Myasthenia Gravis: Diagnosis, Treatment and Anesthetic Implications
advertisement
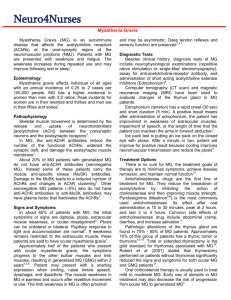
Terri Kueber, CRNA, MS Explain the pathophysiology and classification of Myasthenia Gravis (MG) List the signs and symptoms and clinical manifestation Describe the various treatments available for Myasthenia Gravis Discuss the anesthetic considerations for patients with Myasthenia Gravis Myasthenia Gravis is an autoimmune neuromuscular Consider a “Snowflake Disease” Cause is still unknown No known cure History Incident and prevalence is increasing with 5-10 per 100,000 25,000 cases in US Still considered sporadic Women versus men Often associated with other autoimmune disorders Class I: Ocular weakness, other muscle are normal Class II: Mild weakness affecting other muscle Class IIa: Muscles weakness affecting limbs and possibly oropharyngeal muscles Class III: Moderate weakness/severe ocular weakness Class IV: Severe weakness affecting limb muscle Class V: Defined by intubation Ocular Myasthenia Gravis Classic General Myasthenia Gravis Transient Neonatal Myasthenia Gravis Juvenile Myasthenia Gravis Congenital Types Drug-induced (Pencillamine, NDMR, aminoglycosides, procainamide) Bilateral or Unilateral Ptosis Diplopia Hoarseness Altered Speech Problems chewing Dysphagia Limited Facial Expressions Endrophonium (tensilon) Chloride Test 2.6-3.3 mg initial dose Neostigmine may be used in patients who do not respond to tensilon Auto-antibodies in MG – receptor binding antibodies are present in 80% of patients Thymic hyperplasia is present in 70% Electromyography (EMG) Testing Repetitive Nerve Stimulation (RNS) Single Fiber EMG (SFEMG) Ocular Cooling Other Testing Congenital Myasthenia Syndromes (not autoimmune) Drug induced MG Eaton-Lambert Syndrome (related to Small cell carcinoma of the lung) Hyperthyroidism (increases MG symptoms) Graves disease Botulism Ophthalmoplegia Intracranial pathology Fatigue or insufficient sleep Stress, anxiety, illness Overexertion, repetitive motion Pain or depression Low potassium or thyroid levels Alcoholic beverages Sudden fear, or extreme anger Extreme temperatures Humidity Sunlight or bright lights Hot foods or beverages Medications (beta blockers, antibiotics, calcium blockers) Chemicals such as household cleaner, insecticides, pet sprays, lawn chemicals Cholinesterase inhibitor Pyridostigmine – most commonly used Neostigmine – used less frequently Thymectomy Plasmapheresis Corticoid Steroid Therapy Immunosuppressive therapy (azathioprine, cyclosporine, etc.) Short-term Immunotherapy (IV immunoglobulin) Current health and symptoms PMH/PSH NMBA – Monitoring Post operative plan Pain control Induction and Extubation criteria 46 year old male diagnosis with MG in 6/2006 Presenting symptoms: fatigue and weakness after working out with intermittent dipoplia At time of diagnosis weakness lead to respiratory failure leading ventilation and respiratory support x 3 days Residual symptoms: weakness, pain and left ptosis Refractory to medical support under went a thymectomy in October 2009 Height/Weight: 75”/95=4.7 PFT’s FVC=65%, FEV1/FVC=61% Did not take his Pyridostigmine this am as he was instructed not to take it (not by anesthesia department) Gave Pyridostigmine 90 mg preoperatively IV Additional dose give at 1400 in recovery room Induction included: slow induction no neuromuscular blocking agents Total Agents included: Propofol 400mg Fentanyl 300 Morphine 4mg Midazolam 3 mg Intubation with glidescope secondary to NIM’s tube placement. Successfully extubated at end of case Received pyridostigmine in recovery room ICU overnight Discharge next day. 63 year old male Diagnosis between 12/05 and 2/06 Schedule for Laparoscopic Nissen Fundoplication Multiple drug allergies Ex-smoker (2 PPD x 30 years) H/O: MG controlled with medications, HTN, diet controlled, AST – normal with EF 55-65% Hiatal Hernia/Barrett’s Esophagus Previous surgery included: Brow lift, Laparoscopic Cholecystectomy Previous anesthetic records Surgeons desire muscle relaxation We did: Propofol 350mg Fentanyl 400 mcg Midazolam 2 mg Zofran/Decadron Ephedrine 15mg Vasopressin 2 units Patient’s was successfully extubated in OR and discharge home the next day Questions??