sparse pubic hairs it is divided in the middle by a septum that separates the two testicles. Externally the septum is marked by a seam the perineal raphe which extends from the inferior surface of the penis, around the scrotum to the margin of the anus. In cold weather the scrotum can retract by contraction of the cremaster muscle (sk.m.) to bring the testicles up closer to the body for warmth. The cremaster muscle is an extension of the ext. oblique muscles. The dartos muscle, a thin layer of smooth muscle in the superficial fascia, causes the scrotum to wrinkle and thicken the skin in order to preserve heat in the cold, as well. Scrotum The scrotum is richly supplied by many sensory and motor nerve fibers It is also highly vascularized by the testicular artery to provide nourishment and oxygen to the spermatogenic apparatus necessary for production of sperm. The pampiniform plexus is a network of veins that surround the testicular artery and serve as a heat exchanger to cool the blood in the testicular artery and allow for production of live sperm. Testes Testes Location: Contained within the scrotum inferior and outside of the abdominal cavity at the root of and posterior to the penis. Structure: Enclosed in a serous sac tunica vaginalis from peritoneum tunica albuginea “white coat”, fibrous outer capsule of the testes. Septal extensions of the t. albuginea form 200-300 lobules. lobules – compartments; contain 1-4 seminiferous tubules seminiferous tubules – tightly coiled “sperm factories” lined with germinal epithelium and sustentacular or Sertoli cells. The “S” cells protect the germinal epithelium and form a blood-testes-barrier to prevent the immune system antibodies from attacking the sperm septum – divides testis into numerous wedge shaped compartments that arise from tunica albuginea. Interstitial cells (Cells of Leydig) – produce androgenic hormones (testosterone, etc.); sourround seminiferous tubules and secrete fluid into surrounding interstitial fluid. Testes SEM of seminiferous tubules Spermatic ducts Consists of those ducts that carry sperm from the seminiferous tubules in testes → urethra. Includes the rete testis, efferent ductules, epididymis, ductus (vas) deferens and ejaculatory duct. Rete testes network of vessels off of seminifeous tubules and lead into head of epididymis. Efferent ductules are 12 small ducts that carry sperm from the seminiferous tubules to the epididymis. They are lined with clusters of ciliated cells that help the sperm move along. Epididymis Coiled tube ~ 20 feet long on posterior surface of testicles. Serve as storage sites and place of maturation of the sperm produced in the seminiferous tubules. Has a head, body and tail and is lined with pseudostratified columnar epithelium covered with stereocilia. Upon entering the epididymis it may take up to 20 days for sperm to mature and become motile and capable of fertilizing an ova. Sperm are stored in the epididymis for 20 days before they are phagocytized and destroyed by surrounding epithelial cells. At the time of ejaculation, the sperm are expelled from the tail of the epididymis into the ductus deferens. Sperm do not begin swimming until ejaculated into the vagina. They are expelled from the sperm ducts by intense peristaltic contractions. Ductus (vas) deferens Thick muscular tube that extends from tail of epididymis to the ejaculatory duct. ~ 45 cm long and 2.5 mm in diameter. Runs superiorly through the inguinal canal and spermatic cord up the anterior wall of pelvic cavity over and behind the urinary bladder and turns anteriorly to join the duct of the seminal vesicles which form the ejaculatory duct. Propels sperm from epididymis to ejaculatory duct by peristaltic contractions. Lined with pseudostratified columnar epithelium. Ampulla Seminal vesicle Ductus deferens Epididymis Glans of penis Prepuce Testis Scrotum Ejaculatory duct Prostate gland Bulbourethral gland Rectum Ejaculatory duct A short segment of spermatic duct system the ejaculatory duct is formed by the convergence of the ductus deferens and seminal vesicle duct. It is ~ 2 cm long and passes into the prostate gland where it empties into the urethra. Accessory glands of male reproductive system Includes three sets of accessory glands: – The seminal vesicles – The prostate gland – The bulbourethral (Cowper) glands Seminal vesicles Paired glands ~ 5 cm long and dorsal to the urinary bladder. Internally they are a complex labyrinth of ducts Produce a yellowish secretion that is ~ 60% of the semen volume. Prostate gland A bulbous gland situated at the base of the urinary bladder and consists of smooth muscle and connective tissue. Composed of 30-50 tubuloacinar glands that empty into the urethra. Milky secretion is ~ 30% of ejaculate volume. Bulbourethral gland Two brownish spherical glands ~ 1 cm diameter. They are located just superior to the bulb of the penis and their duct empties into the penile urethra. Their secretion neutralizes the residual acidic urine in the urethra and serves as a pre-ejaculate to lubricate the penis for easy insertion into the vagina. Semen Is a complex mixture of sperm and glandular secretions released upon ejaculation. Typical volume is ~ 2 to 5 ml/ ejaculate. Sperm count is 50 to 120 million/ ml. of semen. It consists of: – ~ 10% spermatozoa – 30% prostatic fluids – 60% seminal fluids – High in fructose and enzymes to neutralize vaginal secretions and bacteria. Spermatozoa Three distinct regions: 1) head, 2) mid piece and 3) tail. – Head is a flattened oval containing chromosomes. Tip contains Acrosomal cap with enzymes that will aid in penetration of the ova membrane. – Mid piece is joined to head by a short neck and contains centrioles and mitochondria. – Tail is a flagellum that propels the spermatozoa through the female reproductive tract. Spermatozoa Urethra Consists of three regions in males – Prostatic urethra – Membranous urethra – Penile “spongy” urethra Penis Tubular organ that empties urine through the distal urethra and introduces semen into the vagina during sexual intercourse. Internal half is the root and external half is a shaft and glans. Together the penis and scrotum constitute the external genitalia of males. The skin of the penis is loose and slides distally over the glans to form a “foreskin” or prepuce. Internally the penis consists of 3 long cylindrical bodies of erectile tissue. These erectile bodies fill with blood during arousal and engorge the penis creating an erection. The erectile bodies are: a single corpus spongiosum, a paired corpus cavernosa (dorsally). Penile structure Root = bulb + crus Shaft = body + glans Erectile tissue: Corpus cavernosa Corpus spongiosum Vascular supply: Internal pudendal art. Nerve supply: Parasym. → erection Sym. → ejaculation Urinary bladder Ureter Ampulla Seminal vesicle Ejaculatory duct Prostate gland Bulbourethral gland Bulb Crus Ductus deferens Corpus cavernosum Corpus spongiosum Epididymis Testis Urethra Glans of penis Penis Chapter 26 Female reproductive system Primary sex organ Ovaries suspended in the retroperitoneal abdominal cavity, superior and lateral to the uterus. They contain the ova for reproduction of the species. They are somewhat almond shaped and are ~3 cm ↑, 1.5 cm → and 1 cm thick. Each ovary contains 6 – 7 million ova and only a single ova is released at the time of ovulation. Female reproductive system Primary and secondary female sex organs Ovaries are the primary female sex organs that manufacture and release a single ova for fertilization with each ovarian cycle. Secondary accessory sex organs include: – The mons pubis, labia minora, labia majora, clitoris, vagina, cervix, uterus, fallopian tubes, fimbria and mammary glands. Ovary Structure: Tunica albuginea – fibrous outer covering on ovary. Cortex – outer layer of ovary where the oocytes reside in primordial follicles “little bags” before maturation. Follicles – tiny scale-like structures that contain the ova. (Graafian or vesicular follicle) – a mature follicle that bulges out onto the surface of the ovary just prior to ovulation (release of the ova). Only 1 ova is released. Corpus luteum – luteal body left after ovulation. Medulla – inner connective tissue core of the ovary, contains blood vessels and nerves. Ovary Ovary Ligaments– ovarian ligament anchors ovary to uterus; suspensory ligament anchors ovary to pelvic wall; mesovarium ligament suspends ovary in between uterus and fallopian tubes. Both suspensory and mesovarium form broad ligament which tents over the uterus and supports the uterine tubes, uterus and vagina. It receives its vascular supply from the ovarian artery and the ovarian branch of the uterine artery. Function of ovary: – a. To produce ova for fertilization – b. Produce estrogen and progesterone Internal female reproductive organs Uterine or Fallopian tubes Consist of fimbriae, infindibulum, ampullae, and isthmus. Fimbriae are finger like ciliated projections at proximal end of infindibulum. They have a wave-like motion to sweep the ova toward the infindibulum. The infindibulum is lined with cilia. At the time of ovulation the cilia beat toward the opening into the fallopian tube pulling the free ova inward, moving it along by peristaltic contractions into the ampullae. Uterine or Fallopian tubes Fertilization of the ova occurs in the ampullae near the infindibulum. The fallopian tubes are made of smooth muscle and are lined with ciliated columnar epithelium and are supported by a short mesentery called the mesosalpinx, a part of the broad ligament. Colorized SEM of fallopian tubes Ovaries, fallopian tubes and uterus Uterus Is a thick muscular organ where implantation of the fertilized ovum occurs for development of the embryo into a fetus. Location – within retroperitoneal pelvic cavity, covered by visceral peritoneum. Structure –looks like an inverted pear Consists of a fundus, body and cervix. – Fundus is the dome of the uterus – Body is the main portion – Cervix is a thick circular muscular ring that opens into the vagina Uterine wall layers and blood supply Layers of the uterine wall include: – endometrium – mucosal layer of simple columnar epithelium with secretory cells and ciliated cells underlain by a thick lamina propria. – Two stratum makeup the lamina propria: Functionalis is highly vascular and under ovarian hormonal control. It is shed at menstruation if an ovum is not implanted. Basalis forms a new functionalis layer after menstruation. – myometrium – thick muscular layer of interlacing bands of smooth muscle. – perimetrium – outer most serous layer = visceral peritoneum Uterine wall layers and blood supply Uterus Vagina Hollow thin walled tube that receives the penis during sexual intercourse and serves as the birth canal at the time of partuition (birth). Inferior to the uterus, the cervix opens into the vagina. Area of the vagina that encircles the cervix is called the fornix. Consists of three layers: Outer fibrous CT adventitia; middle muscularis of smooth muscle and inner mucosa with transverse rugae. Lined with stratified squamous epithelium Vaginal orifice opens to the exterior and in virginal women is covered by an incomplete diaphragm called the Hymen Sagittal view of female reproductive tract External genitalia or Vulva = Pudendum mons pubis – fatty area anterior to the pubic symphysis; covered with pubic hair. labia majora – large fatty skin fold running posteriorly to the mons; the female homologue of the male scrotum. labia minora – smaller fatty skin fold; medial to the labia majora. vestibule – area surrounded by the labia minora; contains the vaginal and urethral openings; also contains the vestibular glands which are responsible for secreting mucous External genitalia or Vulva = Pudendum clitoris – small protruding structure of erectile tissue (corpus cavernosa) located anterior to the vestibule and within the prepuce (hood). – Consists of the glans and crus (similar to penis) – is the female homologue of the male penis and is highly sensitive to touch. – Hooded by a fold of skin called the prepuce of the clitoris. External genitalia External genitalia Clitoris Glans Crus Greater vestibular gland Urethral orifice Vestibular bulb Vestibule Mammary Glands Present in both sexes, and become functional in females after giving birth. They function only during lactation in response to hormonal stimulation to nourish the infant. Contain a large lymphatic vascular network. Two principal regions: Body and axillary tail. – Body is the pendulous portion and extends to the nipple. The nipple is in the center of a circular colored zone = areola. – Axillary tail is at base and extends toward the armpit region. – Lymphatics in axillary region drain from the mammary glands and are important route for metastatic breast cancer. Mammary glands anatomical structure Mammary Glands Structure – modified sweat glands; at puberty the female duct system partially develops, but the increase in breast size is largely due to fat deposition. It does not become fully secretory until pregnancy occurs. In non-pregnant females breast size is determined by presence of fatty tissue within the breast. Structure – modified sweat glands; at puberty the female duct system partially develops, but the increase in breast size is largely due to fat deposition. It does not become fully secretory until pregnancy occurs. In non-prenanat females breast size is determined by presence of fatty tissue within the breast. Vascular supply is from lateral and internal thoracic artery as well as the posterior intercostal artery. Mammary glands anatomical structure Consist of: lobes/interlobar connective tissue – 15 to 25 lobes formed by strips of the suspensory (Cooper) ligament and radiate around and open at the nipple. lobules with alveoli – smaller units that contain alveoli that produce milk when the female is lactating. lactiferous duct – tubes that receive milk from alveolar glands and empty into lactiferous sinus. lactiferous sinus – dilated region at end of lactiferous ducts and stores milk prior to release during suckling by infant. Mammary glands anatomical structure