DSM IV Diagnosis in Mental Health Work
advertisement

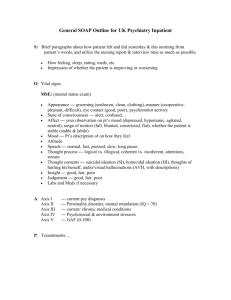
Mental Status Assessment Adapted from Casey Barrio, Ph.D. University of North Texas Amy McCortney, Ph.D., LPC-S, NCC DSM IV-TR and the DSM 5 • Note: – DSM III, DSM IV, and DSM IV-TR all included the use of multiaxial diagnosis, a practice that was widely adopted in assessment and managed care – The DSM 5 is intended to be a “non-axial” or more holistic view of biopsychosocial functioning – However, it is likely many assessment methods, as well as insurance forms, will continue to include the multiaxial format through a transition time. Multiaxial Evaluation (review) Axis I Clinical disorders Other conditions that may be focus of clinical attn • Includes all current disorders except – Personality disorders – Mental retardation • • • • List principal diagnosis first List all Axis I Include major stressors if focus Ok to defer or assign no diagnosis Axis II Personality disorders Mental Retardation • Includes – Personality disorders – Mental retardation – Personality traits – Defense mechanisms • Note if principal reason • List all Axis II • OK to defer to assign no diagnosis Axis III General Medical Conditions • Relevant to understanding or management – – – – – – Directly causes disorder (xx due to yy) Causes d/o to worsen D/o is a reaction to medical dx Choice of meds is influenced Management or safety is issue Incidental • Specify – “None” if none – “Deferred” if in progress – “By patient history” if not formal Axis IV Psychosocial and environmental problems • May include problems that… – affect dx, tx, prognosis – Put one at risk for mental d/o – are a result of mental d/o • Include – Relevant in past year – Very salient context/history • If focus, also gets coded on Axis I • Often include “mild” “moderate” “severe” Axis IV Psychosocial and environmental problems • Primary support group • Housing • Social environment • Health care • Educational • Legal system • Occupational • Others • Economic Axis V Global Assessment of Functioning (GAF) • Level of psych, soc, and occ functioning • 100-point scale includes attention to – Severity – Functioning • Rate – current period (lowest past week) – past year – discharge/termination Axis V Global Assessment of Functioning (GAF) • Often used to determine level of care • Generally… – 50-70 Outpatient – 30-50 Intensive outpatient/partial hosp – 1-30 Inpatient Severity & Course Specifiers • Mild Few symptoms in excess of min; minor impair • Moderate • Severe Many symptoms in excess, several particularly severe symptoms, marked impairment • Partial remission • Full remission • Prior history Axis V Determining a GAF Score (p. 34) • Start at top and use “EITHER OR” logic Is either severity OR level of functioning worse? • Move down until range matches severity OR functioning (WHICHEVER WORSE) • Go one lower to make sure both are TOO SEVERE • Determine SPECIFIC number within 10-point range In a nutshell… Communicating severity and impairment • DSM-IV severity specifiers (Axis I) • Co-morbid personality disorders (Axis II) • Co-morbid medical conditions (Axis III) • Listing all stressors (Axis IV) • GAF (Axis V) Checking in… Why do counselors assess? When do counselors assess? How do counselors assess? Mental Status Exam Purpose & Overview • Standard practice at most agencies – Crisis situations – Necessity of treatment / level of care – Managed care requirements • Provides baseline • Assists in documentation Purpose & Overview con’t • Generally adjunct to intake • Ongoing observation & integrated assessment • What’s not present is as important as what is • Objective measure (SOAP) although some assessment (SOAP) Overview of MSE areas • • • • • • • • • Appearance Motor Speech Affect Thought content Thought process Perception Intellect Insight Assess all items based on current observations The very basic… • Orientation x4 – Person – Place – Time – Situation AKA “Oriented x4” Appearance • • • • • • • Age Sex, race Build Position Posture Dress Grooming • Manner • Distinguishing features • Prominent physical abnormalities • Emotional facial expression • Alertness Behavior • Eye contact • Habits • Movements • Willingness to respond • Attitude toward counselor • Evidence of internal stimuli Motor • Retardation (slowed) • Agitation • Abnormal movements • Gait • Catatonia Speech • Rate • Volume • Amount • Articulation (clarity) • Spontaneity • Changes in patterns Affect • Stability • Range (long-term, immediate) • Appropriateness • Intensity • Affect (outward appearance) • Mood (internal - self-report) Thought Content • Suicidal ideation • Phobias • Death wishes • Ideas of reference • Homicidal ideation • Paranoid ideation • Depressive cognitions (guilt, worthlessness) • Magical ideation • Obsessions • Ruminations • Delusions • Overvalued ideas • Other major themes Thought Process • Stream • Associations (flight of ideas, loose) • Coherence • Logic • Clang associations (rhyming/pattern) • Perseverative (repetition) • Neologism (new words) • Blocking (interruption in flow) • Attention Perception • Hallucinations (all 5 senses) • Illusions • Depersonalization (of self) • Derealization (of outside world) • Déjà vu • Jamais vu (French, “never seen”)disfamiliarity Other MSE observations • Approximate IQ • Insight – Awareness of problem & self • Judgment – Ability, given info, to make sound decisions • Impulse control – Ability for person to control/resist urges Biopsychosocial History Purpose of Intake Interviews (Seligman, 2004) • Determine suitability for services • Assess urgency of situation • Familiarize person with process • Elicit positive attitudes toward counseling • Gather information for dx and tx plan Variables to consider • Information gathering methods • Depth & duration • Client needs – Referral source – Presenting problem – Urgency – Motivation & functioning Skills for intake interviewing • Establish rapport • Educate regarding process – Goals and expectations – This session different from others • Balance – Open-ended ? for perspective – Closed-ended ? for efficiency – Reflections & encouragers • Descriptive Empathy • Directness / assumptions may help Major areas of assessment • • • • • • • • • Identifying information Presenting problem(s) Other current problems and previous difficulties Present life situation Family of origin Current family Developmental history Medical & counseling history See Seligman (2004) Additional information AND Zimmerman psychosocial outline Intake Reports • Identifying information • Overview of presenting problem, symptoms, impact on person • Mental Status Exam • Other problems and difficulties • Present life situation • Information on family of origin and present family Intake Reports (con’t) • Developmental history, important incidents • Medical and treatment history • Case conceptualization including strengths and areas of difficulty • Multiaxial diagnosis • Treatment plan and other recommendations • Conclusion and summary