Western PA HFMA & Three Rivers AAHAM, Winter Education Conference
“If only we had known sooner the patient
couldn’t pay that much,” AKA: “Woulda,
Shoulda, Coulda”
Larry Estes
TransUnion Healthcare
Then
Where we’ve been.
Now
Where we are.
Today
What is changing around us?
Next
What if we don’t make a change?
How did 2013 go?
• Exceed hospital’s patient access and revenue cycle KPI
goals?
• Exceed National Benchmarks/Best Practices?
• Sitting on extra money?
• Making CFO happy?
Clinical diagnosis
Determine symptoms via questions
Collect data
• History
• Test results
Deliver treatment plan
• Wrong treatment?
Lost time = patient gets worse before getting better!
Financial diagnosis
Determine symptoms via questions & data
•
•
•
ID, Insurance Eligibility, Estimation
History
Financial Information (Bad Debt?)
Deliver financial plan
• Wrong treatment?
Lost Time = lost revenue/increased expenses (or - hospital gets worse…)
In conjunction with
shifting plan
designs, lower
reimbursement rates
Consumer-directed
health plans now more
popular
than HMOs
Rising
patient outof-pocket
costs
Reduced
reimbursements
Challenging
how
healthcare
operates
Increasing
bad debt
Patients are responsible
for greater portion of
medical costs =
increase
in bad debt
Stagnant
revenue
growth
Patients are
forgoing lucrative
elective procedures
Critical Business Issues: Pre-Service
Process
Critical Business Issues
Financial Clearance – WHY?
Determining the patient’s ability-to-pay and if they qualify for financial
assistance is a key driver for increased collections at the POS
Point-of-Service
Collections
• Self-pay balances continue to rise
• Traditional collection rates are stagnant or decreasing
• Macro economic factors (unemployment, etc.) are increasing the
need for more effective POS collections
• Difficulty determining which patients have the ability, capacity and
propensity to pay
Charity and Financial Aid Screening – WHY?
Matching uninsured or underinsured patients to the appropriate
funding sources is a critical revenue source
Financial
Counseling
• Numerous programs and requirements
• Tedious manual processes to qualify and enroll patients into
appropriate programs
• Lack of patient involvement to provide supporting financial
information
6
© 2010 TransUnion LLC All Rights Reserved
Critical Business Issues: Post-Service
Process
Medicaid
Re-Verification
Critical Business Issues
Identify Self-Pay Accounts that were Enrolled in Medicaid at the
Date of Service – WHY?
Recover reimbursements from self-pay accounts that were
previously thought to be uninsured
• Difficulty identifying all Medicaid coverage at registration
• Lost reimbursements from accounts that will most likely roll to bad
debt
• Identify opportunities for future billing based upon current coverage
Discern true charity care from bad debt – WHY?
Address IRS 990 Schedule H reporting requirements
• Accurately report and track charitable giving
Charity
Determination
• Lack of patient involvement to provide supporting financial
information
• Inability to identify patients truly in need – resulting in wasted
collection efforts
• Could/Should be Pre-Service, too!
7
© 2010 TransUnion LLC All Rights Reserved
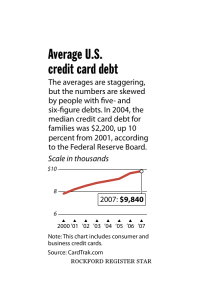
• 2.5 statements before a patient begins to pay the hospital
• 50% of an insured patients’ balance becomes bad debt1
• 90% of an uninsured patients’ balance becomes bad
debt1
= $60 Billion in bad debt/year
1Source:
McKinsey Quarterly, June 2007, “Overhauling the US healthcare payment
system”
Nick A. LeCuyer and Shubham Singhal
Guess What?
• Annual Out-of-Pocket for Families Covered by EmployerSponsored Insurance
1
= $4,316
• Covered Workers with Deductible >$1,000
= 34%1
1Source:
The 2012 Employer Health Benefits Survey, the Kaiser Family Foundation and the Health
Research and Educational Trust (HRET), September 2012.
Challenges in 2014 –
Déjà Vu all over again
• Rising patient deductibles – at even faster pace
• Higher co-pays
• More patients than ever
– Newly Insured:
• “I owe money? But I have insurance!”
– Always Been Insured:
• “I owe money? But I have insurance!”
• Insured? Not insured?
– ACA Premiums Paid? 90 day grace period? (This should be fun.)
• Lower reimbursements
• Bad Debt vs. Charity Care
With ACA HIE’s (A-OK?)
Deductible*
Patient CoInsurance
Patient Out of
Pocket
Bronze 1
$4,375
20%
$6,350
Bronze 2
$3,475
40%
$6,350
Silver 1
$2,050
20%
$6,350
Silver 2
$650
40%
$6,350
*Deductible doubled for family1!
1Source:
Act”
Kaiser Family Foundation, April 2012, “Patient Cost-Sharing Under the Affordable Care
Woulda, Shoulda, Coulda
• “A bird in the hand is worth two in the bush.”
– John Ray's A Hand-book of Proverbs, 1670
• “Too soon old and too late smart.”
– Pennsylvania Dutch saying
• “Hindsight is always 20/20.”
– Virtually every politician ever elected.
• “If I had only known….”
– Former Employee
• “If only I knew then what I know now.”
– Anyone who ever made past age 30.
• “D’oh!”
– Homer Simpson
How will you react?
• Insanity: doing the same thing over and over again and
expecting different results. - Albert Einstein
I know! Let’s Have a Meeting!
• “We can tweak our process to make it work!”
• “Let’s come up with some ideas for next year.”
• Goes something like this….
• One Thing Leads to Another
• “If You Give a Mouse a Cookie…”
External Data
• Are they them?
– Are they giving me an accurate name,
address, phone number, SSN and date
of birth?
• Insurance?
?
?
?
?
?
?
?
?
?
?
?
?
?
?
?
?
?
?
?
?
• How much will it be?
• Can they pay POS?
• Will I (can I?) collect on the backend?
• Eligible for financial assistance?
17
© 2010 TransUnion LLC All Rights Reserved
External Data = Financial Diagnosis = Options
18
FPL < 100% with
no insurance
Potential charity
care or Medicaid
Strong ability to pay
with nominal copay
Collect payment
at time of service
Identity issues
Potential fraud
Borderline ability to pay
with large deductible
Consider for
financing solutions
© 2010 TransUnion LLC All Rights Reserved
1. One-stop shops
▪ Ask questions
Who owns the financial data you’re buying?
Who maintains, updates software, loads payer contracts, history?
Where do they get eligibility info?
▪ Big companies usually will, but remind niche companies to accept
responsibility
One contract, One contact
2. Best in Breed
▪ How well do they play together?
▪ Seamless data transmission can happen among better vendors, but may mean
separate contracts and contacts.
3. Considered an Investment, not Expense!
Physician EMR or
Portal
Work List Manager / Rules Engine / Data Audit / Exception Manager
3
Text?
Reporting/Dashboard
Accept
Appointment
Automation
ID and Address
Verification
Eligibilty
Estimation
Full Patient Financial
Discussion
Patient Responsibility
Credit Report/ Financial
Analysis
Insurance Authorization
Medical Necessity
Charity Assessment
HIS Integration
SelfService
Kiosk
e-cashiering/
Payment
Plan
Admitted/
Procedure
Discharge
The Key? Build Your Process to Stay
Ahead of the Game…
• The Chocolate Factory
Pieces and Data needed to know your
Patient and “treat” efficiently
•
•
•
•
•
•
•
•
Registration Accuracy
Insurance Eligibility
Financial Analysis
Charity Assessment
Payment Estimation
Payment Processing
Patient Loans
Bad Debt Risk
Oh, and • Stay Ahead of the Game!
Larry Estes
Regional Sales Executive
TransUnion Healthcare
lestes@transunion.com
(717) 275-2484
www.transunionhealthcare.com
23