The Near-Term - March of Dimes
advertisement

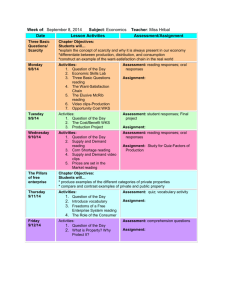
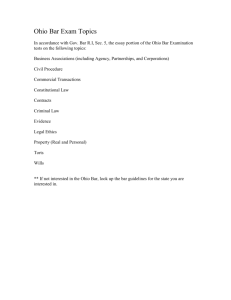
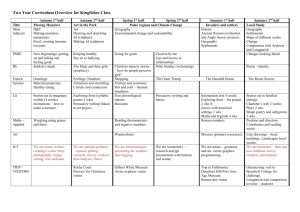
The Near-Term (Scheduled, Elective, Convenient) (Indicated?) Birth Controversy and the OPQC Christopher T. Lang MD Columbus, Ohio Disclosures: None Objectives… Audience members will be able to: List reasons for current concerns. Counsel women and families about the risks and benefits of near-term birth. Adopt care practices to reduce inappropriate scheduled births. Percent change in gestational age distribution in US (1990-2006) Martin JA, Hamilton BE, Sutton PD, et al. Natl Vital Stat Rep. 2009. Causes and consequences of the rise in late preterm birth A culture of “interventional obstetrics” Medical and obstetric benefit Rising rates of scheduled births after 37 wks Rising rates of cesarean births Obstetric complacency Obstetricians work in Labor & Delivery Unit Pediatricians work in the NICU Happy parents until they are unhappy in NICU Unhappy AAP, March of Dimes, others Unhappy obstetricians (?) Unhappy patients and colleagues Late-preterm and near-term infants occupy most NICU beds Number of Patients 30000 25000 20000 15000 10000 5000 0 23 24 25 26 27 28 29 30 31 32 33 34 35 36 37 38 39 40 Estimated Gestational Age (wks) Clark R et al. Pediatrix Database. 2005. Increased public awareness of the risks of near-term birth Morbidity at 37 and 38 wks greater than at 39 wks March of Dimes National conferences – Surgeon General, IOM, NIH Recent literature State preterm birth “report cards” – Ohio got an F The “Brain Card” The “Fertility Care Card” Health departments and hospital systems Hospital Performance Public Reporting Perinatal Measures (March, 2009 Ohio HB 197) Measure Title Source Cesarean rate for low-risk first birth women (NTSV CS rate) California Maternal Quality Care Collaborative Elective delivery prior to 39 completed wks gestation HCA - St Mark’s Perinatal Center Appropriate use of antenatal steroids Providence St. Vincent’s Hospital/Council of Women and Infants' Specialty Hospitals (CWISH) Infants < 1500g not delivered at appropriate level of care California Maternal Quality Care Collaborative (CMQCC) Timing of elective repeat cesarean delivery at term and neonatal outcomes Tita ATN, Landon MB, Spong CY, et al. NEJM. 2009. Timing of elective delivery at term and neonatal outcomes Clark SL, Miller DD, Belfort M, et al. AJOG. 2009. Timing of delivery and diagnosis of clinically significant respiratory morbidity Yoder BA, Gordon MC, and Barth W. Obstet Gynecol. 2008. Infant mortality rates in Ohio by gestational age at birth 1999-2001 (423,803 births) 411,089 births, 35 – 41 weeks gestational age Infant Mortality Rate Ohio, 1999-2001 423,803 births, 35-41 weeks gestational age Infant Deaths per 1000 live births 12.0 10.0 8.0 6.0 4.0 2.0 0.0 35 36 37 38 39 Gestational Age (weeks) 40 41 Obstetrical factors contributing to a culture of scheduled birth More indicated inductions Time management Better induction techniques Need to satisfy patients Confidence in NICU care Better dates Antenatal tests not perfect Liability No suit for doing a cesarean Competition for OR slots Cesarean on demand Availability of anesthesia The tough case ACOG Guidelines: Indications for induction of labor (ACOG Practice Bulletin No. 10, 1999) Examples = Abruption, preeclampsia, etc… “Labor may also be induced for logistic reasons, for example, risk of rapid labor, distance from hospital, or psychosocial indications. In such circumstances, at least 1 of the criteria [for being at least 39 weeks gestation] should be met or fetal lung maturity should be established.” ACOG Guidelines: Confirming 39 wks gestation (ACOG Practice Bulletin No. 10, 1999) Fetal cardiac activity documented x 20 wks without electronic fetoscope or x 30 wks with Doppler 36 wks since positive beta-hCG by reliable lab Ultrasound at 6 - 12 wks 39 wks or greater Ultrasound at less than 20 wks confirms history and exam IOM Preterm Birth Report early scan for all patients The Washington Post May 21, 2006 (1) As Babies are Born Earlier, They Risk Problems Later The average U.S. pregnancy has shortened from 40 weeks to 39, driven by social and medical trends, e.g. older mothers, fertility treatments and more women’s decision to choose when they will deliver. At the same time, medical advances enable doctors to detect problem pregnancies earlier and to improve care for premature babies, prompting them to deliver babies early when something threatens their lives or those of their mothers. The Washington Post May 21, 2006 (2) As Babies are Born Earlier, They Risk Problems Later Some question whether the increase in Caesareans and inductions is the reason for the drop in stillbirths. They worry that much of the increase may be due to women hastening delivery for non-medical reasons — they want to make sure their mother will be in town, their husband has a business trip pending, or they are just fed up with being pregnant. An obstetrician in San Ramon, Calif. routinely honors such requests for the wives of professional athletes so their husbands can be present. “I have no problem with that. We never compromise the mother or baby’s safety.” The pediatric perspective (summary of the NICHD Late Preterm Workshop): Do some health care providers use “soft” indications for induction of labor in late-preterm pregnancies? Have the improved standards of neonatal care led to a sense of complacency concerning late-preterm births? Do some patients request early labor inductions (and their obstetricians oblige) for the sake of mutual conveniences? If so, how common are such practices? Are there variations in standards of care for latepreterm birth? Pediatricians do not speak the same language as obstetricians Late-preterm birth = not term = not 39 wks 386 wks = late-preterm Scheduled = elective = convenient A scheduled birth between 340 and 386 = elective Obstetrics Elective = not emergent Denominator: all fetuses Measure: gestational age “Good dates”: hx = US < 20 wks Pediatrics Elective = convenient Denominator: live born Measure: birth weight “Good dates”: Ballard score Perinatal mortality US (1990-2004) Mathews TJ, MacDorman MF. Natl Vital Stat Rep. 2008. Non-stress test ≠ Crystal ball Placenta previa Prior classical cesarean delivery Cholestasis of pregnancy Mild preeclampsia Preterm premature rupture of membranes “Institutional commitment” and the feasibility of decreasing elective deliveries (1) Oshiro BT, Henry E, Wilson J, et al. Obstet Gynecol. 2009. “Institutional commitment” and the feasibility of decreasing elective deliveries (2) Oshiro BT, Henry E, Wilson J, et al. Obstet Gynecol. 2009. A collaborative effort by Ohio care providers, hospitals, payers, parents and policy makers to identify and apply effective improvement methods to reduce preterm birth and morbidity and mortality for preterm infants in Ohio. 1 Preterm birth is the leading cause of infant mortality in Ohio. Among states, we rank 35th in infant mortality and 31st in prematurity. Effective interventions such as antenatal corticosteroids, surfactant, regionalized care, and CPAP are variably used throughout Ohio. Thus, there are opportunities to improve our care before and after birth. 2 OPQC has received a contract from the Ohio Department of Job and Family Services (ODJFS) for 2 years of funding from the Centers for Medicare & Medicaid Services (CMS) to further develop a quality improvement collaborative including setting up a data system and supporting optimal systems of care throughout Ohio. The Ohio Department of Health (ODH) is also a partner. March of Dimes, National Initiative for Children’s Healthcare Quality (NICHQ), AAP, ACOG 3 Ohio’s opportunity to be a national model… 1) Large and diverse population 2) Cooperative and collegial institutions and professionals 3) Regionalized care 4 5 Document method of pregnancy dating Document reason for scheduled delivery < 39 wks Document discussion with patient regarding risks and benefits of delivery < 39 wks Scheduled delivery form Communicate with pediatricians directly Promote early ultrasound Data tracking Gestational age distribution of births at OPQC member hospitals, by month, January 2006 to July 2009 65 60 55 2% decrease in births 36-38 wks and 2% increase in births 39-41 wks; approximately 1000 births moved to term Percent 50 45 40 35 30 25 20 Jan- Feb- Mar- Apr- May- Jun07 07 07 07 07 07 Jul- Aug- Sep- Oct- Nov- Dec- Jan- Feb- Mar- Apr- May- Jun07 07 07 07 07 07 08 08 08 08 08 08 Full term (39-41 weeks) Jul- Aug- Sep- Oct- Nov- Dec- Jan- Feb- Mar- Apr- May- Jun08 08 08 08 08 08 09 09 09 09 09 09 Near term (36-38 weeks) Jul09 Ohio births at 36-38 weeks gestation following induction, with no apparent medical indication for delivery, by OPQC member status September 2008 to June 2009 Non-member hospitals = 0.1% decrease/mo 20 18 16 14 Percent 12 10 8 Member hospitals = 0.3% decrease/mo 6 4 2 0 Sep-08 Oct-08 Nov-08 Dec-08 Non-member Jan-09 Member Feb-09 Mar-09 Apr-09 Linear (Non-member ) May-09 Linear (Member ) Jun-09 Jul-09 Aug-09 % charts with risks and benefits of scheduled birth documented % charts with method of EDC determination documented % charts with optimal criteria for gest age determination July 2008 February 2009 Obstetrical best practices Establish dates early with ACOG criteria (1999 PB) Patient education Establish hospital policies for scheduled births The Labor & Delivery front desk Document benefits and risks of scheduled births Signed consent in chart Improve communication with pediatricians Physician-to-physician before and after birth Expand schedule to weekends