Effects of orthotic heel wedges on lower limb biomechanics

1 16th June 2015
2
3
4 Orthotic Heel Wedges do not alter Hindfoot Kinematics and Achilles Tendon Force during Level and Inclined Walking in Healthy Individuals 5
6
7 Robert A Weinert-Aplin, 1,2 Anthony M J Bull, 2 Alison H McGregor 1
8
9
10
11
1
Department of Surgery and Cancer, Imperial College London, London, U.K.;
2
Department of Bioengineering, Imperial College London, London, U.K.
12
13 Funding: This study was funded by an EPSRC Case award, with financial contributions from
14 Vicon Motion Systems for the running costs of the project.
15
16 Conflicts of interest statement: None
17
18 Correspondence Address :
19
20
21
22
23
24
25
26
Robert Weinert-Aplin,
Department of Bioengineering,
Royal School of Mines,
South Kensington Campus,
Imperial College London,
London, SW7 2AZ,
United Kingdom
27
1
28 Abstract
29 Conservative treatments such as in-shoe orthotic heel wedges to treat musculoskeletal
30 pathologies are not new. However, the mechanical basis by which such orthoses act have not
31 been elucidated. Quantifying the mechanical changes that occur when wearing heel wedges
32 may help to explain the mixed evidence supporting their use in management of Achilles
33 tendonitis.
34 A musculoskeletal modelling approach was used to quantify changes in lower limb
35 mechanics when walking due to the introduction of 12mm orthotic heel wedges. A control
36 group of 19 healthy volunteers walked on a level and inclined walkway while optical motion,
37 forceplate and plantar pressure data were recorded as model inputs.
38 Heel wedges induced a posterior shift of centre of pressure that resulted in increased ankle
39 dorsi-flexion moments and reduced plantar-flexion moments. Consequently, this resulted in
40 increased peak ankle dorsi-flexor muscle forces during early stance and reduced Tibialis
41 Posterior and toe flexor muscles forces during late stance. Heel wedges did not reduce triceps
42 surae muscle forces during any walking condition.
43 These results add to the body of clinical evidence against the use of heel wedges
44 hypothesised to reduce Achilles tendon loading, as a means to treat Achilles tendonitis . our
45 findings provide an explanation as to why this theory is not appropriate.
46
47 Keywords: tendonitis, tendinitis, musculoskeletal, modelling, conservative treatment
48 Word Count: 3427
49
50
2
51
52
Introduction
The Achilles tendon is functionally important as it is the main driver of locomotion.
53
54
Consequently it is a highly loaded tendon, with reported loads of up to 5 times body weight
(BW) during level walking
1
and 8.2BW- 12.5BW during running.
55
56 loads being experienced by the Achilles, it is unsurprising that the Achilles is a common site of overuse injury,
4
with 5-18% of all lower extremity injuries involving the Achilles tendon.
5
57 As a result of this high injury prevalence, there have been a number of reviews into Achilles
58 injuries.
6-11
59 Risk factors for Achilles injuries include: magnitude of Achilles tendon load,
60 inappropriate equipment such as inappropriate footwear
12
, training errors
7
and abnormal kinematics.
6
Abnormal kinematics are generally considered to be related to over-pronation of 61
62 the hindfoot causing asymmetric loading across the Achilles tendon.
7 While there is some
63
64 evidence to show differences in strain across the tendon cross-section
13
and along the length,
14
over-pronation alone has not been linked to injury risk in running.
65
66 been shown that differences exist between Medial Gastrocnemius and Soleus contractile
20
and cycling,
21
suggesting that differential strains
67 across the tendon may exist naturally during these activities.
68 Treatments for tendinopathies have varied substantially over the years, but have
69 always been aimed at reducing or eliminating pain in the tendon. Conservative treatments
70 which directly address the Achilles tendon include: : Rest Ice Compression Elevation, eccentric strengthening exercises,
22-25
and ultrasound.
27
Of the treatments that influence 71
72
mechanical alignment of the hindfoot, insoles and splints are the only option 24,26 , but have
73 been shown to reduce pain and aid in return to sport following Achilles tendinopathy.
17
74 However, the direct link between correcting hindfoot motion and tendon healing has not been
75 established, but this treatment is still recommended.
9
3
76
77
Currently it is believed that incorporating heel wedges aids in reducing tendon strain
during activities to avoid excess tendon loading and reduce pain during running.
78 Investigations regarding heel wedges which plantarflex the ankle by raising the heel equally
79 on the medial and lateral sides, insoles and other orthotics have had variable success
80
regarding reduction of pain and ability to return to sport.
81 require no invasive procedures and injury management can be at home and on-going, they are
82 particularly appealing.A similar approach has been used in osteoarthritis, where knee
83 adduction moment has been the target of a variety of orthotics that aimed to alter the
84 mechanical loading of the knee by altering the frontal plane alignment of the hindfoot, with
85
86 several studies showing positive effects of using foot orthotics on knee adduction moment
34 and tibio-femoral load.
35
However, while studies investigating such orthotics have been
87 focussed on influencing out of plane moments at the knee, investigations of orthotics
88 focussed on relieving Achilles tendon strain through plantarflexion of the ankle are less
89 common. With wedges being able to alter loading at the knee, it is not unreasonable to
90 hypothesise that a similar approach could alter the loading at the ankle, and indeed, this is the
91 basis by which heel wedges are thought to operate during walking when managing Achilles
92 tendon pain in Achilles Tendonitis patients.
36 Therefore, the hypothesis of this study was that
93 heel wedges which raise the heel are able to reduce Achilles tendon force during level and
94 inclined walking.
95 The aim of this study was to quantify the effect of heel wedges on lower limb
96 mechanics, specifically ankle joint angles, moments and muscle forces; and relate these to
97 common injuries such as Achilles tendonitis. This is conducted during level and inclined
98 walking in order to understand their effect beyond the constrained context of level walking.
99 Methods
4
100 The participant group consisted of nineteen healthy individuals, with no history of
101 ankle injuries and no lower limb injury in the last 12 months and no clinical symptoms of
102 Achilles Tendinopathies (8 male [mean (SD); age: 28 (3); height: 1.76 m (0.10); mass: 73.4
103 kg (12.0)] and 11 females [age: 29 (6); height: 1.63 m (0.05); mass: 58.7 kg (10.2)].
104 Individuals were excluded if they had ever been diagnosed with Achilles Tendinopathy or
105 had any previous musculoskeletal or neuromuscular condition of the lower limb.
Ethical
106 approval was obtained by a university institutional review board in accordance with the
107 Declaration of Helsinki and all participants were given an information sheet and provided a
108 signed consent form upon arrival.
109 A pair of commercially available orthotic heel wedges were used by all participants
110 (Elevator Proheel™, Talar Made Orthotics Ltd, Springwood House, Foxwood Way,
111 Chesterfield, Derbyshire, England) (Figure 1). The wedges are made from medium density
112 ethylene vinyl acetate (EVA) foam and are designed to mould to the rearfoot and elevate the
113 heel, with the aim of being used as a tendonitis treatment. Wedges were available for UK
114 shoe sizes 2-5; 6-9 and 9.5-12.5 and all wedges had a 12mm rise from the front edge of the
115 wedge to approximately where the centre of the heel would be. Participants were fitted with
116 wedges corresponding to their running shoe size. All participants wore standard running
117 shoes that they felt comfortable in. Shoes were checked visually for excessive wear under the
118 sole and participants confirmed that they had used their running shoes previously before
119
120 participating in the study. A wedge height of 12mm was chosen as it represents a height that is recommended for Achilles tendonitis patients.
36
121 The mechanical effect of heel wedges on a variety of walking conditions necessitated
122 the need for an inclined walkway which could securely accommodate a forceplate either on a
123 level or inclined surface (Figure 2). The setup allowed the participants to approach the 10°
124 incline on a level surface for several steps, before ascending the 2m inclined section where
5
125 foot strike was recorded followed by a few steps of level walking at the top of the incline.
126 Participants were then asked to turn around and walk down the incline to provide the data for
127 the downhill walking condition .
For both inclined and declined walking, all participants
128 required three steps to cover the 2m inclined section, with the middle step being used for
129 subsequent analysis.
Participants were given as long as they needed to familiarise themselves
130 with each condition. This was assessed by participants themselves as they walked freely
131 around the laboratory and up and down the level and inclined walkway until they felt
132 comfortable. The amount of time taken by each individual was not measured, but was on the
133 order of a few minutes.
134 Participants were given time to familiarise themselves with the equipment and testing
135 protocol before data collection began. 3D optical motion (Vicon Motion Systems, Oxford,
136 UK), plantar pressure (Novel GmbH, Munich, Germany) and forceplate (Kistler, Winterthur,
137 Switzerland) data were collected for all conditions and used as inputs to the musculoskeletal
138 model (described below). Optical motion and plantar pressure data were recorded at 100Hz
139 and forceplate data were recorded at 1000Hz. Data were recorded continuously while the
140
141
142 participants walked over the level or inclined walkway with a minimum of 5 clean strikes of the forceplate when walking in running shoes (“shod walking”) or in running shoes with the orthotic heel wedges (“wedged walking”). Both the walking condition order (shod or wedged
143 walking) and walking incline (level, uphill or downhill) were randomised. Participants were
144 given time to become used to the heel wedges when going between shod and wedged walking
145 conditions on each incline and were able to walk freely along the level or inclined walkway
146 without targeting the forceplate.
147 The musculoskeletal model used here has been described elsewhere previously; 37 in
148 summary, it is a unilateral model of the lower limb, scaled to participant height and weight by
149
optical markers placed on the pelvis and lower limb (Figure 3), with the Achilles insertion,
6
150 the first metatarsal head and base, the fifth metatarsal head and base and the tip of the second
151
152 phalanx digitised as virtual landmarks relative to the marker clusters on the foot and hallux.
Ошибка! Источник ссылки не найден.
The measured optical motion data were used to
153 calculate joint angles and inter-segmental moments using Euler angle decompositions and
154 Newton-Euler equations at the metatarsophalangeal (MTP), ankle, knee and hip joints
155 respectively and a static optimisation routine used to estimate muscle forces for the 13
156 muscles crossing the ankle joint and Achilles tendon force is taken as the sum of the triceps
157 surae muscle forces. The knee and hip were modelled with 3 rotational degrees of freedom
158 and the ankle modelled as a saddle with 2 degrees of freedom and the MTP as a hinge with 1
159 rotational degree of freedom. Inter-segmental moment data are presented in the local segment
160 coordinate frame in which they were calculated. Centre of pressure (CoP) data are presented
161 as dimensionless values normalised to foot length, defined as the RMS distance from the
162 calcaneus to the second metatarsal head.
163 Statistical analyses were performed in Matlab using the Statistical Analysis Toolbox
164 (Version 2010b, The Mathworks Inc.). All data was checked for normality using a
165 Kolmogorov-Smirnov test. As the effect of orthotic heel wedges on lower limb mechanics
166 was the parameter of interest, statistical comparisons between shod and wedged walking for
167 each incline individually was performed using paired t-tests, with the level of significance set
168 at 0.05. P-values under 0.1 are presented as trend changes and values above 0.1 are not
169 presented. Statistical comparisons for all hip, knee, ankle and MTP kinematics and inter-
170 segmental moments were performed at heel-strike (HS), defined by a forceplate force
171 exceeding 40N, weight-acceptance (WA), push-off (PO) and toe-off (TO), with the latter
172
173 three time-points defined according to changes in knee flexion angle.
38
Inter-segmental moments were normalised to body weight (BW) and height (ht).
39
Peak muscle forces were
7
174 compared across all of stance phase, and in the case of the inv/evertor muscles, peak forces
175 were compared during early (<50 %) and late (≥ 50 %) stance.
176
177
Results
For the full gait analysis results, the reader is directed to the supplementary material.
178 The results presented here are those directly related to the calculation of the ankle muscle
179 forces. Changes in overall gait dynamics due to heel wedges were only observed during
180 inclined walking as an increase in stance time (Table 1). Compared to shod walking, the most
181 anterior centre of pressure (CoP) position was found to be less anterior during uphill and
182 downhill wedged walking by 3% (P = .002) and 4% (P = .014) foot length respectively.
183 At all time points considered no changes in peak frontal plane kinematics were
184 observed during level or inclined wedged walking, but changes in sagittal plane ankle
185 kinematics were observed during inclined walking (Figure 4).. Changes in ankle angle were
186 confined to early stance, with a more plantar-flexed ankle at HS (-1.4±5.5° vs. -4.5±7.2°, P =
187 .024 and -9.0±4.3° vs. -10.9±5.3°, P = .015 uphill and downhill respectively) and WA (-
188 1.0±5.5° vs. -5.2±9.4°, P = .034, -18.6±4.8° vs. -21.4±5.3°, P = .003 uphill and downhill
189 respectively) during wedged walking. Sagittal plane ankle angles were unaffected by heel
190 wedges during level walking. Compared to the shod condition, ankle ROM was observed to
191 decrease during uphill wedged walking (35.1±5.7° vs. 32.1±4.6°, P = .035), but increase
192 during downhill wedged walking (21.9±5.4° vs. 25.9±6.3°, P < .001).
193 Ankle joint moments were significantly affected by the presence of heel wedges at
194 each incline (Figure 5). Changes at the ankle during level walking were less apparent
195 compared to uphill or downhill walking, with delays to peak ankle dorsi-flexion and plantar-
196 flexion moments by 2% stance and 1% stance respectively only.
8
197
198
199
During uphill walking, peak ankle dorsiflexion moment increased (0.01 vs. 0.06 N m∙BW -1 ∙ht -1 , P = .005)
, peak plantar flexion moment decreased (-0.85 vs. -0.79 N m∙BW -1 ∙ht -
1
, P = .002) and peak inversion moment decreased (0.09 vs. 0.06 N m∙BW
-1 ∙ht -1
, P < .001).
200
201
202
203
Similar changes in ankle moments were observed during downhill walking, with an increase in dorsiflexion moment (0.09 vs 0.14 N m∙BW
-1 ∙ht -1
, P < .001), a decrease in plantar flexion moment (-0.62 vs. -0.57 N m∙BW
-1 ∙ht -1
, P = .002) and a decrease in inversion moment
(0.09 vs. 0.07 N m∙BW -1 ∙ht -1 , P = .030).
204 The most consistent change in muscle force estimates due to heel wedges were in the
205 ankle dorsi-flexors (12–26 % BW increases in peak Tibialis Anterior force) and toe extensors
206 (range of 4–6 % BW increase for Extensor Digitorum/Hallucis Longus forces) muscle forces
207 during the first half of stance across all walking conditions (Figure 6 and Table 2). A second
208 consistent observation was the decrease in peak Tibialis Posterior and toe flexor forces during
209 level and inclined wedged walking, although this was only statistically significant during
210 inclined walking (mean decreases of 12-14 % BW for Tibialis Posterior and 9–11 % BW the
211 toe flexor muscles respectively). Critically, there was no statistically significant reduction in
212 peak Achilles force for any walking incline due to heel wedges (range of 5–14 % BW
213 decrease). The only significant changes in triceps surae loading during uphill walking were
214 decreases in the medial parts of the triceps surae (12 % BW and 6 % BW for medial Soleus
215 and medial Gastrocnemius respectively). During downhill walking, only the medial portion
216 of Soleus showed a significant decrease in peak force (9 % BW). Overall ankle joint reaction
217 force was reduced by 29 % BW during downhill wedged walking.
218
219
Discussion
The aim of this study was to quantify the effect of heel wedges on lower limb
220 mechanics, specifically ankle joint angles, moments and muscle forces; and relate these to
221 common injuries such as Achilles tendonitis. The main clinical driver behind assessing the
9
222 effect of orthotics on ankle loading during inclined walking was to determine how effective
223 heel wedges are at reducing tendon load not only on during level walking, but also on
224 inclined surfaces, where Achilles tendon loads are known to be increased. Given the mixed
225 evidence surrounding the use of heel wedges to manage Achilles tendonitis, a broader
226 characterisation of lower limb mechanics due to orthotic heel wedges would provide some
227 insight into how the body may adapt to walking with such an intervention, allowing for
228 improvements regarding injury management.
229 A number of kinematic and kinetic changes were consistently observed across
230 walking conditions and these will be discussed further. However, the key finding of the study
231 was that 12mm orthotic heel wedges did not result in a reduction in peak triceps surae or
232 overall Achilles tendon forces, as was expected from current theories on the mechanism of
233 treating Achilles tendonitis with heel wedges.
234 No changes in ground reaction forces or ankle inversion kinematics were observed for
235 any wedged walking condition. While inferring subtalar kinematics through angles derived
236 from markers on the shoe has its limitations, information regarding out of plane changes in
237 kinematics can still be gained. However, as the cohort tested here consisted of healthy
238 individuals, hindfoot motion may not have required any correction, and as such the lack of
239 difference in hindfoot kinematics here should not automatically be extrapolated to a patient
240 population. This has similar implications for the kinetics, as kinetic changes are in response
241 to the kinematic and CoP changes that occur. If patient groups reported similar CoP and
242 kinematics changes, then it is likely that the kinetic results obtained here will have direct
243 relevance to the mechanical response of the lower limb to orthotic wedges in a patient
244 population. It should be noted that the observations here are valid only for this type of heel
245 wedge and wedges aiming to shift CoP in the frontal plane may act differently.
10
246 Changes in CoP were consistently shifted posteriorly across walking conditions. This
247 had two distinct effects on lower limb loading. During early stance, a posterior shift in CoP
248 would place the GRF more posterior to the ankle joint centre, resulting in a greater
249 dorsiflexion moment and dorsiflexor muscle forces. During late stance at push-off, a
250 posteriorly shift in CoP places the GRF closer to the ankle joint centre, resulting in smaller
251 plantar flexion moments. However, as was previously mentioned, this did not result in a
252 reduction in peak triceps surae or overall Achilles tendon forces. Instead, a redistribution of
253 the triceps surae loads was observed (Figure 6), where the medial triceps surae muscle loads
254 reduced and lateral triceps surae loading increased, while the peak forces of the less efficient,
255 secondary ankle plantar flexor muscles of Tibialis Posterior and the toe flexor muscles were
256 consistently reduced during wedged walking. The redistribution of triceps surae loading from
257 the medial to lateral side has relevance in the rehabilitation of calf strains and tears, where
258
259 strains and tears are more common in the medial head of Gastrocnemius and where heel wedges are also a prescribed treatment.
40
260 The sensitivity of these secondary ankle plantar flexor muscles to changes in inter-
261 segmental moments is of particular interest, both clinically and computationally. From a
262 computational perspective, the use of a static optimisation approach to derive muscle forces
263 inherently makes less efficient muscles more sensitive to changes in inter-segmental
264 moments compared to more efficient muscles. Tibialis Posterior and the toe flexors are
265 significantly less powerful and efficient ankle plantar flexors compared to the triceps surae
266 muscles, and as such these are the muscles that one would expect to respond to changes in
267 ankle moment. However, from a clinical perspective, it is not known if the body responds in
268 such a way to changes in demand at individual joints, possibly due to practical constraints of
269 determining deep muscle electromyography (EMG) data. If this observation is indeed found
270 to be true, it may provide some explanation as to why Achilles tendonitis patients respond so
11
271 variably to orthotics. Therefore, it is recommended that future research into the use of
272 orthotics to treat Achilles tendonitis focuses on the mechanical response specific orthotics
273 induce in the body at both individual muscle and whole joint levels with a view to proposing
274 methods to improve the conservative management of Achilles tendonitis.
275 A practical limitation of the study is that due to the inclined section being fixed to 2m,
276 it should be noted that some participants may not have reached a steady-state of inclined
277 walking, despite using the middle of the three steps on the inclined surface. However, the
278 current setup does represent a change in walking incline which would be commonly
279 experienced in daily life. A second limitation of this study relates to the absence of direct
280 measures or estimates of tendon strain, which would have complimented the changes in
281 muscle and tendon force observed. While estimating tendon strain here would require
282 combining a finite element tendon model with the musculoskeletal model implemented here,
283 which is beyond the scope of this study, such an approach may have provided a greater depth
284 of understanding into the mechanical changes that are induced by orthotic heel wedges. A
285 final limitation of the study is related to the sensitivity of musculoskeletal models to muscle
286 morphology and geometry inputs. While a limitation of any model that does not have MRI
287 datasets of their participant cohort, the use of scaled cadaveric muscle data in estimating
288 muscle loads during various activities is a common approach,
41-44
particularly when
289 comparing intra-subject gait patterns such as in this study.
290 This study characterised the effect of orthotic heel wedges on lower limb
291 biomechanics in the context of level, uphill and downhill walking, with the intention of trying
292 to quantify any mechanical differences that may arise due to heel wedges and help explain
293 the current mixed evidence surrounding heel wedges as a treatment for Achilles tendonitis.
294 Heel wedges were unable to significantly alter hindfoot kinematics, but did result in changes
295 in inter-segmental moments at all joints of the lower limb. However, heel wedges were
12
296 unable to reduce Achilles tendon loading across level, uphill and downhill walking conditions
297 in healthy individuals. Instead, secondary ankle plantarflexor muscles consistently showed
298 substantial reductions in loading. These results add to the body of largely clinical evidence
299 (pain, functional improvement etc.) that indicates that heel wedges are not an appropriate
300 treatment for Achilles tendonitis and has provided evidence as to why this is the case.
13
301
302 1.
303
304 2.
305
306 3.
307
308 4.
309
310 5.
311
312 6.
References
Stauffer RN, Chao EY, Brewster RC. Force and motion analysis of the normal, diseased, and prosthetic ankle joint. Clin Orthop Relat R. 1977(127):189-196.
Komi PV. Relevance of in vivo force measurements to human biomechanics. Journal of
Biomechanics. 1990;23 Suppl 1:23-34.
Scott SH, Winter DA. Internal forces of chronic running injury sites. Medicine & Science in
Sports & Exercise. Jun 1990;22(3):357-369.
Maffulli N, Wong J, Almekinders LC. Types and epidemiology of tendinopathy. Clinical
Journal of Sport Medicine. Oct 2003;22(4):675-692.
Donoghue OA, Harrison AJ, Laxton P, et al. Lower limb kinematics of subjects with chronic achilles tendon injury during running. Research in Sports Medicine. 2008;16(1):23-38.
Reinking M. Tendinopathy in athletes. Phys Ther Sport. Feb 2012;13(1):3-10.
313 7.
314
315 8.
Kader D, Saxena A, Movin T, et al. Achilles tendinopathy: some aspects of basic science and clinical management. Brit J Sport Med. Aug 2002;36(4):239-249.
Paavola M, Kannus P, Jarvinen TA, et al. Achilles tendinopathy. J Bone Joint Surg Am. Nov
316
317 9.
318
319
2002;84-A(11):2062-2076.
Cook JL, Khan KM, Purdam C. Achilles tendinopathy. Manual Therapy. Aug 2002;7(3):121-
130.
10. Schepsis AA, Jones H, Haas AL. Achilles tendon disorders in athletes. The American Journal of
320
321
322
Sports Medicine. Mar-Apr 2002;30(2):287-305.
11. McCrory JL, Martin DF, Lowery RB, et al. Etiologic factors associated with Achilles tendinitis in runners. Med Sci Sport Exer. Oct 1999;31(10):1374-1381.
323 12. McCrory JL, Martin DF, Lowery RB, et al. Etiologic factors associated with Achilles tendinitis
324 in runners. Med Sci Sports Exerc. Oct 1999;31(10):1374-1381.
14
325 13. Lersch C, Grotsch A, Segesser B, et al. Influence of calcaneus angle and muscle forces on
326 strain distribution in the human Achilles tendon. Clin Biomech (Bristol, Avon). Nov
327
328
329
2012;27(9):955-961.
14. Farris DJ, Trewartha G, McGuigan MP, et al. Differential strain patterns of the human Achilles tendon determined in vivo with freehand three-dimensional ultrasound imaging. Journal of
330
331
Experimental Biology. Feb 15 2013;216:594-600.
15. Chuter VH, Janse de Jonge XAK. Proximal and distal contributions to lower extremity injury:
332
333
A review of the literature. Gait & Posture. 2012;36(1).
16. Kaufman KR, Brodine SK, Shaffer RA, et al. The effect of foot structure and range of motion
334
335
336 on musculoskeletal overuse injuries. Am J Sport Med. Sep-Oct 1999;27(5):585-593.
17. Van Ginckel A, Thijs Y, Hesar NG, et al. Intrinsic gait-related risk factors for Achilles tendinopathy in novice runners: a prospective study. Gait & Posture. Apr 2009;29(3):387-
337
338
391.
18. Cronin NJ, Avela J, Finni T, et al. Differences in contractile behaviour between the soleus and
339
340 medial gastrocnemius muscles during human walking. Journal of Experimental Biology. Mar
1 2013;216:909-914.
341 19. Farris DJ, Sawicki GS. Human medial gastrocnemius force-velocity behavior shifts with
342
343 locomotion speed and gait. Proceedings of the National Academy of Sciences U S A. Jan 17
2012;109(3):977-982.
344 20. Wyndow N, Cowan SM, Wrigley TV, et al. Triceps surae activation is altered in male runners
345
346 with Achilles tendinopathy. Journal of Electromyography and Kinesiology. Feb
2013;23(1):166-172.
347 21. Sanderson DJ, Martin PE, Honeyman G, et al. Gastrocnemius and soleus muscle length,
348
349 velocity, and EMG responses to changes in pedalling cadence. Journal of Electromyography
and Kinesiology. Dec 2006;16(6):642-649.
15
350 22. Sayana MK, Maffulli N. Eccentric calf muscle training in non-athletic patients with Achilles
351 tendinopathy. Journal of Science and Medicine in Sport. Feb 2007;10(1):52-58.
352 23. Maffulli N, Walley G, Sayana MK, et al. Eccentric calf muscle training in athletic patients with
353
354
Achilles tendinopathy. Disability and Rehabilitation. 2008;30(20-22):1677-1684.
24. Roos EM, Engstrom M, Lagerquist A, et al. Clinical improvement after 6 weeks of eccentric
355
356 exercise in patients with mid-portion Achilles tendinopathy - a randomized trial with 1-year follow-up. Scandinavian Journal of Medicine & Science in Sports. Oct 2004;14(5):286-295.
357 25. Rees JD, Lichtwark GA, Wolman RL, et al. The mechanism for efficacy of eccentric loading in
358 Achilles tendon injury; an in vivo study in humans. Rheumatology (Oxford). Oct
359
360
361
2008;47(10):1493-1497.
26. Mayer F, Hirschmuller A, Muller S, et al. Effects of short-term treatment strategies over 4 weeks in Achilles tendinopathy. Brit J Sport Med. Jul 2007;41(7).
362 27. Enwemeka CS. The effects of therapeutic ultrasound on tendon healing. A biomechanical
363
364
365 study. Am J Phys Med Rehab. Dec 1989;68(6):283-287.
28. Clement DB, Taunton JE, Smart GW. Achilles tendinitis and peritendinitis: etiology and treatment. Am J Sport Med. May-Jun 1984;12(3):179-184.
366 29. Farris DJ, Buckeridge E, Trewartha G, et al. The effects of orthotic heel lifts on achilles
367
368 tendon force and strain during running. J Appl Biomech. Nov 2012;28(5):511-519.
30. Magnussen RA, Dunn WR, Thomson AB. Nonoperative treatment of midportion Achilles
369
370
371 tendinopathy: a systematic review. Clinical Journal of Sport Medicine. Jan 2009;19(1):54-64.
31. Gross ML, Davlin LB, Evanski PM. Effectiveness of orthotic shoe inserts in the long-distance runner. Am J Sport Med. Jul-Aug 1991;19(4):409-412.
372 32. Stackhouse CL, Davis IM, Hamill J. Orthotic intervention in forefoot and rearfoot strike
373
374
375 running patterns. Clin Biomech. Jan 2004;19(1):64-70.
33. Ferber R, Benson B. Changes in multi-segment foot biomechanics with a heat-mouldable semi-custom foot orthotic device. Journal of Foot & Ankle Research. 2011;4(1):18.
16
376 34. Erhart JC, Mundermann A, Elspas B, et al. Changes in knee adduction moment, pain, and
377 functionality with a variable-stiffness walking shoe after 6 months. J Orthopaed Res. Jul
378
379
380
2010;28(7):873-879.
35. Kutzner I, Damm P, Heinlein B, et al. The effect of laterally wedged shoes on the loading of the medial knee compartment-in vivo measurements with instrumented knee implants. J
381
382
Orthopaed Res. 2011;29(12):1910-1915.
36. Carcia CR, Martin RL, Houck J, et al. Achilles pain, stiffness, and muscle power deficits:
383
384 achilles tendinitis. J Orthop Sports Phys Ther. Sep 2010;40(9):A1-26.
37. Weinert-Aplin RA, Bull AMJ, McGregor AH. Investigating The Effects of Knee Flexion During
385
386
The Eccentric Heel-drop Exercise. Journal of Sports Science and Medicine. 2015;14(2):459-
465.
387 38. Shamaei K, Sawicki GS, Dollar AM. Estimation of quasi-stiffness of the human knee in the
388
389 stance phase of walking. PLoS One. 2013;8(3).
39. Moisio KC, Sumner DR, Shott S, et al. Normalization of joint moments during gait: a
390
391 comparison of two techniques. Journal of Biomechanics. 4// 2003;36(4):599-603.
40. Bryan Dixon J. Gastrocnemius vs. soleus strain: how to differentiate and deal with calf
392
393
394 muscle injuries. Curr Rev Musculoskelet Med. Jun 2009;2(2):74-77.
41. Erdemir A, McLean S, Herzog W, et al. Model-based estimation of muscle forces exerted during movements. Clin Biomech. Feb 2007;22(2):131-154.
395 42. Modenese L, Phillips AT, Bull AM. An open source lower limb model: Hip joint validation.
396
397
Journal of Biomechanics. Aug 11 2011;44(12):2185-2193.
43. Lundberg HJ, Foucher KC, Andriacchi TP, et al. Direct comparison of measured and calculated
398
399 total knee replacement force envelopes during walking in the presence of normal and abnormal gait patterns. Journal of Biomechanics. 2012;45(6):990-996.
17
400 44. Delp SL, Anderson FC, Arnold AS, et al. OpenSim: open-source software to create and
401 analyze dynamic simulations of movement. IEEE Trans Biomed Eng. Nov 2007;54(11):1940-
402 1950.
403
404
18
405
406
407
Figure 1 : Image of the 12mm orthotic heel wedge used by all participants
19
408
409
410
411
Figure 2 : Sketch of the inclined walkway setup
20
412
413
414
415
416
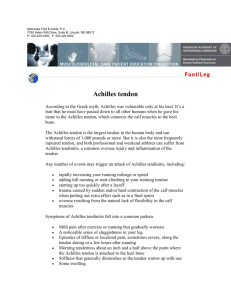
Figure 3: Posterior (left) and lateral (right) views of the optical marker setup. Note: Grey circles indicate reflective marker positions
21
417
418
419
420
421
422
423
424
425
426
Figure 4 : Mean shod (black lines) and wedged (grey lines) ankle joint angles (A-C) and moments (D-F)when walking uphill (left column), on level ground (middle column) and downhill (right column) . Note: Solid lines represent flexion/extension angles and dashed lines represent inv/eversion angles and moments. * denotes a statistically significant difference
22
A B C
D
G
*
E
*
H
F
I
*
J
K L
427
428
429
430
431
432
433
434
435
436
437
Figure 5 : Mean shod (solid lines) and wedged (dashed lines) muscle forces when walking uphill (left column), on level ground (middle column) and downhill (right column) for the
Achilles (A-C), triceps surae (D-F), inv/evertor (G-I) and toe (J-L) muscles. Note:
Abbreviations are: GastMed/GastLat – Medial/Lateral heads of the Gastrocnemius,
SolMed/SolLat – Medial and lateral portions of Soleus, PeroB/L and PeroT – Peroneus
Brevis/Longus and Tertius, TibAnt/TibPost, Tibialis Anterior and Tibialis Posterior,
EDL/EHL – Extensor Digitorum/Hallucis Longus, FDL/FHL – Flexor Digitorum/Hallucis
Longus. * denotes statistically significant change in peak force (only shown for the triceps surae muscles for clarity).
23
438
439
440
441
442
Table 1: Comparison of forceplate and spatio-temporal gait characteristics across all inclines, mean (SD).
Stance time [s]
Velocity [m/s]
Most Posterior
CoP
[normalised]
Most Anterior
CoP
[normalised]
CoP travel per step
[normalised]
Uphill Level Downhill
Shod Wedged Shod Wedged Shod Wedged
0.72
(0.08)
1.20
(0.24)
0.03
(0.07)
0.73
(0.10)
1.18
(0.24)
0.01
(0.09)
0.69
(0.08)
1.24
(0.20)
0.01
(0.07)
0.70
(0.07)
1.21
(0.20)
-0.01
(0.08)
0.63
(0.09)
1.20
(0.24)
0.03
(0.09)
0.65*
(0.08)
1.17
(0.24)
0.01
(0.08)
0.68
(0.08)
0.64
(0.10)
0.65*
(0.08)
0.63
(0.10)
0.66
(0.07)
0.65
(0.09)
0.63
(0.07)
0.64
(0.10)
0.66
(0.07)
0.63
(0.11)
0.62*
(0.07)
0.61
(0.10)
* denotes P < .05 between shod and wedged conditions
24
443
444
445
446
Table 2 : Comparison of peak muscle and ankle joint reaction forces during shod and wedged walking across all inclines . Note: For full muscle names, see Figure 6 notes; Data presented as mean (SD).
Peak Force
[BW]
Muscle Shod
Uphill
Wedged p-value Shod
Level
Wedged p-value Shod
Downhill
Wedged p-value
SolMed 1.30
( 0.26) 1.18
( 0.34) 0.047 1.16 (0.27) 1.03 (0.29) - 0.96
( 0.23) 0.87
( 0.23) 0.040
Triceps
Surae
SolLat 0.77 (0.35) 0.88 (0.41)
GastMed 0.72
( 0.15) 0.67
( 0.18)
GastLat 0.24 (0.08) 0.25 (0.08)
-
0.040
-
0.55 (0.33) 0.59 (0.34)
0.66 (0.16) 0.59 (0.16)
0.20 (0.07) 0.20 (0.06)
-
-
-
0.53 (0.23) 0.60 (0.26)
0.53 (0.12) 0.49 (0.12)
0.17 (0.04) 0.18 (0.05)
-
-
-
Achilles - 2.47 (0.61) 2.33 (0.59) - 2.15 (0.48) 2.10 (0.54) -
Invertor/
Evertors
(1 st half of stance)
Invertor/
Evertors
(2 nd half of stance
Toes
Ankle JRF
PeroB/L
PeroT
TibAnt
TibPost
PeroB/L
PeroT
TibAnt
TibPost
EDL
EHL
FDL
FHL
2.98 (0.69) 2.92 (0.81)
0.10
( 0.11) 0.30
( 0.30)
0.02
( 0.03) 0.07
( 0.06)
0.26 (0.11) 0.38 (0.24)
0.33
( 0.15) 0.20
( 0.14)
0.09 (0.10) 0.17 (0.19)
0.01 (0.00) 0.01 (0.01)
0.31
( 0.14) 0.21
( 0.16)
0.50
( 0.21) 0.36
( 0.23)
0.02
( 0.03) 0.06
( 0.06)
0.02
( 0.02) 0.06
( 0.05)
0.04
( 0.02) 0.03
( 0.02)
0.39
( 0.17) 0.29
( 0.16)
5.17 (0.86) 4.88 (1.12)
0.002
0.002
0.058
<0.001
-
0.057
0.012
0.020
0.002
0.002
0.023
0.015
-
0.29
( 0.27) 0.61
( 0.45)
0.09
( 0.06) 0.15
( 0.09)
0.53
( 0.22) 0.79
( 0.37)
0.31
( 0.13) 0.20
( 0.16)
0.06 (0.10) 0.11 (0.13)
0.00 (0.01) 0.01 (0.01)
0.33 (0.15) 0.26 (0.16)
0.53 (0.23) 0.41 (0.26)
0.09
( 0.06) 0.15
( 0.09)
0.08
( 0.05) 0.14
( 0.08)
0.04 (0.02) 0.03 (0.02)
0.42 (0.18) 0.31 (0.18)
4.69 (0.83) 4.28 (0.85)
0.027
0.035
0.030
0.029
-
-
-
0.095
0.036
0.032
0.058
0.064
-
0.38
( 0.30) 0.67
( 0.51)
0.09
( 0.07) 0.15
( 0.10)
0.56
( 0.25) 0.75
( 0.36)
0.37
( 0.21) 0.26
( 0.22)
0.06 (0.08) 0.10 (0.10)
0.01 (0.08) 0.01 (0.01)
0.26
( 0.10) 0.18
( 0.10)
0.41
( 0.16) 0.29
( 0.17)
0.09
( 0.07) 0.15
( 0.09)
0.09
( 0.06) 0.14
( 0.08)
0.04
( 0.02) 0.03
( 0.02)
0.34
( 0.14) 0.25
( 0.15)
3.82
( 0.64) 3.53
( 0.70)
0.003
<0.001
0.002
0.003
0.083
0.076
0.006
0.005
<0.001
<0.001
0.003
0.002
0.037
25