16 Bichet Hyponatremia Nov 2012
advertisement

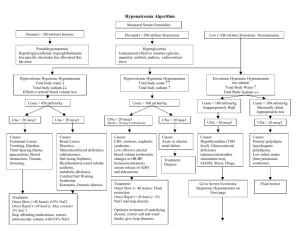
Investigation and Treatment of Hyponatremic States Daniel G. Bichet, M.D. Professeur of Medicine and Physiology, Université de Montréal Hôpital du Sacré-Cœur de Montréal Conflict Disclosures The speaker has received fees/honoraria and grants from Otsuka Pharmaceutical. An honorarium from Otsuka Pharmaceutical will also be received related to the present lecture. Some of the drugs, devices, or treatment modalities mentioned in this presentation are: Samsca (Tolvaptan) from Otsuka Pharmaceutical Speaker: D.Bichet M.D. Title Hyponatremia – date Nov 24 2012 At the end of this presentation, the attendee will able to: • Understand the role of vasopressin secretion and its non-suppression by hyponatremia in most clinically important hyponatremic states • Distinguish hypovolemic hyponatremia (easily treated with volume repletion) from euvolemic and hypervolemic hyponatremic states • Recognize the importance and urgency of treating symptomatic hyponatremia where severe neurologic manifestations are related to brain edema Objectives (2) • Understand the need to treat chronic hyponatremia slowly to prevent osmotic demylination syndrome • Understand the value and limitations of indirect treatments such as water restriction, urea, furosemide and sodium compared to direct inhibition of the vasopressin V2 receptor with a V2 receptor antagonist How cats lap: water uptake by Felis catus Science. 2010 Nov 26;330(6008):1231-4. Epub 2010 Nov 11. We show that the domestic cat (Felis catus) laps by a subtle mechanism based on water adhesion to the dorsal side of the tongue. Hyponatremia:PNa<136 mmol/L serum [Na+] ~ Na+E + K+E body water Two factors to evaluate: deficit in Na+/K+; excess water Normal glucose, increased in protein or lipids could decrease the volume of water where Na+ is measured: pseudo-hyponatremia. Mannitol, maltose or glycine: hyponatremia with hyper-osmolality.Urea is a permeable osmolyte and do not cause hyponatremia Prevalence of Hyponatremia at Initial Presentation to a Healthcare Provider 30 Percentage (%) 25 28.2 Acute hospital care Ambulatory hospital care Community care 21.0 20 15 10 7.2 5 2,60 0,49 0 0,17 0,03 Na <116 0,96 0,14 Na <126 Na <136 Serum [Na+] (mEq/L) Tan Tock Seng Hospital, Singapore. Data from 303,577 samples on 120,137 patients available for analysis. 7 Hawkins RC. Clin Chim Acta. 2003;337(1-2):169-172. Risk Factors for Hyponatremia Selected Conditions1 Selected Drug Classes • • • • • • • • Congestive Heart Failure Cirrhosis SIADH Very young or very old age Adrenal insufficiency Hypothyroidism Renal dysfunction Central nervous system impairment • • • • • • • • • • Surgery or injury Diuretics1,2 NSAIDs1,2 Opiate derivatives1,2 Antidepressants1,2 Antipsychotics1,2 Antiepileptic agents1,2 Anticancer agents1,2 Antihypertensive agents2 Proton-pump inhibitors2 [Na+] <135 mEq/L3 NSAIDS = Nonsteroidal Anti-inflammatory Agents, SIADH = Syndrome of Inappropriate Antidiuretic Hormone.1. Adrogué HJ. Am J Nephrol. 2005;25:240-249. 2. Liamis G, et al. Am J Kidney Dis. 2008;52:144-153. 3. Ellison DH, Berl T. N Engl J Med. 2007;356(20):2064-2072. 8 Falls Are a Common Symptom of Chronic “Asymptomatic” Hyponatremia 25 21.3 Falls (%) 20 Adjusted OR 67.4, 95% CI 7.5–607.4, P<.001 Odds Ratio: probability ratio Odds = The probability of events / the probablity of non-events 15 10 5.3 5 0 Mean Serum [Na+]: No. of Patients: Hyponatremic Patients Controls 126±5 mEq/L 139±2 mEq/L (n=122) (n=244) Patients with chronic “asymptomatic” hyponatremia were admitted for falls significantly more frequently than patients with normal [Na+] levels Data based on a case-control study in a general Belgium hospital.Renneboog B, et al. Am J 9 Med. 2006;119(1):71.e1-71.e8. Hyponatremia in Patients With Bone Fractures Resulting From Incidental Falls Patients With Hyponatremia (%) 14 13.1% 12 Adjusted OR (CI): 4.16 (2.24–7.71) P<.001 10 8 6 3.9% 4 Hyponatremia was mild and asymptomatic in all patients (mean serum [Na+] 131 mEq/L) and was found to be associated with bone fracture after incidental fall in ambulatory elderly 2 0 Patients (n=513) Control (n=513) Case control study of 513 cases of bone fracture after incidental fall in ambulatory patients ≥65 y in general university hospital. Gankam Kengne F, et al. QJM. 2008;101(7):583-588. • Rat model SIADH: hyponatremia induced x 3 months - ↓ BMD ~ 30% • NHANES III survey data: mild hyponatremia ~ Adj-OR 2.85 osteoporosis Hyponatremia Rats Non-Hyponatremic Rats Restrictive Cubic Spline Depicting the Unadjusted Relationship Between Hospital Admission Serum Sodium Concentrations and In-Hospital Mortality Predicted Probability of In-Hospital Mortality 0.20 0.15 0.10 0.05 110 115 120 125 130 135 140 145 Admission Serum [Na+] Concentration (mEq/L) Wald R, et al. Arch Intern Med. 2010;170(3):294-302. Hyponatremia and Long-term Outcomes • Prospective cohort study of 98,411 adults hospitalized between 2000 and 2003 • Assessed in-hospital, 1-year, and 5-year mortality • Hyponatremia (serum [Na+] <135 mmol/L) was observed in 14.5% of patients on initial measurement • Those with hyponatremia were older (67.0 vs 63.1 years) and had more comorbid conditions (mean Deyo-Charlson index 1.9 vs 1.4) Waikar SS, et al. Am J Med. 2009;122(9):857-865. Odds Ratio for Death in Patients With Hyponatremia According to Clinical Subtypes 1.47 Overall 1.30 Acute myocardial infarction 1.44 Congestive heart failure Odds Ratio: probability ratio Odds = The probability of events / the probablity of non-events 1.06 Sepsis 1.00 Pneumonia 1.55 Chronic kidney disease 0.91 Liver disease 1.08 Gastrointestinal bleeding 1.21 Volume depletion 2.05 Metastatic cancer 1.34 Circ system: surgical 2.26 Circ system: med 2.31 Musculoskeletal: surg 1.45 Nervous system: surg 1.38 Nervous system: med 1.07 Resp system: med -2.00 -1.50 -1.00 -0.50 0.00 0.50 1.00 1.50 2.00 2.50 3.00 3.50 4.00 4.50 Multivariable-Adjusted Odds Ratio Waikar SS, et al. Am J Med. 2009;122(9):857-865. 14 Effect of Resolution of Hyponatremia on Odds Ratio for Mortality Persistent Normonatremia (n = 42,176) Persistent Hyponatremia (n = 4524) Resolved Hyponatremia (n = 3794) In-hospital mortality 1 (ref) 2.37 1.26 1-year mortality 1 (ref) 1.55 1.19 5-year mortality 1 (ref) 1.32 1.18 Analysis in patients with at least 2 serum [Na+] determinations (categorizations based on first and final serum [Na+] values). Multivariate analysis adjusted for age, sex, Deyo-Charlson index, and individual diagnoses Waikar SS, et al. Am J Med. 2009;122(9):857-865. Two types of hyponatremia Dilutional hyponatremia Total body sodium near normal Total body water increased Hypervolemic Euvolemic (edema) Heart failure* Cirrhosis* Nephrotic syndrome (no edema) SIADH* Hypothyroidism Secondary adrenal insufficiency Depletional hyponatremia Hypovolemic Sodium lost Total body water reduced Diarrhea Pancreatitis Vomiting Diuretics Burns Renal salt wasting Trauma Primary adrenal insufficiency *Share underlying pathophysiology of AVP excess. 1. Douglas I. Cleve Clin J Med. 2006;73:S4-S12. 2. Kumar S, et al. Lancet. 1998;352:220-228. hyponatremia can be caused by dilution from retained water, or by depletion from electrolyte losses in excess of water Secretion of vasopressin, the antidiuretic hormone, osmoregulatory pathways of the hypothalamus Sagital section of the ventral brain in a mouse at the level of the third ventricle MnPO : median preoptic nucleus Wilson Y, et al.: Visualization of functionally activated circuitry in the brain. Proc Natl Acad Sci USA 99:3252-3257, 2002 Determinants of Vasopressin Secretion B 5 1000 Increase in Plasma Arginine-Vasopressin (pg/mL) Plasma Arginine-Vasopressin (pg/mL) A 4 100 3 10 2 1 Detection Limit 120 125 130 1 0 135 140 Plasma Sodium (mEq/L) 145 10 20 30 40 50 60 % Fall in Mean Arterial Blood Pressure Cationic channels inactivated by stretch, TRPVs (Transient Receptor Potential Vanilloid channels), are the osmoreceptors of the anterior hypothalamus : thirst and magnocellular neurons. Hyperosmotic stimuli depolarize these cells via the activation of nonselective cation channels (NSCCs) Hypoosmolality causes hyperpolarization by inhibiting NSCCs Osmosensation in vasopressin neurons: Prager-Khoutorsky M, Bourque CW.Trends Neurosci. 2010 Feb;33(2):76-83. Non-osmotic stimulation of vasopressin, importance of Angiotensin II •angiotensin II is inducing an osmoregulatory gain. •This helps restoration of volume and blood pressure maintenance. AVP Levels Are Elevated in Patients With Hypo-osmolality and CHF 19.2 15.0 No diuretics (n=14) 14.0 Taking diuretics (n=23) Normal Range Plasma AVP (pg/mL) 13.0 12.0 4.0 3.0 2.0 1.0 0.5 0.0 250 260 270 280 290 300 Plasma Osmolality, mOsm/kg of Water Szatalowicz VL, Bichet DG et al. N Engl J Med. 1981;305:263-266. Indirect and Direct Therapies for SIADH, Cirrhosis and CHF Therapy Target: AVP Excess Isotonic Saline Limitations Hypertonic Saline Fluid Restriction Demeclocycline Urea Vasopressin antagonists 23 Ineffective in dilutional hyponatremias Can’t be used in edema-forming disorders No controlled safety database No consensus on appropriate infusion rates Overcorrection can cause osmotic demyelination Can’t be used in edema-forming disorders No controlled safety database Slow to correct; Poorly tolerated due to thirst Ineffective with high AVP levels and urine osmolalities Not approved for hyponatremia Slow to correct Nephrotoxic (esp. cirrhosis) and disposed by kidney No USP formulation Not approved for hyponatremia Poor palatability Conivaptan in USA is IV only (due to CYP3A4 inhibition) Tolvaptan accepted by Health Canada Urine/Plasma electrolyte ratio: UNa+UK/PNa+ PK to guide water restriction U/P ratio Insensible water losses Expected net water loss Recommended water consumption ≥ 1.0 800 mL - 800 mL 0 mL .5 - 1,0 800 mL -800 to -1300 mL Up to 500 mL < 0.5 800 mL -1300 to -1800 mL Up to one liter The Urine/Plasma Electrolyte Ratio: A Predictive Guide to Water Restriction:Furst,… Neilson, Eric American Journal of the Medical Sciences. 319(4):240-244, April 2000. Molar mass of urea CO(NH2)2 = 60g/mol Molecular weight calculation ; 12.0107 + 15.9994 + (14.0067 + 1.00794x2)2 60g of urea = 1000 mmol 30g of urea = 500 mmol “Medicinal urea” 30 g × 1 month will be less than $1.00: urea 10, NaHCO3 2g Citric Acid 1.5g, sucrose 200 mg 60g of urea=1000 mmol: forcing water excretion , however, bitter taste and necessity to absorb with additional fluid Daily Intake (Solute + Water) Urinary Osmolality (mOsm/kg) Urine Volume (Liter/day) Water Balance (Liter/day) Normal 500 mmol of solute + 2 liters of water 250 2 liters 0 SIADH 500 mmol of solute + 2 liters of water 500 1 liter (500/500) +1 2. 500 mmol of solute + 500 mmol of urea + 2 liters of water 500 2 liters (1000/500) 0 Editorial,What Is the Role of Vaptans in Routine Clinical Nephrology? Daniel G. Bichet Clin J Am Soc Nephrol 7: 700–703, 2012. Vasopressin Makes the Cortical and Medullary Collecting Ducts Permeable to Water Tolvaptan Bichet DG. The posterior pituitary. In: The Pituitary, 3rd Ed. Melmed, S. (ed.), Elsevier Press, Inc., 2011, pp. 261-299. Binding Sites for Agonists and Antagonists AVP and OPC 21268 (V1a) Macion-Dazard R, et al. J Pharmacol Exp Ther. 2006. 28 SALT(Study of Ascending Levels of Tolvaptan in Hyponatremia ) Criteria and Restrictions • Persistent dilutional hyponatremia – Inclusion: serum [Na+] below normal (<135 mEq/L) – Non-reversible etiology (eg, HF, cirrhosis, SIADH) – Exclusion: serum [Na+] <120 mEq/L if neurologic impairment • Concomitant therapies – “Standard of care” medications permitted – Fluid restriction was not mandatory • Safety considerations – No confounding disease (eg, recent stroke or MI, recent surgery, uncontrolled diabetes, etc) Schrier RW, et al. N Engl J Med. 2006;355(20):2099-2112. SALT-1 and SALT-2 Study Design (cont’d) Titration up to day 4 Samsca® (tolvaptan) 15 mg QD initiated in the hospital dose if serum [Na+] <136 mEq/L and serum [Na+] increase is <5 mEq/L during prior 24 hrs 30 mg/day then 60 mg/day as needed Withheld dose, decreased next dose, or increased patient’s fluid intake to mitigate risk of overly rapid correction if serum [Na+] was • >145 mEq/L, or • by >12 mEq/L during prior 24 hours, or • by >8 mEq/L during 8 hours on the 1st day Schrier RW, et al. N Engl J Med. 2006;355(20):2099-2112. Mean Change From Baseline in Serum [Na+] by Hyponatremia Etiology Pooled Analysis of SALT-1 and SALT-2; Baseline Serum [Na+] <135 mEq/L Day 30 Day 4 10 9 * Mean Change From Baseline (mEq/L) 8 7,4 * 6,6 7 6 5 * 4,8 * 4,2 * * 3,5 4 3,5 2,4 3 1,5 2 1 Samsca® (tolvaptan) (n=213) Placebo (n=203) 0,2 0,5 1,5 0,4 0 SIADH HF Cirrhosis SIADH HF Cirrhosis *P<.0001 for Samsca® (tolvaptan) vs placebo, based on Cochran-Mantel-Haenszel (CMH) Data on file: Protocols 156-02-235 and 156-03-238; Pooled. test. Improved and Maintained Serum [Na+] (Baseline Serum [Na+] <130 mEq/L) Pooled Analysis of SALT-1 and SALT-2 Samsca® (tolvaptan) 15–60 mg (n=110) Placebo (n=105) 142 Mean Serum [Na+] (±SD, mEq/L) 140 138 136 * 134 * 132 130 * * * * * * 128 126 124 122 *P<.0001 vs placebo 120 0 Baseline 8h 2 3 Day 1 4 11 18 25 30 7-day follow-up Treatment Day *P<.0001 for all visits during tolvaptan treatment compared to placebo. SF-12 Conceptual Framework Items Summary Measures Not as careful at work? (Emotional) Accomplish less at work? (Emotional) Have lots of energy? Felt calm and peaceful? Mental Component Summary - MCS Felt downhearted and blue? Social activities (Physical/Emotional) In general, is your health …? Health limit moderate activities? Health limit climbing several flights? Accomplish less work (Physical) Limited in kind of work (Physical) Has pain interfered with work? 33 Physical Component Summary - PCS Results in SF-12 Mental (MCS) Status Demonstrate Improvements in Patients With Hyponatremia (ANCOVA, LOCF) 8 Samsca® (tolvaptan) Placebo Large ES P<.05 Change From Baseline to Day 30 7 P<.05 6 P=NS Moderate ES 5 4 3 MID 2 Small ES 1 0 SALT-1 n = 83/71 SALT-2 n = 101/103 Mental Component Summary Score ES = effect size; MID = minimally important difference. 34 Data on file: Protocols 156-02-235 and 156-03-238; Pooled. Pooled n = 184/174 Hyponatremia secondary to SIADH Severe symptoms (seizures, coma, respiratory distress) Active therapy with hypertonic saline Moderate symptoms Mild symptoms or ( nausea, confusion , disorientation, unsteady gait) asymptomatic ( mild neurocognitive symptoms, depression) Active therapy with either hypertonic saline or Tolvaptan Fluid restriction, if it fails or not tolerated, consider Tolvaptan Acute Hyponatremia Clinical Features • Seizures, coma, and respiratory arrests sometimes with little warning • Neurogenic pulmonary edema (hypoxia may increase severity of brain swelling) • Cerebral edema with herniation (particularly in young women and children) Brain CT Scans Normal Study Fatal Hyponatremia Causes of Acute Hyponatremia With Fatal Cerebral Edema • Self-induced water intoxication – Psychotic patients – Ecstasy (N-Methyl-3,4-methylenedioxyamphetamine) – Marathon runners – Radio contests • Post-operative iatrogenic hyponatremia Consensus Conference on Rx of Acute Hyponatremia in Marathon Runners Recommended Therapy: • In the field: 3% saline 100 ml over 10 minutes, repeated x 2 if needed • In hospital: 3% saline 100 ml or 1 ml/kg bolus followed by 100 ml/hr or 1-2 ml/kg/hr Hew-Butler, Clin J Sport Med 2008;18:111-121 Therapeutic Hypernatremia for Cerebral Edema • 30 ml bolus of 23.4% saline (equivalent to 238 ml 3% saline) • Serum Na = 5 mEq/L • Reversed clinical signs of brain herniation in most cases • Decreased intracranial pressure by 40% Koenig, MA. Neurology 70: 1023–1029, 2008 Hypertonic Saline for Seizures, Coma or Cerebral Edema: Data @ ≤ 4 hours Sterns, Semin Nephrol 29:282-299, 2009 Hypertonic Saline for Seizures, Coma or Cerebral Edema: Data @ ≤ 4 hours 4 to 6 mEq/L Increase Appears To Be “Enough” Sterns, Semin Nephrol 29:282-299, 2009 Acute vs Chronic Hyponatremia Acute Patients Duration Serum Na Stupor or Coma Seizures Mortality Low Na Deaths 14 < 12 hrs 112 ± 2 100% 29% 50% 36% Chronic 52 3 days 118 ± 1 6% 4% 6% 0% Data from Arieff, Medicine 56:121, 1976 (consults at one hospital in one year; Na < 128) Rapid Correction of Chronic Hyponatremia Causes Myelinolysis. 100% 80% 60% 40% 20% 0% 0 1.0 ± 0.1 2.8 ± 0.2 5.7 ± 0.4 Maximum Correction Rate (mEq/L/hr) Data from Verbalis KI 1991;39:1274 Inadvertent Overcorrection • Frequent readjustments of dose of 3% • 10% of patients given D5W or hypotonic fluid after d/c of 3% saline to offset an unexpected water diuresis • 1 patient given D5W and DDAVP Mohmand, et al. Clin J Am Soc Nephrol, 2:1110-7, 2007. Reversing Overcorrection D5W 3% NaCl 3% NaCl DDAVP 2 mcg q 6hrs 120 Serum Sodium (mmol/l) 115 110 105 Urine Osmolality (mOsm/kg) 100 600 80 700 700 700 700 95 0 12 24 36 Hours Sterns, R. Kidney Int August, 2009 48 60 72 Treatment of double-digit hyponatremia Richard H. Sterns,American Journal of Kidney Diseases, Vol 56, No 4 (October), 2010: pp 774-779 Teaching Points for Managing Profound Hyponatremia (1) • Prompt correction by enough to improve symptoms and reduce the risk of seizures – – – – 4-6 mEq/L is enough correction regardless of the severity of the hyponatremia Correct hyponatremia rapidly in the first few hours and then slow down • Limited correction to prevent neurologic injury (osmotic demyelination syndrome) – 10 mEq/L in a 24-hour period – 18 mEq/L in a 48-hour period • Stay well below these limits in patients at high risk of osmotic demyelination Teaching Points for Managing Profound Hyponatremia (2) • Anticipate and manage reversible causes of hyponatremia – Administration of desmopressin (dDAVP) every 68 hours with hypertonic saline solution is an effective strategy to control the rate of correction – Water intake and hypotonic intravenous fluids (including those containing medications) must be restricted in hyponatremic patients treated with desmopressin Correction Goals for Severe Chronic Hyponatremia • Rule of Sixes: – Six-a-day makes sense for safety – Six in six hours for severe sxs (symptoms) and stop • Explanation: • • • • For all patients with chronic hyponatremia, the goal is 6 mEq/L during the initial 24 hours. For those with severe symptoms (seizure, severe delirium, and unresponsiveness), postponing subsequent efforts to increase serum sodium level until the next day. HYPONATREMIA TREATMENT ALGORITHM EUVOLEMIC HYPONATREMIA (SIADH) LEVEL 3 - SEVERE SYMPTOMS: vomiting, seizures, obtundation, respiratory distress, coma hypertonic NaCl administration, followed by fluid restriction ± vaptan LEVEL 2 - MODERATE SYMPTOMS: nausea, confusion, disorientation, altered mental status vaptan or hypertonic NaCl administration, followed by fluid restriction fluid restriction, but vaptan under select circumstances: •inability to tolerate fluid restriction or LEVEL 1 - NO OR MINIMAL SYMPTOMS: headache, irritability, inability to concentrate, altered mood, depression failure of fluid restriction •very low sodium level (<125 mEq/L) with increased risk of developing symptomatic hyponatremia •need to correct serum [Na+] to safer levels for surgery or procedures, or for ICU/hospital discharge •unstable gait and/or high fracture risk •prevention of worsened hyponatremia with increased fluid administration •therapeutic trial for symptom relief tolvaptan: patient selection Dilutional hyponatremia1 Depletional hyponatremia2 total body sodium normal to increased total body water increased total body sodium decreased total body water decreased Hypervolemic1 Euvolemic1 (edema) (no edema) heart failure cirrhosis SIADH Hypovolemic2 Diarrhea Vomiting Burns Trauma Pancreatitis Diuretic excess Renal losses tolvptan CONTRAINDICATED [Na+] <125 mEq/L [Na+] ≥125 mEq/L may be used as initial therapy at discretion of MD must be: 1. symptomatic 2. resistant to fluid restriction for all patients receiving tolvaptan: • initiate and re-initiate treatment in a hospital • frequently monitor serum sodium serious neurological symptoms requiring raising [Na+] urgently tolvptan NOT INDICATED (avoid use of tolvaptan with hypertonic saline) 1. Douglas I. Cleve Clin J Med. 2006;73:S4-S12. 2. Kumar S. et al. Lancet. 1996;352:220-228. Dosing Recommendations for Samsca® (tolvaptan) • Initiate and re-initiate therapy only in a hospital Recommended dosage – Too rapid correction of serum [Na+] can cause serious neurologic sequelae • During initiation and after titration, frequently monitor for changes in serum electrolytes and volume • Start with 15 mg tablets once daily without regard to meals • Increase to 30 mg once daily after 24 hours to a maximum of 60 mg once daily as needed • Avoid fluid restriction during first 24 hours of therapy • Advise patients that they can and should drink fluid in response to thirst • Fluid restriction with Samsca may increase risk of dehydration and hypovolemia Samsca® (tolvaptan): Drug Interactions Agent Effects of Other Drugs on Samsca Ketoconazole 5-fold in tolvaptan exposure; greater in exposure with higher ketoconazole doses or highest labeled doses of other strong CYP 3A inhibitors Grapefruit juice 1.8-fold in tolvaptan exposure P-gp inhibitors tolvaptan dose may be required Rifampin and other CYP3A inducers 85% in tolvaptan exposure; tolvaptan dose may be required Lovastatin, digoxin, furosemide, hydrochlorothiazide Coadministration has no clinically relevant impact on tolvaptan exposure Effects of Samsca on Other Drugs Digoxin 1.3-fold in digoxin exposure Lovastatin lovastatin exposure, but not clinically relevant Warfarin, amiodarone, furosemide, hydrochlorothiazide No clinically important pharmacokinetic changes CYP 3A = Cytochrome P450 3A; P-gp = P-glycoprotein. Summary • Treatment of hyponatremia depends on the underlying cause, volume status, and duration of onset • Vasopressin is a key physiological hormone in body water homeostasis and, therefore, hyponatremia • Vasopressin receptor antagonists (“vaptans”) selectively increase solute-free water excretion by the kidneys • Tolvaptan is the first and only oral selective vasopressin V2 receptor antagonist to treat clinically significant nonhypovolemic hyponatremia