Neuromuscular Disorders - Calgary Emergency Medicine
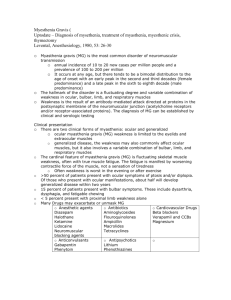
advertisement

Neuromuscular Disorders Ping-Wei Chen PGY – 2 Emergency Medicine Resident April 8, 2010 Thanks: Dr. Walker, Dr. Burton-MacLeod, Dr. Oster, Dr. Brownell Weakness • Non-Neuromuscular – – – – – – Cardiovascular Respiratory Infectious Metabolic Endocrine Toxicologic • Neuromuscular – – – – – – Brain Spinal Cord Anterior Horn Cell Peripheral Nerve Neuromuscular Junction Muscle Localizing the Lesion: UMN vs LMN • Upper motor neuron – Unilateral symptoms – If bilateral symptoms, associated • Altered mental status • Cranial nerve abnormalities – If bilateral symptoms and normal mental status • THINK spinal cord Localizing the Lesion: UMN vs LMN Reflexe s Spasticity Atrophy Fasciculations Babinski’s Nerve Conduction Testing Weakness Upper Motor Neuro n hyper yes no no upgoing normal yes Lower Motor Neuro n hypo no yes yes downgoing abnormal yes Myelopathy • Pathology of the spinal cord • Clinically: – UMN signs – Ascending weakness – Bowel/Bladder involvement – Sensory involvement (define level) Anterior Horn Cell • UMN synapses with LMN here • Clinically: – Both UMN/LMN signs – Little/No sensory involvement – Bulbar symptoms (ALS) • Speech • Swallowing • Chewing Neuropathy • Peripheral nerve pathology • Clinically: – LMN signs – Distal to proximal involvement • “glove and stocking” pattern – Varied sensory involvement Neuromuscular Junction • Connection between CNS and muscles • Clinically: – Variable presentations of weakness • Fatigability • Proximal • Ascending vs Descending – No sensory involvement Myopathy • Muscle pathology • Clinically: – LMN signs – Proximal > Distal – ±muscle tenderness Case • 65M with weakness. – 2x visits to GP in last 3 months for same. – Notices: • sometimes chokes on food • Blurry vision when tired • Generalized fatigue – “Enough is enough” • O/E: – Normal PERL – Rapid neurological exam otherwise normal. • Any thoughts? Myasthenia Gravis • RARE • Rarely diagnosed in ED • Bi-modal age of onset – Women 20-40 – Men 50-70 Neuromuscular Junction Myasthenia Gravis • Autoantibodies against Nicotinic ACh receptors – Decreased number of post-synaptic ACh receptors – Compete for binding on ACh receptors with ACh Myasthenia Gravis • Clinically: – Fatigability of voluntary muscles • BEWARE – respiratory muscles – Ocular symptoms first • Ptosis, diplopia, blurred vision – Normal sensation – No pain Myasthenia Gravis • Diagnosis – Clinical + Further Testing • • • • Edrophonium/Ice Bag Test Anti-ACh Receptor Antibody Muscle Specific Receptor Tyrosine Kinase Antibody Electrophysiologic Tests Myasthenic Crisis • MG + Respiratory failure requiring intubation – 15%-20% MG patients • Precipitants – Infection (most common) – Medication changes – Surgery – Pregnancy/Childbirth – Unidentified (30%) Back to our patient • When to intubate? Caution: Don’t rely on work of breathing! •Spirometry •FVC ≤ 1L = intubate •Rate of decrease in FVC •“sooner rather than later” Cholinergic Crisis • Excessive anticholinesterase medication – Too much Acetylcholine Acetylcholine Succinylcholine Myasthenic VS Cholinergic Crisis • May be difficult to differentiate – Response to Edrophonium/Ice Bag Test – Presence of muscarinic symptoms • Cholinergic crisis rare unless >> dose ingested – ie: pyridostigmine >120mg every 3 hours • Assume weakness 2o worsening MG Edrophonium/Tensilon Test • Edrophonium – 135mg IV – Response 30-90s? – Adverse effect? • Max dose 10mg IV • Caution – Asthmatics/COPD • Atropine at bedside!! • Measure distance between upper and lower eyelid in most affected eye Ice Bag Test • Apply ice to most affected eye X 2 mins • Measure distance between upper and lower eyelid in most affected eye Myasthenia Gravis • Management – Emergency Department • Identify • Supportive – Early intubation for respiratory failure – Neurology/ICU • Anti-cholinesterase Medications – Pyridostigmine • Immunomodulation – Plasmapheresis, IVIG – Glucocorticoids, Azathioprine, Mycophenolate Mofetil, Cyclosporine • Thymectomy Clinical Pearls • Do spirometry! – Insidious respiratory failure – FVC ≤1L = ICU consult, FVC≤500cc • Sick Myasthenia Gravis patient? – *Continue acetylcholinesterase inhibitor meds* • Admitting Myasthenia Gravis patient? – Neurology consult Case • 62M with known small cell lung Ca – Generalized leg weakness – Difficulty climbing stairs • Could this be Lambert-Eaton Syndrome? Lambert-Eaton Syndrome • RARE • Strong association with neoplasm (SCLC) • Auto-antibodies to Voltage Gated Ca channels – Decreased release of ACh from pre-synaptic terminal Lambert-Eaton Syndrome • Clinically: – Proximal muscle weakness (<MG) ± soreness – Autonomic dysfunction (anti-cholinergic) – Variable bulbar involvement • Differentiation from MG – Weakness improves with use of muscle – Autonomic involvement Case • 41yo male with nausea and diarrhea X 24 hrs • “really weak” – Difficulty holding head up for long periods – Arms weak • Blurred vision, dry mouth • ? “food poisoning” – moloha • Any thoughts? Botulism • Clostridium botulinum – Obligate anaerobe – Spore forming – Toxin producing • Mechanism of Action – Irreversible binding to presynaptic membrane of peripheral and cranial nerves • inhibiting ACh release – Disperses widely via vascular system regardless of portal of entry Botulism • Clinical Entities 1. 2. 3. 4. Food-borne Infantile Wound Adult Enteric Infectious Botulism/Adult Infectious Botulism of Unknown Source 5. Inhalational Botulism • Clinically: – Both voluntary and autonomic involvement – Symptom onset 6-48hrs post-ingestion of toxin • Descending, symmetrical paralysis • ±GI tract symptoms (N/V/D, abdo cramps, constipation) • ±Anti-cholinergic symptoms – Pupils dilated and non-reactive to light* • No sensory involvement • No pain • No fever *differentiates from myasthenia gravis Infantile Botulism • Clinically: – Constipation – Weak Cry – Feeding difficulties/Anorexia – Descending/Global Hypotonia – Lethargy Botulism • Diagnosis – Clinical Diagnosis (exclude other pathology) • Home canned foods, contaminated aquatic products, honey (infants) • Vegetables – Centre for Disease Control and Prevention 1998 • Suspect in • Adult with acute onset dysfunction of – GI tract – Autonomic nervous system (anticholinergic symptoms) – Cranial nerve dysfunction • Infant with acute onset of – – – – Poor feeding Diminished crying ability Weakness Respiratory distress Botulism • Diagnosis – Laboratory tests rarely helpful in initial management • Toxin/Spore Analysis – Serum, Stool, Vomitus, Food • Wound Cultures Management • Supportive Care – Early intubation for respiratory failure – Equine Trivalent Anti-toxin • • • • >1 year old Decrease mortality, disease duration (if given early) Unclear effect on ventilator dependence Side effects: serum sickness, anaphylaxis – Human Botulism Immune Globulin (BIG-IV) • <1 year old – Antibiotics in Wound Botulism • Penicillin G or Metronidazole (allergy) Case • 9yo male • 1 day history of: – Tripping when walking – Legs “feeling tight” • Seen by GP earlier; clinic note faxed – Neuro exam abnormalities • • • • 4+/5 strength bilaterally in lower extremities Sensation grossly normal Able to ambulate but “clumsy” Bloodwork normal – Go to ED if gets worse Case • • • • Now back: can’t walk or sit up independently “A cold” 3 weeks ago Otherwise healthy, IUTD O/E: – Normal cranial nerves – No sensory level – Decreased DTRs Video Exam Case • Bloodwork unremarkable – Electrolytes normal – No increased WBC • Other investigations? • Any thoughts? Guillain-Barre Syndrome • Most common cause of acute symmetrical weakness in developed countries • 1-2 per 100,000 worldwide • All ages affected – Peaks in young adults and elderly Guillain-Barre Syndrome • Heterogeneous syndrome with several variant forms – – – – Acute Inflammatory Demyelinating Polyneuropathy Miller-Fisher Syndrome Acute Motor Axonal Neuropathy Acute Sensorimotor Axonal Neuropathy • Autoimmune response to preceeding infection – Molecular mimicry – Campylobacter – HIV, EBV, CMV, H. influenza, E. coli Guillain-Barre Syndrome • Clinically: – Progressive, relatively symmetric muscle weakness • Usually ascending, then generalized – – – – Distal paresthesias Decreased/Absent deep tendon reflexes Dysautonomia Variable involvement • Facial muscles • Bulbar muscles • Cranial Nerves • Investigations: – Increased protein in CSF; normal white cell count Guillain-Barre Syndrome • Management – Emergency Department • Supportive – Early intubation for respiratory failure (15-30%) – Hemodynamic monitoring (autonomic dysfunction) – Neurology/ICU • Plasmapheresis • IVIG • No role for steroids Tick Paralysis • Summer months • Tick Endemic Areas – Pacific Northwest (BC) – Rocky Mountains • Injection of ixovotoxin with tick feeding – Diminish release of ACh – Slow nerve conduction velocity • Clinically: – Early: restless, irritable, hand/feet paresthesia – 24-48hrs: • ascending, symmetrical, flaccid paralysis • ±cerebellar dysfunction Tick Paralysis • Diagnosis: – Clinical; no diagnostic laboratory measure • Management: – Supportive Care • Early intubation for respiratory failure – Tick Removal Case • 46yo woman with ALS – 5 days of productive cough (clear, now green) – Fever 38.9oC today – No GI/GU symptoms • O/E: •HNT – normal •CV – tachycardic (115bpm) •Resp – RR46, SCM use, crackles R lung field •Abdo – soft, nontender, no CVA tenderness •MSK – no rashes Intubate? Amyotrophic Lateral Sclerosis • 1-3 per 100,000 • Sporadic and Familial forms • Increasing incidence after 40yo; peaks 7080yo • Clinically: – Progressive UMN/LMN symptoms (months/years) – Asymmetric weakness (distal to proximal) – No sensory findings Amyotrophic Lateral Sclerosis • Management – Supportive Care – Advanced Directive? • Moss et al. Chest. 1996 – Case Series (n=75) » 72% ALS patients aware of disease progression to respiratory failure » 48% ALS patients learned this from MD » 42% ALS patients made decision re: long term ventilation prior to crisis Questions?