Alterations in Fluid, Electrolyte and Acid
advertisement

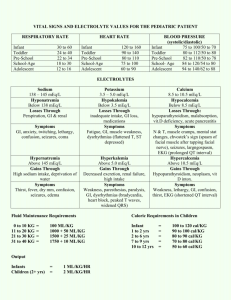
Fluid and Electrolyte Imbalance Jianzhong Sheng MD, PhD Water Body fluids • Extracellular fluids (ECF) – Interstitial fluid - fills the spaces between most cells of the body – Intravascular fluid - plasma (WBC, RBC and platelets in this fluid) Body fluids • Intracellular fluids (ICF) – Liquids within cell membranes – 40% of body weight Components in body fluids • Electrolyte – an element that when dissolved can carry an electrical current – Cations - (+) ; Anions - (-) – neuromuscular function – acid-base balance – ingested compounds – serve as catalysts in nerve response, muscle contraction, and metabolism of nutrients in foods, regulate electrolyte balance Movement of body fluids • Diffusion – Area of higher concentration to an area of lower concentration till even distribution • Osmosis – Movement of a pure solvent, e.g. water through a semipermeable membrane from a solution that has a lower solute concentration to one that has a higher solute concentration Osmotic pressure • Drawing power of water (dependent on the number or molecules in solution) – Isotonic – Hypotonic – Hypertonic Movement of body fluids • Filtration – Water and diffusible substances move together in response to fluid pressure • Active transport – Requires energy – Able to move larger molecules and go from less to greater concentration Transmembrane water permeability Bilayer Diffusion Aquaporin Water Channels Hard to explain All biological membranes Renal tubules, secretory glands, red cells Low capacity High capacity for H2O, not H3O+ Bi-directional Directed by osmotic gradients Unknown inhibitors Reversibly inhibited by Hg++ Discovery of Aquaporin-1 A serendipitous observation Contaminant in 32 kDa Rh preparations Simple purification Atypical staining Insoluble in N-lauroylsarc. 200,000 copies per red cell Channel-like homotetramer Protein sequence 1-35 aa Denker et al., J Biol Chem, 1988 Smith & Agre, J Biol Chem, 1991 Discovery of Aquaporins-AQP1 Functional expression (with Wm. Guggino at JHMI) Hypo-osmolar swelling Hg++ inhibited, no currents Xenopus oocyte, CHIP28 Preston et al., Science 1992 Peter Agre & Roderick MacKinnon Nobel Prize---10 December 2003 Structure of AQP1 Hg++ inhibitory site Fluid Intake • Hypothalamus - thirst control center • Oral fluid intake - requires an alert state • Osmoreceptors - monitor osmolality Fluid Output • Loss through the kidneys and GI tract • Insensible • Sensible Cations • Sodium (Na+) – Most abundant in the extracellular fluid – Maintains water balance, transmits nerve impulses, contracts muscles – Values - 135-145 mEq/L Cations • Potassium (K+) – Major intracellular cation – Regulates neuromuscular excitability, muscular contraction, and acid-base – Value - 3.5 -5.3 mEq/L Cations • Calcium (Ca2+) – Cardiac conduction, blood coagulation, bone growth and formation, & muscular relaxation – Value - 4 - 5 mEq/L Cations • Magnesium (Mg2+) – Second most important of intracellular fluids – Enzyme activities, muscular excitability – Value - 1.5 - 2.5 mEq/L Water (and sodium) disorders Dehydration hypertonic isotonic water excess hypotonic Extracellular fluid deficit 1. Hypotonic dehydration sodium loss > water loss serum sodium < 130mmol/L plasma osmotic pressure < 280mOsm/L hypertonic isotonic hypotonic 1) Cause and Pathogenesis Excessive loss of water Sodium replaced with water only. Vomiting, diarrhea; burn; diuretics; Addison’s disease (ADS ) ; Chronic renal failure; renal tubular acidosis 2) Adaptive response and effect on body ① movement of body fluid ECF ICF Cellular swelling Blood volume Extracellular fluid Shock Dehydrated signs Brain and lung edema ② urinary alteration urine specific urine volume gravity [Na+] ---------------------------------------------------------Early ADH ±or stage ADS Late ADH stage ADS ----------------------------------------------------------- 3) principles of treatment ① treating primary disease ② 0.9%NaCl 2. Hypertonic dehydration ① water loss > sodium loss ② serum sodium > 150mmol/L ③ plasma osmotic pressure >310mOsm/L 1) Cause and pathogenesis lack of water (desert; sea) ① intake to drink inability (coma; baby) lung: hyperpnea (hypoxia; acidosis) ② loss skin: fever; hyperthyroidism; sweat; exposure to hot environment digestive tract: vomiting; diarrhea; baby diarrhea ([Na+]: 60mmol/L) kidney: diabetes (ketosis); diabetes insipidus diuretic (mannitol; hypertonic glucose) 2) Effect on body ① hypertonic of ECF thirst ② movement of the body fluid ICF ECF cell dehydration Brain dehydration Sleepiness Dehydrated fever subarachnoid bleeding ③urinary alteration urine specific urine volume gravity [Na+] ---------------------------------------------------------------Early ADH stage ADS± Late ADH stage ADS ----------------------------------------------------------------3) principles of treatment Water > NaCl 3. isotonic dehydration ① water loss ≈ sodium loss ② serum sodium = 130-150mmol/L ③ plasma osmotic pressure:280- 310mOsm/L 1) cause and pathogenesis ① vomiting; diarrhea; gastrointestinal suction; biliary fistula; intestinal fistula ② ascitic fluid; pleural effusion 2) effects on body ① slight thirst ② blood volume dehydrated signs; BP ③ urinary alteration urine specific urine volume gravity [Na+] -----------------------------------------------------------------Early ADH stage ADS Late ADH stage ADS -----------------------------------------------------------------3) principles of treatment 补偏低渗液;先补0.9%NaCl Extracellular fluid excess 1. Water intoxication water intake , total sodium ±; ECF , ICF ; hyponatremia; Serum sodium < 130mmol/L 1) Causes excessive water intake renal loss (acute renal failure; acute congestive heart failure) 2) effects on body brain cells swelling water moves into cells pulmonary edema 3) principles of treatment diuresis 2. Edema interstitial fluid fluid in the body cavities hydrops fluid in the cells cellular edema (1) pathogenesis 1) imbalance of exchange between intra- and extra-body fluid (retention of water and sodium) basic mechanism: glomerular-tubular imbalance ① GFR acute glomerulonephritis heart failure ② reabsorption of proximal tubule sympathetic nerve filtration fraction ANP reabsorption of water and sodium Electrolyte Imbalances Hyponatremia • Defined as serum [Na+] less than 136 mEq/L • Water shifts into cells causing cerebral edema • 125 mEq/L – nausea and malaise • 120 mEq/L – headache, lethargy, obtundation • 115 mEq/L – seizure and coma Hyponatremia (cont) • 1. Assess plasma osmolality • 2. Assess volume status of patient – Hypervolemic, Euvolemic, Hypovolemic • 3. Assess Urine Sodium Concentration – Needed for definitive diagnosis, not needed for treatment purposes • 4. Calculate Na+ Deficit – 0.6 x weight (kg) x (130 – plasma [Na+]) • 5. Correct at no more than 0.5mEq/L per hour or 12 mEq/L per 24 hours Isosmotic and Hyperosmotic Hyponatremia – Iso and Hyperosmotic hyponatremia are due to excessive solutes in plasma. – Isosmotic • Pseudohyponatremia – No treatment necessary – Hyperlipidemia – Hyperproteinemia • Isotonic Infusions – Glycine – Mannitol – Hyperosmotic – Treat underlying cause • Hyperglycemia – Each 100 mg/dl of glucose reduces [Na+] by 1.6 mEq/l • Hypertonic Infusions – Glycerol – Mannitol – Glycine Hyposmotic Hyponatremia • 1. Assess volume status – Hypervolemic – cirrhosis, heart failure, nephrotic syndrome – Euvolemic – polydipsia, SIADH – Hypovolemic – most common cause • Excessive renal (diuretic) or GI (emesis, diarrhea) losses Treatment of Hyponatremia • Iso or Hyperosmotic – Correct underlying disorder • Hyposmotic – Iso or hypervolemic – fluid restriction – Hypovolemic • Asymptomatic – fluid resuscitate with isotonic saline • Symptomatic or plasma [Na+] less than 110 mEq/L – Calculate Na+ deficit – Correct at a rate no greater than 0.5 mEq/L/hour or 12 mEq/L/day Correction of Sodium Deficit Example: A 60 kg woman with a plasma sodium concentration of 120mEq/L: Sodium deficit = TBW x (130 – [Na+]p) Sodium deficit = 0.5 x 60 x (130-120) = 300mEq 3% NaCl contains 513 mEq sodium/L Volume of 3% NaCl needed = 300/513 = 585 mL At 0.5 mEq/L/hr a correction of 10 mEq should be done over 20 hours So, 585 mL/20 hours = 29 mL/hour of 3% NaCl Hypernatremia • Defined as serum [Na+] greater than 146 mEq/L • Lethargy, weakness, and irritability that progress to seizure, coma, and death • Usually occurs in adults with altered mental status or no access to water Hypernatremia (cont) • 1. Assess volume status • 2. Measure urine [Na+] • 3. Calculate water deficit – 0.6 x weight (kg) x ([Na+]/140 -1) • 4. Correct with free water no faster than 0.5 mEq/L/hour or 12 mEq/L/day Hypernatremia • Hypovolemic – loss of hypotonic fluids – Diuresis, vomiting, diarrhea • Isovolemic – loss of free water – Diabetes insipidus, hypodipsia • Hypervolemic – gain of hypertonic fluids – Hypertonic saline administration Treatment of Hypernatremia • Hypovolemic – Replace the free water deficit • Hypervolemic – Diuretics (lasix) to excrete sodium in urine combined with hypotonic saline for partial volume replacement Treatment of Hypernatremia • Isovolemic – Diabetes Insipidus – Loss of hypotonic urine secondary to lack of ADH production (central) or lack of response to ADH by kidney (nephrogenic) – Hallmark is hypotonic urine (200-500 mOsm/L) with hypertonic plasma – Treat by correcting free water deficit – In central DI must also administer 5 – 10 units of DDAVP Q6H to prevent ongoing free water loss Hyperkalemia • Defined as a serum [K+] greater than 4.6 mEq/L • Changes in cellular transmembrane potentials can lead to lethal cardiac arrhythmias • Most often associated with renal impairment coupled with exogenous K+ administration or drugs that increase K+ • Transcellular shifts – acidosis, succinylcholine, insulin deficiency, massive tissue destruction • Massive blood transfusions • Pseudohyperkalemia - Thrombocytosis, hemolysis, leukocytosis • Urine K+ excretion rate can be used to determine exact cause of hyperkalemia Hyperkalemia • Drugs causing hyperkalemia – K+ sparing diruetics, ACEI, NSAIDs, Heparin, Cyclosporin, Tacrolimus, Bactrim • EKG Changes – 5.5 – 6.5 mEq/L – peaked T-waves – 6.5 – 7.5 mEq/L – loss of P-waves – > 8.0 mEq/L – widened QRS Treatment of Hyperkalemia • 1. If EKG changes administer 10 mL of 10% Calcium Gluconate • 2. 1 amp D50 with 10 units IV insulin (onset 10-20 minutes, duration 2-3 hours) • 3. Albuterol 10 -20 mg (onset 4-5 hours, duration 2-3 hours) • 4. Kayexalate 15-30 g (oral onset 4-5 hours, enema onset 1 hour) • Dialysis Hypokalemia • Defined as serum [K+] less than 3.6 mEq/L • Occurs in up to 20% of hospitalized patients • 2.5 mEq/L – muscular weakness, myalgia • <2.5 mEq/L – cramps, parasthesias, ileus, tetany, rhabdomyolisis, PVCs, A-V block, V-tach, V-fib Hypokalemia • Inadequate intake • Increased excretion – diarrhea, diuretics, alkalosis, glucocorticoids, RTA • Transcellular shifts – beta-agonists, theophylline, insulin, hyperthyroidism, barium • Replace no faster than 20 mEq/H peripherally and 100 mEq/H centrally Hypercalcemia • Excess calcium • Needs vit D for efficient absorption; most of Ca is stored in the bones. • Causes: bone tumors that cause bone destruction, chemo rx release Ca from the bones; immobilization causes loss from the bones (usually excreted) but if kidneys can’t clear it, hypercalcemia results, increased intake (milkalkali syndrome). Hypercalcemia (cont) • Clinical manif: Ca imbalances alter neuromuscular irritability with non-specific symptoms – Constipation, anorexia, N/V, fatigue, skeletal muscle weakness, confusion, lethargy. – Renal calculi, cardiac arrhythmias – HyperCa increases Na and K excretion leading to polyuria and polydipsia. – Rx: serum Ca, Ionized Ca, fluids, Lasix, steroids, dialysis. Hypocalcemia • Decreased serum calcium • Causes: decreased intake of Ca and/or Vit D (adolescents are vulnerable d/t fad diets and the deficit cannot be made up later, increasing risk for osteoporosis). – Limited exposure to sunlight, premature infants and dark skinned people at increased risk to inadeq. Vit D and therefore decreased Ca absorption. – Parathyroid dysfunction, multiple transfusion (Citrate binds Calcium), steatorrhea (as in pancreatitis and Cystic Fibrosis) binds Calcium in the stool. Hypocalcemia (cont) • Clinical Manif: acute situation related to increased muscular excitability: tetany. +Chvostek’s Sx, + Trousseau’s Sx. • In children: Twitching, cramping, tingling around the mouth or fingers, carpal/pedal spasms. • In infants: tremors, muscle twitches, brief tonicclonic seizures, CHF. • Laryngospasm, seizures and cardiac arrhythmias in severe situations. Hypocalcemia (cont 2) • In children and adolescents, chronic hypocalcemia more common, manif. By spontaneous fractures. Lab tests: serum Ca; bone density study Rx: oral and/or IV Ca, Ca rich diet Hypermagnesemia • Excess in Mg. • Imbalances characterized by neuromuscular irritability • Causes: impaired renal function, Mag Sulfate given perinatally to treat eclampsia, increased use of laxatives, enemas, antacids, IV fluid additives. Hypermagnesemia (cont) • Clinical Manif: decreased muscle irritability, hypotension, bradycardia, drowsiness, lethargy, weak or absent DTR’s. • Rx: increase fluids, diuretics, dialysis. Hypomagnesemia • Decreased serum Mg. • Stored in cells and bones • Causes: prolonged NPO without replacement, chronic malnutrition, chronic diarrhea, short bowel syndrome, malabsorption syndromes, steatorrhea, multiple transfusions, prolonged NG Sx, some medications. Hypomagnesemia (cont) • Clinical manif: increased neuromuscular excitability (tetany). Hyperactive reflexes, skeletal muscle cramps, twitching, tremors, cardiac arrhythmias, seizures. • Lab: serum Mg along with Ca and K. • Rx: po/IV Magnesium admin and treating underlying cause of imbalance.