UNCONSCIOUS PATIENT
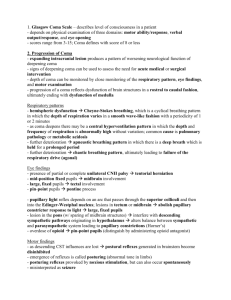
advertisement

UNCONSCIOUS PATIENT Dr. M. Sofi MD; FRCP (London); FRCPEdin; FRCSEdin NEUROLOGICAL ASSESSMENT Consciousness is a state of awareness of self and the environment. This state is determined by two separate functions: a) Awareness (content of consciousness). b) Arousal (level of consciousness) Coma is caused by disordered arousal rather than impairment of the content of consciousness. a) Arousal depends on an intact: ascending reticular activating system b) connections with diencephalic structures Coma is caused by: Diffuse bilateral hemisphere damage. Failure of the ascending reticular activating system, or both. Sites and causes of coma. ARAS Diffuse mass of neurons & nerve fibers that make the core of the brain stem. Fibers run through medulla oblongata, pons & midbrain. Receives fibers from the sensory pathways via long ascending spinal tracts. Ascending ReticularActivating System ASCENDING RETICULAR ACTIVATION SYSTEM - ARAS • It’s believed to be the center of arousal and motivation in mammals. • Alertness, maintenance of attention and wakefulness. • Emotional reactions, important in learning processes. • Identify causes(s) of a deteriorating conscious level. • Stabilize, evaluate, and treat the comatose patient in the emergency setting. • Use an organized, sequential, prioritized approach. • Use the Glasgow coma scale for assessment of altered conscious level. Altered levels of consciousness • Clouding of consciousness is a very mild form of altered mental status in which the patient has inattention and reduced wakefulness. • Confusional state is a more profound deficit that includes disorientation, bewilderment, and difficulty following commands. • Lethargy consists of severe drowsiness in which the patient can be aroused by moderate stimuli and then drift back to sleep. • Obtundation is a state similar to lethargy in which the patient has a lessened interest in the environment, slowed responses to stimulation, and tends to sleep more than normal with drowsiness in between sleep states. • Stupor means that only vigorous and repeated stimuli will arouse the individual, and when left undisturbed, the patient will immediately lapse back to the unresponsive state. • Coma is a state of unarousable unresponsiveness. Grady Coma Scale Grade State of awareness Responds appropriately to: Calling Light Deep name pain pain I Confused, drowsy, lethargic, indifferent and/or uncooperative; does not lapse into sleep when left undisturbed Yes Yes Yes II Stuporous; may be disoriented to time, place, and person; will lapse into sleep when not disturbed; or belligerent and uncooperative No Yes Yes III Deep stupor; requires strong pain to evoke movement No No Yes IV Exhibits decorticate or decerebrate posturing to a deep pain stimulus No No No V Does not respond to any stimuli; flaccid No No No Coma: Causes I. Head Trauma Coma may result from significant traumatic injury to the head, such as from a car accident or fall. II. Bleeding (Hemorrhage) into the brain or skull Types of brain/skull hemorrhage include: a. Intracerebral hemorrhage: bleeding within the brain tissue b. Epidural hemorrhage: bleeding inside the skull, but outside the dura, (the covering of the brain) c. Subdural hemorrhage: bleeding inside the skull, and inside the dura, but not in the brain tissue itself d. Subarachnoid hemorrhage: bleeding in the space immediately adjacent to the brain tissue Coma: Causes III. Causes of brain/skull hemorrhage include: a. High blood pressure (hypertension) b. Cerebral aneurysm: a weak spot in a blood vessel of the brain c. Arteriovenous malformation (AVM): an abnormal cluster of blood vessels d. Tumors IV. Swelling of the brain (cerebral edema) Causes of swelling of the brain: a. Infections b. Metabolic imbalances c. Traumatic injuries d. Problems with the flow of cerebrospinal fluid (CSF) Coma: Causes V. Lack of oxygen to the brain The most common causes for lack of oxygen to the brain include: a. Heart arrhythmias b. Lung disease, including pneumonia, emphysema, or asthma. c. Anemia (low red blood cell count) d. Toxins VI. Poisons External poisons are those that are ingested or inhaled. Internal poisons are by-products of the body's normal metabolism that for some reason cannot be excreted properly. VII. Endocrine disorders a. Myxedema coma (hypothyroidism) b. Diabetes Mellitus: Hypoglycemia or Hyperglycemia CLINICAL ASSESSMENT OF COMA Coma is an acute, life threatening situation and evaluation must be swift, comprehensive and include: Resuscitation of CVS and respiratory system. Correction of blood glucose and thiamine Control of seizures Temperature Specific treatments— naloxone. If Indicated Assessment now should comprise: 1. History—through friend, family or emergency medical personnel 2. General physical examination 3. Neurological assessment—to define the nature of coma CLINICAL ASSESSMENT OF COMA The approach to clinical evaluation is used to categories coma into: A. Coma without focal signs or meningism. This is the most common form of coma and results from anoxicischaemic, metabolic, toxic, and drug induced insults, infections, and post-ictal states. B. Coma without focal signs with meningism. This results from subarachnoid hemorrhage, meningitis, and meningoencephalitis. C. Coma with focal signs. This results from intracranial haemorrhage, infarction, tumor or abscess. THE ABCD2E APPROCH TO COMA A AIRWAYS B BREATHING C CIRCULATION D DRUGS/DISABILITY E EXPOSURE CLINICAL ASSESSMENT OF COMA General examination Neurological (general) Skin: rash, anemia, jaundice Head, neck and eardrum (trauma) Temperature: (fever infection hypothermia-drugs/circulatory failure Meningism (SAH/meningitis) Blood pressure (for example, septicemia/Addison's disease) Fundoscopy Breath (fetor hepaticus/alcohol) Motor response Cardiovascular (for example, arrhythmia) Deep tendon reflexes: Biceps, Triceps, Brachioradialis, Patellar, Achilis Abdomen (organomegaly) Muscle tone/Planters CLINICAL ASSESSMENT OF COMA Pupillary Patterns in Comatose Patients Pattern Small, reactive Site of dysfunction Diencephalon Large "fixed," with hippus Midbrain tectum Midposition, "fixed" Midbrain Pinpoint, not reactive Pons One dilated Suggests transtentorial herniation Pupils: Localizing Value Pupils: Localizing Value Horner’s syndrome Midriasis-sympathetic stimulation Eye Movements Left 6th Nerve Palsy Left 3rd Nerve Palsy CLINICAL ASSESSMENT OF COMA Brainstem Reflexes Reflex Pupillary light reaction Technique Shine light on pupil and observe constriction Localization Midbrain and pontine tegmentum Corneal response Open lid if necessary; lightly stroke cornea with cotton wisp; observe for blink Pons Oculocephalic response (doll's eyes) Hold lids open with one hand while turning head side to side with the other hand; observe rotation of eyes side to side Pons—vestibular Oculovestibular; cold-water calorics With head at 30 degrees, irrigate external auditory canal and tympanic membrane slowly with up to 120 ml ice water; observe for conjugate rotation of the eyes toward the side irrigated Pons—vestibular Puppilary light reflex • Pupillary light reflex (PLR) is a reflex that controls the diameter of the pupil, in response to the intensity (luminance) of light. • Controls adaptation to various levels of lightness/darkness. • A greater intensity of light causes the pupil to constrict (miosis). • lower intensity of light causes the pupil to dilate (mydriasis, expansion) (allowing more light in). Corneal Reflex Afferent: Trigeminal Nerve Efferent: Third Nerve (Bell’s Phenomenon and Facial Nerve (Eye closure) Tests dorsal midbrain (Bell’s) and pontine integrity (Eye closure) • Definition: The gag reflex evaluates the integrity of Cranial nerves IX and X • Test procedure: Using a long handle swab stick (orange swab) gently and briskly touch the pharyngeal wall behind the pillars of the fauces. • Test findings: – A positive gag reflex will produce a non symmetrical elevation of the uvula or the fauces. – If there is no movement of the uvula with the gag reflex and with saying 'ahh' this may signify bilateral palatal muscle paralysis. – In a normal gag reflex there will be a symmetrical elevation of the uvula or the fauces / tonsilar arches. Gag reflex Test for oculocephalic reflex response (Doll’s eyes phenomena). (B) abnormal response when thee head is rotated the eyes do not turn in a conjugated manner. Vestibulo-cephalic reflex test Caloric reflex test is a test of the vestibulo-ocular reflex that involves irrigating cold or warm water or air into the external auditory canal. The eyes should move conjugately in the direction opposite to the cold irrigation and same side to warm irrigation. An abnormal response (absent or asymmetric) implies brain stem disease. One mnemonic used to remember the FAST direction of nystagmus is COWS. COWS: Cold Opposite, Warm Same. Some Abnormal Respiratory Patterns Found in Comatose Patients Pattern Description Site of dysfunction Cheyne–Stokes Periodic breathing in which phases Cerebral of hyperpnea alternate with hemispheres; apnea; the phases alternate every diencephalons 30 to 45 seconds Central neurogenic hyperventilation Deep, rapid respirations at a rate of 24 or more/min Apneustic A prolonged inspiratory "cramp"; a Pontine prolonged gasp tegmentum Ataxic Random sequences of shallow and Medulla deep respiration without pattern Midbrain; diencephalons Ataxic (Biot) breathing is a random pattern of shallow and deep breaths interspersed with irregular pauses – pontine lesions Apneustic breathing involves repetitive gasps, with pauses at full inspiration lasting a few seconds - pontine disease. Cheyne-Stokes respiration is cyclic, with a crescendo-decrescendo pattern interrupted by apneas – brainstem lesions. Abnormal breathing patterns Assesses patient’s neurological condition Value range 3 -15 3 totally comatose patient 9-12 Moderate altered conscious level 15 fully alert patient Coma Mimics • • • • Akinetic mutism ‘Locked-in’ syndrome Catatonia Conversion reactions Akinetic Mutism • Silent, immobile but alert appearing • Usually due to lesion in bilateral mesial frontal lobes, bilateral thalamic lesions or lesions in periaqueductal grey (brainstem) Many cases of akinetic mutism have occurred after a thalamic stroke “Locked-In’ Syndrome • Infarction of basis pontis (all descending motor fibers to body and face) • May spare eyemovements • Often spares eyeopening • EEG is normal or shows alpha activity Bilateral Pontine Infarction Catatonia Symptom complex associated with severe psychiatric disease with: • stupor, excitement, mutism, posturing • can also be seen in organic brain disease: encephalitis, toxic and druginduced psychosis Conversion reactions • Fairly rare • Occulocephalics may or may not be present • The presence of nystagmus with cold water calorics indicates the patient is physiologically awake • EEG used to confirm normal activity