Amino acid metabolism 1
advertisement
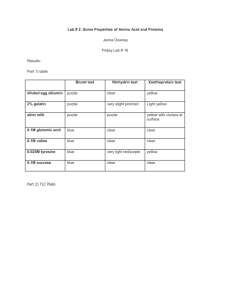
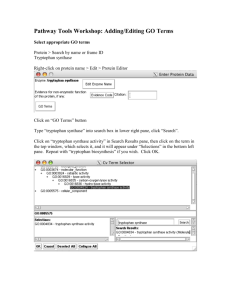
Dr.S.Chakravarty,MD • Explain the steps in synthesis of various non-essential amino acids in the body • List the molecules derived from aromatic amino acids and their uses • Discuss the enzyme deficiencies of aromatic amino acid metabolism and their clinical features • Differentiate various types of phenylketonuria and its diagnosis • Discuss the clinical features of Alkaptonuria and its treatment 1. Glutamate : NH3 Alpha keto Glutarate Glutamate dehydrogenase Glutamate Glutamate Dehydrogenase 2. Glutamine: NH3 Glutamate Glutamine Glutamine synthase Glutamine syhthetase Transamination reactions 3. Alanine: Pyruvate Glutamate ALT PLP Alanine Alpha keto glutarate 4. Aspartate : AST Oxaloacetate Glutamate PLP Aspartate Alpha keto glutarate 5. Asparagine: NH3 Aspartate Asparagine Asparagine synthase 6. Tyrosine : Phenylalanine THB DHB Tyrosine Phenyl alanine Hydroxylase 7. Glycine - Glycine amidotransferases synthesize glycine from glyoxylate and glutamate or alanine. Two other reactions make glycine :- serine hydroxymethytransferase reaction(freely reversible) • 8. Serine :- Two ways to make it – Reversal of serine hydroxymethytransferase reaction 9. Proline – from Glutamate -reversal reaction of proline catabolism Methionine Methionine adenosyl transferase THF ATP 10. Cysteine: S- Adenosyl Methionine Acceptor Methyl transferase CH3-acceptor S- Adenosyl Homocystiene Homocysteine methyl Transferase (CH3 1-carbon )B12 Homocysteine Serine B6 Cystathionine β synthase Methyl THF Cystathionine Cystathioninase B6 Cysteine Alpha-keto butyrate • Phenylalanine – essential • Tyrosine – non essential • Tryptophan – essential SYNTHESIS OF THYROID HORMONES MELANIN SYNTHESIS TYROSINE CATABOLISM TO ACETOACETIC ACID (KETOGENIC ) + FUMARIC ACID SYNTHESIS OF CATECHOLAMINES eg Epinephrine and Norepinephrine Dihydrobiopterin reductase Phenylalanine Phenylalanine hydroxylase Tyrosine THB Tyrosine Hydroxylase DHB DOPA co2 B6 DOPA Decarboxylase Arvid Carlsson M.D. Nobel Prize Dopamine 2000 β oxidase alongwith Eric Kandel and Paul Greengard. Dopamine Dihydrobiopterin reductase Important – alpha methyl DOPA inhibits dopa decarboxylase and prevents hypertension by decreasing epinephrine Ascorbate(Vitamin C) O2, Cu2+ Dehydro-Ascorbate Nor-Epinephrine S- Adenosyl Methionine (SAM) Phenylethanolamine N-methyl Transferase (NMT) Catechol-o-methyl Transferase (COMT) Epinephrine S- Adenosyl Homocysteine (SAH) mono amine oxidase(MAO) metanephrine Vanillyl mandelic acid • Schizophrenia – Dopamine overproduction • Parkinson’s disease : Damage to Nigro-striatal tract - Dopamine Treatment: – Levo-DOPA + Carbidopa Carbidopa is PERIPHERAL DOPA-DECARBOXYLASE INHIBITOR it increases the plasma half-life of levodopa from 50 minutes to 1½ hours. Carbidopa cannot cross the blood brain barrier, so it inhibits only peripheral DDC. It thus prevents the conversion of L-DOPA to dopamine peripherally • Pheochromocytoma • Neuroblastoma Increased catecholamine production IMPORTANCE OF VMA estimation • Some tumors like Pheochromocytoma (epinephrine excess ) or Neuroblastoma • Excess of VMA in urine Lab analysis Tyrosine Tyrosinase Copper (Melanoblasts ) DOPA Copper Tyrosinase (Melanoblasts ) Dopaquinone Several steps TYROSINASE IS ABSENT IN ALBINISM NO MELANIN Melanin THIS ALSO EXPLAINS HYPOPIGMENTATION IN PHENYLKETONURIA !! • T3 Triiodothyronine • T4 Thyroxine Catabolism of phenylalanine and tyrosine USMLE !! Phenylalanine Phenylketonuria Phenyl alanine Hydroxylase Tyrosine Tyrosinemia- II Tyrosine Aminotransferase Parahydroxyphenyl pyruvate Cu, Vit C P-Hydroxyphenyl pyruvate hydroxylase Homogentisic acid Alkaptonuria Tyrosinemia- I Fumarate Homgentisate oxidase Fumaryl acetoacetate hydrolase Acetoacetate 1 Type II TYROSINEMIA 2 NEONATAL TYROSINEMIA 3 ALKAPTONURIA 4 TYPE I TYROSINEMIA Tyrosinemia Type 1 • Defect in fumarylacetoacetate hydrolase • Plasma tyrosine levels elevated (6-12mg/dl)] – ACUTE FORM – FATAL BY 6-8 MONTHS – CHRONIC FORM- 10 YEARS • • • • DIARRHOEA VOMITING CABBAGE LIKE ODOR LIVER FAILURE • URINE :-tyrosine, p -hydroxyphenyl pyruvate, P- hydroxyphenyl lactate , p- hydroxyphenyl acetate Tyrosinemia Type II (Richner Hanhart Syndrome) DEF. OF TYROSINE AMINOTRANSFERASE • Mental retardation • Keratosis of palmar surface • Painful corneal lesions • Photophobia NEONATAL TYROSINEMIA • Def . Of p-hydroxyphenyl pyruvate hydroxylase Phenylketonuria Phenylalanine Phenylalanine hydroxylase defect (-) Dihydrobiopterin reductase defect Phenylpyruvate Phenyl Lactate Tyrosine Phenyl acetate Phenyl acetyl Glutamine ALTERNATE ROUTES OF METABOLISM OF PHENYLALANINE Phenylketonuria USMLE !! • Autosomal recessive disease – MC disorder of amino acid metabolism • Def of phenylalanine hydroxylase or Dihydrobiopterin reductase. • Increased phenylalanine in the blood • Saturates – LNAAT (large neutral aminoacid transporter system of brain). • mental retardation, seizures– Poor protein and neurotransmitter synthesis in brain – Toxicity from accumulating alternate metabolites like phenylketones • Decreased pigmentation of skin and eyes. Amino Acid Disorders Argininosuccinic aciduria (ASA) NEONATAL SCREENING IN FLORIDA Citrullinemia, type I (CIT) (SOURCE CDC website and http://www.babysfirsttest.org) Classic phenylketonuria (PKU) Homocystinuria (HCY) Hemoglobin Disorders • Mousy/ of urine – phenyl acetate, phenyl lactate and phenylpyruvate Maple syrup urineMusty diseaseodor (MSUD) S, Beta-thalassemia (Hb S/ßTh) Tyrosinemia, type I (TYR I) S, C disease (Hb S/C) in urine. Tyrosinemia, type II (TYR II) Sickle cell anemia (Hb SS) • National biochemical screening programme Endocrine Disorders Organic Acid Conditions Congenital adrenal hyperplasia 3-Hydroxy-3-methylglutaric aciduria (HMG)or • Blood sample – Heel(CAH) filter paper analytical laboratory ( PCR + HPLC Primary congenital hypothyroidism (CH) 3-Methylcrotonyl-CoA carboxylase deficiency (3-MCC) TANDEM MASS SPECTROMETRY) Beta-ketothiolase deficiency (BKT) – Screens diseases like :Glutaric acidemia type I (GA1) Fatty Acid Oxidation Disorders Holocarboxylase synthetase deficiency (MCD) • Cystic fibrosis Carnitine acylcarnitine translocase deficiency (CACT) Isovaleric acidemia (IVA) • PKU Carnitine palmitoyltransferase I deficiency (CPT-IA) Methylmalonic acidemia (cobalamin disorders) (Cbl A,B) Carnitine palmitoyltransferase type II deficiency (CPT-II) Methylmalonic acidemia (methymalonyl-CoA mutase • Congenital hypothyroidism Carnitine uptake defect (CUD) deficiency) (MUT) Glutaric acidemia, type II (GA-2) Propionic acidemia (PROP) • Medium chain acyl CoA dehydrogenase deficiency Long-chain L-3 hydroxyacyl-CoA dehydrogenase Other Disorders • FeCl test – Ferric chloride test. 3 deficiency (LCHAD) Biotinidase deficiency (BIOT) Medium-chain acyl-CoA dehydrogenase deficiency Classic galactosemia (GALT) (MCAD) Cystic fibrosis (CF) • Guthrie test: Gold standard of the past Short-chain acyl-CoA dehydrogenase deficiency (SCAD) Hearing loss (HEAR) Trifunctional protein strains deficiency Severe combined growth immunodeficiency (SCID) growth – Certain of (TFP) Bacillus Subtilis need Phe as essential factor.Bacterial Very long-chain acyl-CoA dehydrogenase deficiency cannot occur in medium devoid of Phe. (VLCAD) Cont.. – So, bactera will grow if blood containing Phe is added = PHENYLKETONURIA Treatment • Early detection is VERY IMPORTANT !! • Diet containing low phenylalanine – ( but NEVER ZERO Phe!!) – FOOD BASED ON TAPIOCA (CASSAVA ) IS HELPFUL • SPECIAL DIET TILL 5YEARS OF AGE • SPECIAL DIET AGAIN IF PERSON IS PREGNANT LATER ON Excess Phe affects brain development of fetus . Phenylketonuria Phenylalanine Hydroxylase def Dihydrobiopterin reductase def • Normal levels of dopamine • Low levels of dopamine • Normal levels of prolactin • High levels of prolactin • Normal levels of catecholamines • Low levels of cathecolamines • Normal levels of tryptophan and serotonin • Increased tryptophan and decreased serotonin Alkaptonuria • Autosomal Recessive • Deficient enzyme: Homogentisate 1,2-dioxygenase/ (Oxidase) – conversion of homogentisic acid (product of tyrosine metabolism) to maleylacetoacetate (→ acetoacetate → Fumarate → TCA) • Pathology – Homogentisic acid accumulates, auto-oxidizes – Oxidized homogentisate polymerizes, forms dark-colored pigment – Purplish black color of urine on standing • Precipitates of dark homogentisic acid (Alkaptan bodies) deposit in connective tissue discoloration (ochronosis) – – – – e.g. in cartilage, joints, ear wax vertebrae deposits cause Arthralgia (joint pain) sometimes associated with degenerative arthritis I N D I C A N Niacin Catabolized to Acetoacetyl CoA (KETOGENIC ) + alanine (Glucogenic ) Synthesis of Serotonin and Melatonin Tryptophan THB Tryptophan Hydroxylase DHB 5-HydroxyTryptophan NADP NADPH + H + PLP A.A. decarboxylase Monoaminooxidase-A (MAO) 5-HydroxyTryptamine (Serotonin) Acetyl CoA Acetylation Acetylation N-acetyl Serotonin methylation Melatonin SAM SAH 5 HYDROXY INDOLE ACETIC ACID ( HIAA) Serotonin MAO-A inhibitors (Anti-Depressants) (-) Monoaminooxidase-A (MAO) 5- Hydroxy indole acetic acid (HIAA) MAO- mono amino oxidase • Epinephrine, norepinephrine, serotonin and melatonin are metabolised by MAO- A enzymes • Dopamine, Tyramine and tryptamine are metabolised by both MAO-A and MAO-B • Tyramine mimics catecholamines in their actions Cheese reaction • A patient presents with headaches, palpitations, nausea and vomiting and elevated blood pressure. These symptoms appear after the person has eaten a large meal containing aged cheeses and wine. The patient’s history indicates that he is on some medicaton for a different condition. Assuming that the medication is in some way involved in these symptoms, which enzyme might be the target of this drug? A. B. C. D. E. Glutamate decarboxylase Monoamine oxidase Tyrosine hydroxylase DOPA decarboxylase COMT (catechol O-methyl transferase) Tryptophan Tryptophan pyrrolase N-formyl kynurenine THFA Kynurenine formylase Formyl THFA 1 CARBON POOL 3-hydroxykynurenine Kynureninase H2O PLP Alanine 3-hydroxy Anthranilic acid(HIAA ) NAD, NADP (Niacin) 60mg tryptophan = 1 mg NIACIN Xanthurenic acid TCA cycle Acetyl Co-A Acetoacetyl Co-A A. 1. 2. 3. 4. 5. Carcinoid syndrome :- (Argentaffinomas ) Neuroendocrine tumors – Midgut, bronchus Excessive serotonin and kallikrenin. Diarrhoea , flushing, abdominal cramps, Heart failure – damage to valves Diagnosis : HIAA in urine • Pellagra like synptoms : Def of B6 or Tryptophan Diarrhoea, Dementia and Dermatitis • Remember – Hartnups disease • Melatonin: promotes sleep – sleep wake cycle 1. Hormone of the dark – blue light inhibits melatonin synthesis. 2. Lowers Leptin levels • Tryptophan load test – B6 deficiency Depression • Decrease in serotonin levels in CNS • Treatment : 1. MAO-A inhibitors 2. SSRIs – selective serotonin reuptake inhibitors Mcq • The non essential amino acid that becomes essential in PKU is :• A. Phenylanaline • B.Tyrosine • C.Tryptophan • D. ALANINE • E. Cysteine Mcq • • • • • • The cause of light skin color in PKU is A. decreased synthesis of melanin from Phe B. decreased synthesis of melanin from Tyr C. excess melanin synthesis from Phe D. excess of phenylketones E.mental retardation causes decreased melatonin