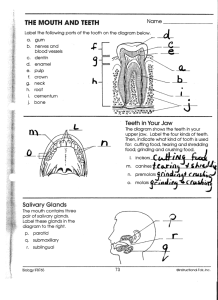
Salivary Glands
advertisement
Salivary Glands Major glands • Parotid: so-called watery serous saliva rich in amylase, proline-rich proteins – Stenson’s duct • Submandibular gland: more mucinous – Wharton’s duct • Sublingual: viscous saliva – ducts of Rivinus; duct of Bartholin Minor glands • Minor salivary glands are not found within gingiva and anterior part of the hard palate • Serous minor glands=von Ebner below the sulci of the circumvallate and folliate papillae of the tongue • Glands of Blandin-Nuhn: ventral tongue • Palatine, glossopalatine glands are pure mucus • Weber glands Functions • Protection – lubricant (glycoprotein) – barrier against noxious stimuli; microbial toxins and minor traumas – washing non-adherent and acellular debris – formation of salivary pellicle • calcium-binding proteins: tooth protection; plaque Functions • Buffering (phosphate ions and bicarbonate) – bacteria require specific pH conditions – plaque microorganisms produce acids from sugars Functions • Digestion – – – – neutralizes esophageal contents dilutes gastric chyme forms food bolus brakes starch Functions • Antimicrobial – lysozyme hydrolyzes cell walls of some bacteria – lactoferrin binds free iron and deprives bacteria of this essential element – IgA agglutinates microorganisms Functions • Maintenance of tooth integrity – calcium and phosphate ions • ionic exchange with tooth surface Functions • Tissue repair – bleeding time of oral tissues shorter than other tissues – resulting clot less solid than normal – remineralization Functions • Taste – solubilizing of food substances that can be sensed by receptors – trophic effect on receptors Embryonic development • The parotid: ectoderm (4-6 weeks of embryonic life) • The sublingual-submandibular glands: endoderm • The submandibular gland around the 6th week • The sublingual and the minor glands develop around the 8-12 week • Differentiation of the ectomesenchyme • Development of fibrous capsule • Formation of septa that divide the gland into lobes and lobules Serous cells • Seromucus cells=secrete also polysaccharides • They have all the features of a cell specialized for the synthesis, storage, and secretion of protein – Rough endoplasmic reticulum (ribosomal sites->cisternae) – Prominent Golgi-->carbohydrate moieties are added Secretory granules-->exocytosis Serous cells • The secretory process is continuous but cyclic • There are complex foldings of cytoplasmic membrane • The junctional complex consists of: – Tight junctions (zonula occludens)-->fusion of outer cell layer – Intermediate junction (zonula adherens)-->intercellular communication – Desmosomes-->firm adhesion Mucous cells • Production, storage, and secretion of proteinaceous material; smaller enzymatic component -more carbohydrates-->mucins=more prominent Golgi -less prominent (conspicuous) rough endoplasmic reticulum, mitochondria -less interdigitations Formation and Secretion of Saliva • Primary saliva – Serous and mucous cells – Intercalated ducts • Modified saliva – Striated and terminal ducts – End product is hypotonic Macromolecular component • Synthesis of proteins • RER, Golgi apparatus • Ribosomes RER posttranslational modification (N- & O-linked glycosylation) Golgi apparatus Secretory granules • Exocytosis • Endocytosis of the granule membrane Fluid and Electrolytes • Parasympathetic innervation • Binding of acetylcholine to muscarinic receptors – Activation of phospholipase IP3 release of Ca2+ opening of channels K+, Cl- Na+ in – K+ and Cl- in – Also another electrolyte transport mechanism through HCO3- • Noepinephrine via alpha-adrenergic receptors – Substance P activates the Ca2+ Myoepithelial cells • One, two or even three myoepithelial cells in each salivary and piece body • Four to eight processes • Desmosomes between myoepithelial cells and secretory cells • Myofilaments frequently aggregated to form dark bodies along the course of the process Myoepithelial cells • The myoepithelial cells of the intercalated ducts are more spindled-shaped and fewer processes • Ultrastructurally very similar to that of smooth muscle cells • Functions of myoepithelial cells – Support secretory cells – Contract and widen the diameter of the intercalated ducts – Contraction may aid in the rupture of acinar cells of epithelial origin Intercalated Ducts • • • • Small diameter Lined by small cuboidal cells Nucleus located in the center Well-developed RER, Golgi apparatus, occasionally secretory granules, few microvilli • Myoepithelial cells are also present • Intercalated ducts are prominent in salivary glands having a watery secretion (parotid). Striated Ducts • • • • Columnar cells Centrally located nucleus Eosinophilic cytoplasm Prominenty striations – Indentations of the cytoplasmic membrane with many mitochondria present between the folds • Some RER and some Golgi, short microvilli • Modify the secretion – Hypotonic solution=low sodium and chloride and high potassium • Basal cells Terminal excretory ducts • Near the striated ducts they have the same histology as the striated ducts • As the duct reaches the oral mucosa the lining becomes stratified • Goblet cells, basal cells, clear cells. • Alter the electrolyte concentration and add mucoid substance. Ductal modification • Autonomic nervous system • Striated and terminal ducts • Modofication via reabsorption and secretion of electrolytes • Final product is hypotonic • Rate of salivary flow – High: Sodium and chlorine up; potassium down Connective tissue • • • • • Fibroblasts Inflammatory cells Mast cells Adipose cells Extracellular matrix – Glycoproteins and proteoglycans • Collagen and oxytalan fibers • Blood supply Nerve supply • • • • No direct inhibitory innervation Parasympathetic and sympathetic impulses Parasympathetic are more prevalent. Parasympathetic impulses may occur in isolation, evoke most of the fluid to be excreted, cause exocytosis, induce contraction of myoepithelial cells (sympathetic too) and cause vasodilatation. Nerve supply • There are two types of innervation: Epilemmal and hypolemmal • beta-adrenergic receptors that induce protein secretion • L-adrenergic and cholinergic receptors that induce water and electrolyte secretion Hormones can influence the function of the salivary glands. They modify the salivary content but cannot iniate salivary flow. Age changes • Fibrosis and fatty degenerative changes • Presence of oncocytes (eosinophilic cells containing many mitochondria) Clinical Considerations • • • • • • Obstruction Role of drugs Systemic disorders Bacterial or viral infections Therapeutic radiation Formation of plaque and calculus