GLORIA Module 8: Anaphylaxis
advertisement
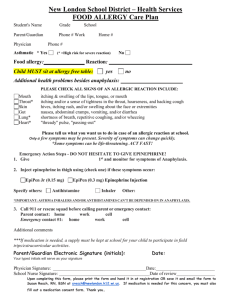
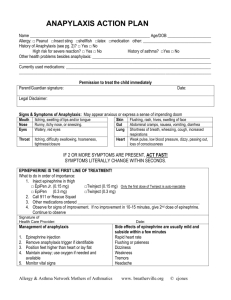
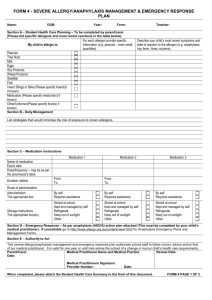
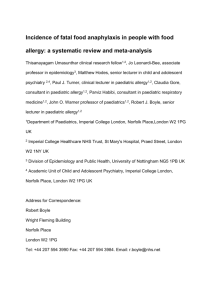
GLORIA Module 8: Anaphylaxis Updated: June 2011 Sponsored by an unrestricted educational grant from Global Resources in Allergy (GLORIA™) Global Resources In Allergy (GLORIA™) is the flagship program of the World Allergy Organization (WAO). Its curriculum educates medical professionals worldwide through regional and national presentations. GLORIA modules are created from established guidelines and recommendations to address different aspects of allergy-related patient care. World Allergy Organization (WAO) The World Allergy Organization is an international coalition of 89 regional and national allergy and clinical immunology societies. WAO’s Mission WAO’s mission is to be a global resource and advocate in the field of allergy, advancing excellence in clinical care, education, research and training through a world-wide alliance of allergy and clinical immunology societies GLORIA Module 8: Anaphylaxis WAO Expert Panel Richard F. Lockey, USA Michael A. Kaliner, USA F. Estelle R. Simons, Canada Cassim Motala, South Africa Bob Lanier, USA Additional contributor: Aziz Sheikh, UK Definition of anaphylaxis Anaphylaxis is a severe life-threatening generalized or systemic hypersensitivity reaction. It is commonly, but not always, mediated by an allergic mechanism, usually by IgE. Allergic (immunologic) non-IgE-mediated anaphylaxis also occurs. Non-allergic anaphylactic reactions, formerly called anaphylactoid or pseudo-allergic reactions, may also occur. Johansson SGO et al JACI 2004,113:832-6 Revised nomenclature for anaphylaxis Anaphylaxis Allergic anaphylaxis IgE- mediated anaphylaxis Johansson SGO et al JACI 2004,113:832-6 Non-allergic anaphylaxis Immunologic, nonIgE-mediated anaphylaxis Gell and Coombs classification of hypersensitivity Type I Type II Type III Type IV Immediate hypersensitivity Cytotoxic reactions Immune complex reactions Delayed hypersensitivity Anaphylaxis can occur through Types I, II and III immunopathologic mechanisms Kemp SF and Lockey RF. J Allergy Clin Immunol 2002;110:341-8 Mechanisms of allergic anaphylaxis …a severe, acute, systemic allergic reaction caused by the rapid, IgE-mediated release of potent mediators such as histamine from tissue mast cells and peripheral blood basophils Acutely released mediators of anaphylaxis • degranulation of mast cells and basophils causes the release of: - preformed granule-associated substances, eg histamine, tryptase, chymase, carboxypeptidase, and cytokines - newly-generated lipid-derived mediators, eg prostaglandin D2, leukotriene (LT) B4, LTC4, LTD4, LTE4, and platelet activating factor. Kemp SF and Lockey RF. J Allergy Clin Immunol 2002; 110:341-8 Primary symptoms of anaphylaxis • Skin: flushing, itching, urticaria, angioedema • Gastrointestinal: nausea, vomiting, bloating, cramping, diarrhea • Other: feeling of impending doom, metallic taste • Respiratory: dysphonia, cough, stridor, wheezing, dyspnea, chest tightness, asphyxiation, death • Cardiovascular: tachycardia, hypotension, dizziness, collapse, death Comments about anaphylaxis signs and symptoms • skin symptoms occur most commonly ( > 90% of patients) • skin, oral, and throat symptoms are often the first ones noted • respiratory symptoms occur in 40% to 70% of patients • gastrointestinal symptoms occur in about 30% of patients • shock occurs in about 10% of patients • signs and symptoms are usually seen within 5 to 30 minutes • the more rapid the onset, the more serious the reaction Lieberman P. In: Middleton’s Allergy: Principles and Practice, 6th edition, Mosby Inc., St. Louis, MO, 2003 Biphasic and protracted anaphylaxis • biphasic anaphylaxis is defined as return of symptoms after resolution of initial symptoms, without subsequent allergen exposure • usually, symptoms return within 1 to 8 hours (sometimes longer) • up to 20% of anaphylactic reactions are biphasic • patients with biphasic anaphylaxis may require more epinephrine to control initial symptoms • in protracted anaphylaxis, symptoms may be continuous for 5-32 hrs Lieberman P. Ann Allergy Asthma Immunol 2005;95:217-26 Biphasic/late-phase reaction Cellular infiltrates: 3 to 6 hours (LPR) Eosinophil Histamine CysLTs, GM-CSF, TNF-, IL-1, IL-3, PAF, ECP, MBP IL-4, IL-6 Allergen 3 to 6 hours Basophil Histamine, CysLTs, TNF-, IL-4, IL-5, IL-6 (CysLTs, PAF, IL-5) Monocyte PGs CysLTs Proteases Mast cell EPR 15 min (Early-Phase Reaction) CysLTs, TNF-, PAF, IL-1 Lymphocyte IL-4, IL-13, IL-5, IL-3, GM-CSF Return of Symptoms Differential diagnosis of anaphylaxis • vasovagal reactions • flushing • mastocytosis • carcinoid syndrome • hyperventilation syndrome • globus hystericus • hereditary angioedema • other types of shock, eg. cardiogenic, septic • scombroid poisoning Montanaro A and Bardana EJ Jr. J Investig Allergol Clin Immunol 2002;12:2-11 Incidence and prevalence of anaphylaxis • “anaphylaxis in the US: an investigation into its epidemiology" - on the basis of a literature review, more than 1.21% of the population may be affected • independent US Omnibus Studies (2002 and 2003) - 32 million have had 2 or more symptoms - 18 million diagnosed - 11 million have suffered a life-threatening reaction Neugut AI et al. Arch Intern Med 2001;161:15-21 Dey, L.P. Independent omnibus studies. Data on file. 2002-2003 Incidence and prevalence of anaphylaxis (cont.) • • • • 5-year review of 1.15 million persons in Manitoba, Canada dispensing patterns of epinephrine for out-of-hospital treatment 0.95% of the general population had epinephrine dispensed dispensing rates in the general population varied with age - 1.44% for individuals <17 years of age - 0.9% for those 17-64 years of age - 0.32% for those >65 years of age • interpretation: anaphylaxis from all triggers, occurring out of hospital, appears to peak in childhood, and then gradually decline Simons FER et al. J Allergy Clin Immunol 2002;110:647-51 International collaborative study of severe anaphylaxis • Objective • • To quantify the risk of anaphylaxis due to drugs and other exposures in hospital patients Methods • • • •Epidemiology Hospitals in Sweden, Hungary, India and Spain Incident cases 1992-1995 Clinical diagnosis using a priori agreed criteria, independent of presumed trigger 1998;9:141-46 International collaborative study of severe anaphylaxis (cont.) • Main findings • • • • • •Epidemiology 123/481,752 i.e. risk of 15-20/100,000 admissions 33% males Median age ~53 79% respiratory symptoms; 70% cardiovascular symptoms; 49% both Death in 2% of cases 1998;9:141-46 UK anaphylaxis death register • Objective • • To understand the circumstances leading to fatal anaphylaxis Methods • • • Running since 1992; ONS mortality data coded for anaphylaxis since 1993 Detailed information obtained from medical records, medical staff, coroners officers and mast cell serum tryptase Adrenaline rarely used before cardiac arrest Pumphrey RSH, Clin Exp Aller 2000; J Clin Pathol 2000; Novartis Found Symp 2004 UK anaphylaxis death register (cont.) • Main findings • • • • • ~20 recorded deaths/year i.e. ~1:2.8 million 50% iatrogenic; 25% food and 25% venom ~50% died from asphyxia (food) and 50% from shock (iatrogenic and venom) Median time to death: 5 mins if iatrogenic; 15 mins venom; and 30 mins food Adrenaline rarely used before cardiac arrest Pumphrey RSH, Clin Exp Aller 2000; J Clin Pathol 2000; Novartis Found Symp 2004 Hong Kong ED Objective To describe the epidemiology, clinical features and management of anaphylaxis Methods Retrospective review of all age patients in one ED, 19992003 Clinical diagnosis of anaphylaxis Main findings ~1/2800 attendances for anaphylaxis Smit DV et al. J Emer Med 2005;28:381-88 Agents that cause anaphylaxis: IgE-dependent triggers • • • • • foods (eg peanut, tree nuts, seafood) medications (eg, β-lactam antibiotics) venoms latex allergen immunotherapy • diagnostic allergens • exercise (with food or medication cotrigger) Kemp SF and Lockey RF, J Allergy Clin Immunol 2002;110:341-8 • hormones • animal or human proteins • colorants (insect-derived, eg. carmine) • enzymes • polysaccharides • aspirin and NSAIDs (possibly through IgE) Risk of anaphylaxis • estimated risk in US: 1-3% • fatalities per year in the US: - food-induced: 150 - antibiotic-induced: 600 - venom-induced: 50 Kemp SF and Lockey RF, J Allergy Clin Immunol 2002;110:341-8 Food-induced anaphylaxis • many anaphylactic reactions are caused by food - accidental food exposures are common and unpredictable - anaphylaxis from food can occur at any age, but children, teens and young adults are at highest risk • prevalence of peanut allergy has doubled in children <5 years of age in the last 5 years • seafood allergy is reported by 2.3% of the US population, and is more common in adults than in children Sampson HA. J Allergy Clin Immunol 2004;113:805-19 Sicherer SH et al. J Allergy Clin Immunol 2004;114:159-65 Most common food allergies • • • • • • • • peanut tree nut seafood fin fish milk egg soy wheat Fatal food-induced anaphylaxis • in a retrospective analysis of 32 deaths in patients age 2-33 years - peanut and tree nuts caused >90% of reactions - most patients had a history of asthma - most did not have injectable epinephrine available at the time of their reaction and death Bock SA et al. J Allergy Clin Immunol 2001;107:191-3 Hymenoptera stings • 0.5% to 5% of the US population is allergic to Hymenoptera venom(s) - bees - wasps - yellow jackets - hornets - fire ants • at least 50 deaths per year • incidence rising due to - increased numbers of fire ants and Africanized bees - increased numbers of people engaged in outdoor activities Neugut AI et al. Arch Intern Med 2001;161:15-21 Iatrogenic anaphylaxis • estimated 550,000 serious allergic reactions to drugs/year in US hospitals • most common drug triggers - penicillin (highest number of documented deaths from anaphylaxis) - sulfa drugs - non-steroidal anti-inflammatory drugs - muscle relaxants • most common biologic triggers - anti-sera for snakebite - anti-lymphocyte globulin - vaccines - allergens Neugut AI et al. Arch Intern Med 2001;161:15-21 Lazarou J et al. JAMA 1998;279:1200-5 Latex-induced anaphylaxis • <1% of the US general population • prevalence is highest among healthcare workers • latex gloves, especially if powdered, are a common trigger • repeated exposure leads to higher risk • incidence increased dramatically in the mid-1980s, but has decreased progressively with more use of non-powdered latex gloves and use of non-latex gloves Neugut AI et al. Arch Intern Med 2001;161:15-21 Peri-operative anaphylaxis • neuromuscular blocking drugs (muscle relaxants), eg suxamethonium, rocuronium, alcuronium, atracurium • induction agents, eg thiopentone, propofol, alfathesin • other: including local anesthetics, antibiotics, protamine, and latex • predisposing factors: atopy, asthma; previous exposure Fisher M. In: Anaphylaxis, John Wiley & Sons Ltd., Chichester, UK, 2004:193-206 Allergen immunotherapy-induced anaphylaxis • fatal reactions are uncommon: 1 per 2,000,000 injections • risk factors for fatality include: - dosing errors - poorly controlled asthma (FEV1 < 70%) - concomitant β-blocker use - lack of proper equipment and trained personnel - inadequate epinephrine treatment Stewart GE and Lockey RF. J Allergy Clin Immunol 1992;90:567-78 Bernstein DI et al, J Allergy Clin Immumol 2004;113:1129-36 Food-dependent exercise-induced anaphylaxis • reported in USA, Thailand and Japan • most commonly occurs in females, and from late teens to mid30’s • triggered by exercise 2-4 hours after ingesting offending food • foods implicated: wheat, seafood, fruit, milk,celery and fish. • associations: asthma, positive skin prick tests to foods • mechanism: two signals required Aunhachoke K et al. J Med Assoc Thai 2002;85:1014-8 Aihara Y et al. J Allergy Clin Immunol 2001;108:1035-9 Anaphylaxis from immune causes other than IgE • cytotoxic (Type II) - transfusion reactions to cellular elements (IgG, IgM) • immune aggregates (Type III) - intravenous immunoglobulin - Dextran (possibly) Kemp SF and Lockey RF, J Allergy Clin Immunol 2002;110:341-8 Anaphylaxis: non-immunologic causes MULTIMEDIATOR COMPLEMENT ACTIVATION/ACTIVATION OF CONTACT SYSTEM • radiocontrast media • ethylene oxide gas on dialysis tubing (possibly through IgE) • protamine (possibly) • ACE-inhibitor administered during renal dialysis with sulfonated polyacrylonitrile, cuprophane, or polymethylmethacrylate dialysis membranes Kemp SF and Lockey RF, J Allergy Clin Immunol 2002;110:341-8 Anaphylaxis: non-immunologic causes NONSPECIFIC DEGRANULATION OF MAST CELLS AND BASOPHILS • opiates • physical factors: - exercise (no food or medication co-trigger) - temperature (cold, heat) Kemp SF and Lockey RF, J Allergy Clin Immunol 2002;110:341-8 Idiopathic anaphylaxis • common in adults who are referred to allergists for evaluation of anaphylaxis • uncommon in children • negative skin tests, negative dietary history, no associated diseases eg. mastocytosis • preventive medication: oral corticosteroids, H1 & H2 antihistamines, anti-leukotrienes • deaths rare • may gradually improve over time Lieberman PL et al. J Allergy Clin Immunol 2005;115:S483-S523 Most common precipitating causes Country Precipitating agents USA Insect venom and drugs, immunotherapy, foods, radio contrast media, NSAID China, Korea Drugs - antibiotics and anesthetic agents India Australia China Japan Antibiotics, radio contrast agents and anesthetic agents plus blood products, insulin and growth hormones Peanuts Foods in children, insect stings, latex and drugs in adults De Bruyne JA and Lee BW. Allergy Clin Immunol Int: J World Allergy Org 2004;16:137-41 -Adrenergic blockade • by mouth or topically • paradoxical bradycardia, severe hypotension and bronchospasm • can exacerbate disease and impede treatment • selective β-blockers can produce clinically significant adverse respiratory effects even in mild-moderate asthma and COPD; not studied in anaphylaxis Lieberman PL et al. J Allergy Clin Immunol 2005;115:S483-523 Diagnosing anaphylaxis • clinical diagnosis based on clinical presentation and exposure history • flushing and tachycardia are invariably present, other cutaneous symptoms (hives, itch) may be absent • anaphylaxis may be difficult to diagnose, especially when patients present with bradycardia (instead of tachycardia, which is usual) • very rarely, patients present only with profound hypotension. The exposure to some inciting event is one key to the diagnosis in this rare circumstance Lieberman PL et al. J Allergy Clin Immunol 2005;115:S483-523 Diagnosing anaphylaxis (cont.) • careful history to identify possible causes • can be confirmed by an elevated serum tryptase level - specific for mast cell degranulation - remains elevated for up to 6 hours - may not be elevated, especially in food allergy • refer to allergist for specific testing Lieberman PL et al, J Allergy Clin Immunol 2005;115:S483-523 Laboratory tests in the diagnosis of anaphylaxis Plasma histamine Serum tryptase 24-hr Urinary histamine metabolite 0 30 60 90 120 150 180 210 240 270 300 330 Problems with laboratory tests • histamine and tryptase levels may not correlate with each other • histamine level was elevated in 42 of 97 patients in the Emergency Department, but only 20 of 97 had an elevated tryptase level • histamine levels also correlated better with symptoms and signs • plasma histamine levels only remain elevated for one hour after symptom onset; therefore, this test is usually not practical Lin RY et al. J Allergy Clin Immunol 2000;106:65-71 Diagnosing anaphylaxis Allergists can identify specific causes by: • complete and accurate medical/allergy history • skin tests/specific IgE levels - foods - insect venoms - drugs (some) • challenge tests: (selected patients, physician-monitored, preferably in hospital) - foods - NSAIDs - exercise Simons FER. J Allergy Clin Immunol 2006;117:367-77 Office management of anaphylaxis: checklist of equipment and drugs required • stethoscope and sphygmomanometer • tourniquets, syringes, needles (including large bore 14gauge) • injectable epinephrine (adrenaline) 1:1000 • oral airway and endotracheal tubes • oxygen, and equipment to administer it • diphenhydramine (or similar) injectable antihistamine • corticosteroids for IV injection • vasopressor (eg dopamine, noradrenaline) • glucagon • automatic defibrillator Physician-supervised management of anaphylaxis I. Speed is critical: a) assess airway, breathing, circulation, and mentation b) epinephrine, IM into the muscle of the anterolateral thigh; 1:1000 dilution, 0.3 - 0.5 mL (0.01 mg/kg in children); repeat, every 5-15 minutes as necessary. Kemp S and Lockey R. J Allergy Clin Immunol 2002;110:341-8 Simons FER et al. J Allergy Clin Immunol 1998;101:33-7 Simons FER et al. J Allergy Clin Immunol 2001;108:871-3 Physician-supervised management of anaphylaxis II. Secondary measures: a) place patient in recumbent position and elevate his/her legs b) maintain airway (endotracheal tube or cricothyrotomy) c) oxygen, 6 - 8 liters/minute d) normal saline IV; volume expanders (colloid solution) for severe hypotension Kemp SF and Lockey RF. J Allergy Clin Immunol 2002;110:341-8 Physician-supervised management of anaphylaxis III. Other measures: a) epinephrine 1:1000, ½ dose (0.1- 0.2 mg) into reaction site diphenhydramine, 50 mg IV or orally (1.25 mg/kg, up to 50 mg dose for children); maximum daily dose: adults 400 mg; children 200 mg b) ranitidine, 50 mg in adults and 12.5 - 50 mg (1 mg/kg) in children, dilute in 5% D/W, total 20 ml, inject slowly IV, over 5 minutes (cimetidine 4 mg/kg OK for adults, dose not established for children) Kemp SF and Lockey RF. J Allergy Clin Immunol 2002;110:341-8 Physician-supervised management of anaphylaxis • for bronchospasm - nebulized albuterol (salbutamol) 2.5 - 5 mg in 3 ml normal saline • for refractory hypotension - dopamine, 400 mg in 500 ml normal saline IV 2 - 20 μg/kg/min - glucagon, 1- 5 mg (20 - 30 μg/kg, max 1 mg in children), IV over 5 minutes followed with continuous IV infusion 5-15 μg/min - methylprednisolone, 1- 2 mg/kg per 24 hr Kemp SF and Lockey RF. J Allergy Clin Immunol 2002;110:341-8 Measures to reduce the incidence of drug-induced anaphylaxis General measures • obtain detailed history of previous adverse reactions to drugs • avoid drugs that cross-react with any agents to which patient is sensitive • administer drugs orally rather than parenterally when possible • check all drugs for proper labeling • monitor patients closely for 20 to 30 minutes after injections Lieberman P. In: Middleton’s Allergy: Principles and Practice, 6th edition, Mosby Inc., St. Louis, MO, 2003 Measures to reduce the incidence of anaphylaxis • identify causative factors; provide specific instructions about avoidance • have patient wear Medic Alert® or carry other medical identification • teach self-injection of epinephrine and caution patients to keep it with them at all times • repeat instructions each year • re-evaluate use of -adrenergic blocking agents, ACE inhibitors, monoamine oxidase inhibitors, and tricyclic antidepressants Simons FER, J Allergy Clin Immunol 2006;117:367-77 Measures to reduce the incidence of anaphylaxis Use preventive techniques when patients need to undergo a procedure or take an agent which places them at risk, such as: - pretreatment - provocative challenge (selected patients, physician-monitored, preferably in hospital) - desensitization (selected patients, physician-monitored, preferably in hospital) Lieberman P. In: Middleton’s Allergy: Principles and Practice, 6th edition, Mosby Inc., St. Louis, MO,2003Q Prevention of anaphylactic reactions to radiocontrast media (RCM) in adults • • • • prednisone 20-50 mg orally 12,7, and 1 hours before administration of RCM diphenhydramine 50 mg orally/intramuscularly 1 hour prior to RCM ephedrine 25 mg orally 1 hour before RCM administered another approach: - give oral non-sedating H1antihistamine and H2 antihistamine at 12 and 1 hours before exposure Lieberman P et al. J Allergy Clin Immunol 2005, 115:5483-5523 Specific advice for food-induced anaphylaxis: patient education • teach patients about risk management • complete avoidance of a food is difficult • patients must always be prepared with: - a written Anaphylaxis Emergency Action Plan - self-injectable epinephrine (adrenaline) - Medic Alert®-type identification Sampson HA, J Allergy Clin Immunol 2004;113:805-19 Simons FER, J Allergy Clin Immunol 2006;117:367-77 Specific advice for food-induced anaphylaxis: patient education • teach patients to avoid allergens - read product labels - identify alternative names for ingredients - identify “hidden” ingredients • avoid high-risk foods (eg baked goods) and high-risk situations (eg buffets) • avoid sharing food, utensils, or dishes - minute amounts of allergen can be life-threatening • provide educational materials, available from Food Allergy and Anaphylaxis Network - FAAN (www.foodallergy.org) Sampson HA, J Allergy Clin Immunol 2004;113:805-19 Simons FER, J Allergy Clin Immunol 2006;117:367-77 Venom-induced anaphylaxis • normal reactions: local pain, erythema, mild swelling - large local reaction: extended swelling, erythema • anaphylaxis: usual onset within 5-30 minutes - cutaneous: pruritus, urticaria, flushing, angioedema - respiratory: dyspnea, wheezing, stridor, dysphonia - cardiovascular: tachycardia, hypotension, dizziness, faintness • in a patient who has already experienced anaphylaxis from a sting, the risk of anaphylaxis to a subsequent sting is 30%-60% Freeman TM, N Eng J Med 2004;351:1978-84 Specific advice for venom-induced reactions: Patient education • teach patients methods of risk reduction (avoidance strategies) • keep injectable epinephrine on hand at all times, in key locations • develop a written emergency action plan, and update it yearly • always wear a Medic Alert®-type identification • consult an allergist to determine need for venom immunotherapy Freeman TM, N Eng J Med 2004;351:1978-84 Simons FER. J Allergy Clin Immunol 2006;117:367-77 Specific advice for venom-induced reactions: immunotherapy • medical criteria - history of any systemic reaction in adults - history of life-threatening reaction in children - positive venom skin test or increased specific IgE level • therapy is >97% effective - less than 3% risk for systemic reaction to subsequent stings vs 30% to 60% risk without immunotherapy Golden DBK, N Eng J Med 2004:351:668-74 Moffit JE et al. J Allergy Clin Immunol 2004;114:869-86 Factors affecting prognosis Factor Poor Prognosis Good Prognosis Onset of symptoms Early Late Initiation of treatment Late Early Route of exposure Injection Oral* β-adrenergic blocker use Yes No Presence of underlying disease Yes No * true for drugs, not foods Anaphylaxis in the emergency department • chart review study in 21 North American Emergency Departments • random sample of 678 charts of patients presenting with food allergy • management: - 72% received antihistamines - 48% received systemic corticosteroids - 16% received epinephrine (24% of those with severe reactions) - 33% received respiratory medication (eg. inhaled albuterol) - only 16% received Rx for self-injectable epinephrine at discharge - only 12% referred to an allergist Clark S et al. J Allergy Clin Immunol 2004;347-52 Referral to allergy/immunology specialist • risk assessment: detailed history; coordinate allergy tests and other investigations • risk management: - patient education (about allergen avoidance measures) - medication review - self-administered epinephrine - immunotherapy (for hymenoptera allergy) - premedication (for idiopathic anaphylaxis) - new therapies Simons FER, J Allergy Clin Immunol 2006;117:367-77 Important resources • • • • • • • www.foodallergy.org www.latexallergyresources.org www.aaaai.org www.acaai.org www.worldallergy.org resources for: patients, families, health-care professionals practical advice, up-to-date scientific information, promotion of research, legislation, etc. Summary • anaphylaxis: release of inflammatory mediators from mast cells and basophils (IgE-mediated or non-IgE mediated) • symptoms: within minutes of exposure to triggering agent (less commonly can be delayed, biphasic or protracted) • common triggers: foods, drugs, latex, hymenoptera stings; idiopathic • first-line of treatment: injected epinephrine (adrenaline) • hallmarks of management: education and prevention World Allergy Organization (WAO) For more information on the World Allergy Organization (WAO), please visit www.worldallery.org or contact the: WAO Secretariat 555 East Wells Street, Suite 1100 Milwaukee, WI 53202 United States Tel: +1 414 276 1791 Fax: +1 414 276 3349 Email: info@worldallergy.org