Complications of Pregnancy - Calgary Emergency Medicine
advertisement

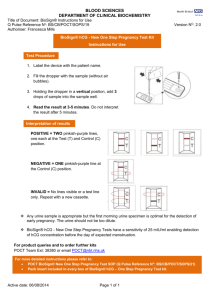
Complications of Pregnancy Lee Graham January 22, 2009 What’s Covered • • • • • Miscarriage Ectopic Hyperemesis preeclampsia/eclampsia/HELLP Throboembolus What’s not covered • • • • • • • Abruption Previa Amniotic fluid embolism Surgical disease of pregnancy Fetal monitoring Delivery US Case 1 • 32 yo with vaginal bleeding • ~7/52 pregnant – (positive home preg test 1 week ago) – no prenatal care • Vaginal spotting X 2 days • Diffuse abdominal cramping 2hrs before arrival • Pmed / Pobs / Psurg = non contributory Case 2 • Vitals = 37 C, HR=93, BP=110/70 • Abdo = soft/non-tender • Pelvic = – Cervic closed – Moderate amount of blood at the os – No adenexal mass and mild cervical motion tenderness Case 2 • US - no visible IUP General approach • In all women presenting with: – – – – Abdominal/pelvic pain Vaginal bleeding Syncope Shock • You must consider the dx of Pregnancy – Obtain a Urine hCG Lower abdominal pain and/or vaginal bleeding - urine hCG + urine hCG Diagnosis of pregnancy • Fertilization occurs in the fallopian tube within minutes to hours after follicular ovulation. • Implantation in the endometrium > ~6 days • Trophoblast secretes hCG > ~7 days • Augments corpus luteal production of progesterone until the trophoblastic production of progesterone is capable of maintaining pregnancy hCG • The initial doubling time is fast – attributed to the actual process of implantation. • This is followed by a slower rate of doubling as trophoblast hCG and maternal circulatory hCG equilibrate • hCG levels peak at 7 to 10 weeks of – mean value of 50,000 IU/L – range of 20,000 to 200,000 IU/L Urine Pregnancy Test • Monoclonal antibodies are selected that act against the purified β subunit of hCG • Sensitivity between 25 and 50 IU/L. • Normal hCG levels in men and premenopausal women range from 0.02 to 0.8 IU/L. • Postmenopausal women may have higher levels. Urine Pregnancy Test • hCG testing becomes positive in 98% of patients 7 days after implantation, which coincides with the time of the expected period. • Negative result 1 week from the expected time of the missed period essentially guarantees that a woman is not pregnant. • Doubling time – 4 wk = 2.2 days (sd ± 0.8 d) – 9 wk = 3.5 days (sd ± 1.2 d) False Positive • postmenopausal status • abortion in the first trimester • exogenous hCG for induction of ovulation • hCG-secreting tumor • Molar pregnancy False Negative • • • • • • • Expired test Too early Murse (color blind) Dilute urine? (SG < 1.010, use 20 drop test) High vitamin C gross hematuria protein > 2+ “Effect of low urine specific gravity on pregnancy testing” • J Am Coll Health 1998 Nov;47(3):138-9. • Urine pregnancy tests with a low urine specific gravity (<1.015) were compared with a serum specimen. • 410 urine specimens were evaluated. Eighty of the women with a specific gravity under 1.015 had negative urine pregnancy tests with a concomitant serum specimen. 0% False Negative. Signs of Pregnancy • Uterine enlargement – – – – – – – – Non pregnant - size of ping pong 4-6 weeks - size of baseball 8-10 weeks - size of softball 12 weeks - symphysis pubis 16 - 20 weeks - umbilicus 36 - 38 weeks xiphoid process of the sternum >38 weeks - fetus descends into the pelvis • Hegar’s sign (6-8 weeks) softening of the lower uterine segment • Chadwick's sign (6-8 weeks) vaginal walls Lower abdominal pain and/or vaginal bleeding Workup as - urine hCG + urine hCG non-pregnant Lower abdominal pain and/or vaginal bleeding Workup as - urine hCG + urine hCG non-pregnant Hemodynamicaly stable Hemodynamicaly unstable Lower abdominal pain and/or vaginal bleeding Workup as - urine hCG + urine hCG non-pregnant Hemodynamicaly stable Hemodynamicaly unstable ?Ruptured ectopic pregnancy or hemorrhage Resuscitate, EDTU and surgical consultation Lower abdominal pain and/or vaginal bleeding Workup as - urine hCG + urine hCG non-pregnant Hemodynamicaly stable Cervix open Or Products of Conception History and physical examination Cervix Closed Ultrasound Ultrasound Inevitable or Complete Miscarriage IUP Miscarriage or Physiologic NonDiagnostic Ectopic Treat Ectopic Pregnancy • Gestation that implants outside the endometrial cavity • Incidence in ED – among women presenting with vaginal bleeding or pain in the first trimester is 10% • 2nd leading cause of maternal death Ectopic Pregnancy • Incidence of ectopic pregnancy is highest in women aged 25 to 34 • The rate is highest among older women and women belonging to minority groups. • Heterotopic pregnancy – Natural birth 1 in 4000 – IVF - 1-4/100 Ectopic and hCG • The embryo grows at a slower rate than normal pregnancies • Usually resulting in a low hCG level and rise • Rupture can occur at any level – Documented at less than 100 mIU/mL – Unruptured ectopics documented at 50,000 Risk Factors • No risk factors in 50% confirmed ectopics • High Odds Ratio – – – – – Previous ectopic pregnancy Previous tubal surgery Tubal ligation Tubal pathology Current IUD use 9.3 - 47 6.0 - 11.5 3.0 - 139 3.5 - 25 1.1 - 45 Risk Factors • Moderate – – – – – Odds Ratio Infertility Previous cervicitis History of pelvic inflammatory disease Multiple sexual partners Smoking 1.1 - 28 2.8 - 3.7 2.1 - 3.0 1.4 - 4.8 2.3 - 3.9 • • Low – Previous pelvic/abdominal surgery – Vaginal douching – Early age of intercourse (<18 years) 0.9 - 3.8 1.1 - 3.1 1.1 - 2.5 Symptoms • In one representative series of 147 patients with ectopic pregnancy • • Abdominal pain (99%) • • Amenorrhea (74%) • • Vaginal bleeding (56%) J Reprod Med 1982 Feb;27(2):101-6. Signs • PE often unremarkable in small, unruptured ectopics • Adnexal masses are felt in only 10% to 20% of patients with ectopic pregnancy • Vital signs – orthostatic changes – occasionally, low grade fever • Mild uterine enlargement • Tenderness – adnexal / cervical motion /abdominal Ectopics and Vaginal Bleeding • Heavy bleeding with clots or tissue usually suggests a threatened or incomplete miscarriage • Endometrial sloughing can be mistaken for passage of fetal tissue (dropping hormone levels) • Passed tissue should be examined in saline Diagnostics • Consider in any female of reproductive age in the ED with – abdo pain – vaginal bleeding – shock – syncope • All women with a positive hCG and these symptoms need an US Ruptured Corpus Luteum Cyst • 1st - trimester bleeding with pain • Corpus luteum normally supports the pregnancy during the first 7 to 8 weeks • Rupture causes pelvic pain and peritoneal irritation • US is helpful if it reveals an IUP (except in patients with in vitro fertilization) Lower abdominal pain and/or vaginal bleeding Workup as - urine hCG + urine hCG non-pregnant Hemodynamicaly stable Cervix open Or Products of Conception History and physical examination Cervix Closed Ultrasound Ultrasound Inevitable or Complete Miscarriage IUP Miscarriage or Physiologic NonDiagnostic Ectopic Treat Non-diagnostic US >1500 Quantitative hCG <1500 Discriminatory zone • Serum hCG level above which a gestational sac SHOULD be visualized by ultrasound examination if an intrauterine pregnancy is present • Institutional dependent – Trans-vaginal 1500 or 2000 IU/L – Trans-abdominal 6500 IU/L Discrimatory zone • -ve US below the discriminatory zone can be – early viable intrauterine pregnancy – ectopic pregnancy – nonviable intrauterine pregnancy • Such cases are termed "pregnancy of unknown location" and 8 to 40 percent are ultimately diagnosed as ectopic pregnancies • Gestatinal sac can be seen as low as 800 hCG rises like an IUP 21% EP Abnormal rise hCG 71% EP hCG 0 Minimal rise IUP hCG falls like a SAB 8% EP 0 Day’s after presentation Minimal fall SAB Non-diagnostic US >1500 Quantitative hCG <1500 Non-diagnostic US >1500 Suspicious mass in adnexa Quantitative hCG No adnexal mass and no IUP Repeat BHCG + and US in 2 days Treat as EP IUP hCG or plateaued Ectopic No IUP hCG decreasing Failed Pregnancy (IUP vs Ectopic) <1500 hCG > 1500 • i)IUP – Visualiztion of IUP rules out ectopic – Exceptions include • heterotopic pregnancies • misdiagnoses – rudimentary uterine horn – Cornua hCG > 1500 • ii)Adnexal Mass – Embryonic cardiac activity or a gestational sac with a definite yolk sac or embryo at an extrauterine location is certain evidence of an ectopic gestation hCG >1500 • • • • iii) Neither NO IUP or Anexal Mass May represent multiple gestations Repeat US and hCG concentration two days later. – No IUP - ABNORMAL – hCG increasing or plateaued - ECTOPIC – hCG decreasing - failed pregnancy • • • • arrested pregnancy, blighted ovum, tubal abortion, spontaneously resolving ectopic Non-diagnostic US >1500 Quantitative hCG <1500 Non-diagnostic US >1500 Quantitative hCG <1500 hCG in 72hr <2X hCG US IUP EP hCG 2X hCG Follow US until IUP or EP Nondiagnostic Failed Pregnancy (IUP vs Ectopic) Failed Pregnancy (IUP vs Ectopic) Weekly hCG until negative Female patient with positive urine BHCG Lower abdominal pain and/or vaginal bleeding Hemodynamicaly stable Cervix open Or Products of Conception Inevitable or Complete Miscarriage Hemodynamicaly unstable History and physical examination Cervix Closed ?Ruptured ectopic pregnancy or hemorrhage Ultrasound IUP Miscarriage or Physiologic bleeding NonDiagnostic Ectopic Treat Resuscitate, EDTU and surgical consultation Management • Surgical vs Methotrexate • Equivalent outcomes • Approximately 35 percent of women with ectopic pregnancy are eligible for medical treatment Ectopic - Medical • MTX is a folic acid antagonist • Inhibits DNA synthesis and cell reproduction, primarily in actively proliferating cells such as malignant cells, trophoblasts, and fetal cells. • Rapidly renally cleared • With renal insufficiency, a single dose of MTX can lead to death or severe complications – bone marrow suppression – acute respiratory distress syndrome – bowel ischemia. Contraindications to MTX • Hemodynamically unstable • Impending or ongoing ectopic mass rupture (ie, severe or persistent abdominal pain or >300 mL of free peritoneal fluid outside the pelvic cavity) • Hematologic, renal or hepatic disease – (need BW before treatment) • Immunodeficiency, active pulmonary disease, peptic ulcer disease • Coexistent viable intrauterine pregnancy • No post-therapeutic monitoring Relative contraindications • High hCG concentration – A high serum hCG concentration is the most important factor associated with treatment failure – hCG concentration greater than 5000 are more likely to require multiple courses of medical therapy or experience treatment failure • Fetal cardiac activity • Large ectopic size (>3.5cm) Follow up • Patients may require multiple doses • Require frequent bloodwork monitoring • Followed until hCG to zero – Can be 2 to 3 months • Patients still at risk of tubal rupture Surgical • Salpingostomy versus salpingectomy • Laparoscopy versus laparotomy • Indications: – – – – – – – Hemodynamic instability Impending or ongoing rupture of ectopic mass Contraindications to use of methotrexate Coexisting intrauterine pregnancy No posttreatment follow-up Desire for permanent contraception Known tubal disease with planned in vitro fertilization for future pregnancy – Failed medical therapy Surgical • Post surgery persistent ectopic pregnancy reported in case series ranges from 4 to 15 percent • Weekly measurement of serum betahCG concentration to r/o persistent disease Case 2 • 25 yr old Female with 1 day of moderate vaginal bleeding • Thought last menstrual period was 6/52 • ROS – Nausea and vomiting X 2/52 – Lower abdo cramping X 3/7 • Pmed / Pobs / Psurg = non contributory Case 2 • Vitals = 37 C, HR=70, 110/60 • Abdo = soft/non-tender • Pelvic = – blood clots in vault – Cervic closed – no adenexal mass or tenderness • Positive urine B-HCG Case 2 • Luckily it is during the day and your able to get an Ultrasound showing an IUP Lower abdominal pain and/or vaginal bleeding Workup as - urine hCG + urine hCG non-pregnant Hemodynamicaly stable Cervix open Or Products of Conception Inevitable or Complete Miscarriage Threatened Miscarriage History and physical examination Cervix Closed Ultrasound IUP Nonviable Ectopic NonDiagnostic Treat Miscarriage • 25-30% of pregnancy’s experience 1st trimester bleeding – about half will go on to miscarry – although the risk is probably higher in the emergency department population. • Risk Factors for misscariage – increase in age and parity, the risk of miscarriage also will increase – <20 =12% – >40 = 26% Miscarriage • Cause – uterine malformations – chromosomal abnormalities (40%) – anembryonic gestation • ovum itself never develops • Fetal death precedes clinical miscarriage – Sonographic (8weeks) – Clinically (8-12weeks) Miscarriage • Risk factors – increasing maternal and paternal age, – tobacco and alcohol use, – increased parity, – history of vaginal bleeding; • About 80% of miscarriages occur during the first trimester; the rest occur before 20 weeks of gestation. Workup • CBC – Baseline, quantify degree of bleeding • Type and Screen – Determine Rh type • US – Evaluate fetal health, location, r/o ectopic Physical exam • The cervix should be gently probed with a ring forceps / finger whether the internal os (1.5 cm deep to the external os) is open or closed • Can be safely performed during the first trimester as long as the forceps are used gently and do not penetrate the cervix more than 2 or 3 cm Terminology • • • • <20 weeks = miscarriage >20 weeks = premature birth. Miscarriage versus abortion ~1/3 of pregnancies end before they are even recognized (before the first missed menses) Terminology • Threatened Miscarriage – Bleeding but a closed internal cervical os. – 35% to 50% eventually miscarry • Inevitable Miscarriage – Internal cervical os is open • Incomplete Miscarriage – products of conception are present at the cervical os or in the vaginal canal Terminology • Missed abortion (1st or 2nd trimester fetal death) – in-utero death of the embryo or fetus prior to the 20th week of gestation, with retention – failure to see fetal heart activity in a fetus with at least a 5-mm crown-rump length • Complete Miscariage – Uterus has expelled all fetal and placental material, the cervix is closed, and the uterus is contracted • Blighted ovum = anembryonic gestation – suspected with gestational sac > 25 mm with no fetal pole gestation • Septic Miscariage - maternal infection Terminology • Lithopedian - ? Stone baby • Ectopic pregnancy, is too large to be reabsorbed by the body, and calcifies on the outside, shielding the mother's body from the dead tissue of the baby and preventing infection • Fewer than 300 cases have been noted in 400 years of medical literature. Lower abdominal pain and/or vaginal bleeding Workup as - urine hCG + urine hCG non-pregnant Hemodynamicaly stable Cervix open Or Products of Conception Inevitable or Complete Miscarriage Threatened Miscarriage History and physical examination Cervix Closed Ultrasound IUP Nonviable Ectopic NonDiagnostic Treat **If patient utilizing artificial reproductive assistance consider dx of Heterotopic Pregnancy IUP Pelvic Exam Internal Os CLOSED Threated Miscarriage Internal Os OPEN Inevitable Miscarriage Products Of Conception Incomplete Miscarriage Vs Complete Miscarriage Signs of Infection Cervical or Vaginal Bleeding Septic Miscarriage Threatened Miscarriage • Bleeding • Pain • Etiology of bleeding often cannot be determined and is frequently attributed to marginal separation of the placenta • With fetal cardiac activity and vaginal bleeding – 7 weeks 90% success – 11 weeks 96% success Hum Reprod 1997 Dec;12(12):2820-3. Threatened Abortion • Serial U/S and hCG if no definitive IUP seen on u/s (r/o out ectopic) • Managed expectantly until: A) their symptoms resolve or B) progression to an inevitable, incomplete, or complete abortion. Threatened Abortion • Return immediately for fever, abdominal pain, or a significant increase in bleeding. • If the patient passes tissue, it should be brought to a provider to examine for POCs, because differentiation of fetal parts or villi from decidual slough or casts is difficult. Threatened abortion • No evidence for bedrest • Women are advised to maintain pelvic rest (ie, nothing per vagina) until two weeks after evacuation or passage of the products of conception, at which time coitus and use of tampons may be resumed Threatened Abortion • Patient counseling is paramount with threatened miscarriage. • Patients should be reassured that they have done nothing to cause miscarriage. Complete vs Incomplete • <12 weeks – common for the entire contents of the uterus to be expelled – one third of all cases are complete • >12 weeks • significant amounts of placental tissue may be retained Incomplete, Inevitable, Missed • Management: – Surgical, Medical or Expectant • All effective • Surgical > Medical > Expectant • MIST trail (RCT comparing all three groups) – Rate of infection in all three groups 2-3% BMJ. 2006 May 27;332(7552):1235-40. Epub 2006 May 17. Surgical • INDICATIONS: – patient does not want to wait for spontaneous or medically induced evacuation of the uterus – heavy bleeding or intrauterine sepsis in whom delaying therapy could be harmful. • Pre-operative ab reduce the risk of postabortal sepsis – doxycycline (100 mg orally for two doses 12 hours apart on the day of the surgical procedure) Medical • Misoprostol (a prostaglandin E1 analog) that acts by causing uterine contractions, which evacuate the uterine contents. • Misoprostol 400 mcg per vagina every four hours for four doses Expectant • Less than 13 weeks of gestation who have stable vital signs and no evidence of infection • Recent cochrane review: – higher risk of incomplete miscarriage – need for unplanned surgical emptying of the uterus – increased bleeding – reasonable approach if the woman preferred nonintervention Complete Miscarriage • Less than 20 weeks • Closed cervix • And any of: – intact gestation is passed and recognized • Send tissue for Pathology – dilation and curettage (D&C) – a sonogram demonstrating an empty uterus with a prior known intrauterine pregnancy (IUP) – or by reversion to a “negative” pregnancy test Complete Miscarriage • Difficult to dx in ED • The routine use of ultrasound in women who were thought to have a complete miscarriage by clinical criteria—closed cervical os and decreasing pain and bleeding after reported or observed passage of tissue—has found that up to 30% will have retained products of conception • Follow serial BHCG b/c could be ectopic Septic Miscarriage • Stabilizing the patient • Obtaining blood and endometrial cultures • Gram +ves, -ves, anaerobes, STD bugs – clindamycin + gentamycin ampicillin Hemorrhagic shock • • • • • • Resuscitate +/- blood Crossmatch PT / PTT STAT O/G consult Oxytocin - Uterine contraction and vasoconstriction – 20 - 40 units / 1L NS: run at 500-1000 ml/hr • Methyergonovine - Vasoconstriction and increased uterine contractions – 0.2mg im/po/iv Prognosis • Most, but not all, studies have found an association between first trimester bleeding and various adverse outcomes (eg, miscarriage, preterm birth, premature rupture of membranes, growth restriction) later in pregnancy. • The overall risk of miscarriage in future pregnancy is approximately 20 percent after one miscarriage, 28 percent after two miscarriages, and 43 percent after three or more miscarriages Counseling • Validate feelings of loss and guilt – Warn about anniversary phenomenon • Emphasize that guilt is unfounded – NOT caused by stress, exercise, trauma, sexual activity • Risk minimization for FUTURE pregnancies – Emphasize prenatal care – Early treatment of infections • Complications: – Bleeding, retained POC, infection Who can wait until tomorrow • • • • • minimal pain minimal bleeding easy to RTED no strong risks for ectopic no strong findings of ectopic – unilateral pain, tenderness, mass Rh Immunization • When an Rh-negative woman is exposed to an Rhpositive fetus, the woman’s immune system may become stimulated to produce anti-Rh antibodies. • Approximately 15% of women will develop sensitization • events that cause maternal transplacental bleeding – trauma – threatened or spontaneous miscarriage – ectopic pregnancies RhoGAM • RhoGAM = anti-D immune globulin • < 12 weeks gestation = 50 micrograms – No harm giving the full dose • > 12 weeks or unknown how far along the full dose of 300 micrograms. • administer within 72 hours of the sensitization Case 3 • 22 yo G3P4 • 22 weeks pregnant (confirmed with US) • 3 weeks of nausea and vomiting • Had this problem last 2 pregnancies 36.9, P=105, RR=18, BP=110/60 Urine dip = 2+ ketones Nausea and Vomiting • Most common medical condition in pregnancy, affecting 50%–90% of women • Serious causes must be ruled out, – – – – – gastrointestinal genitourinary central nervous system, and toxic/metabolic problems pregnancy related • hydatidiform mole or multiple gestation. Hyperemesis Gravidarum • no clear demarcation between common pregnancy-related "morning sickness" and the infrequent pathologic disorder • Dx hyperemesis gravidarum (HG) – persistent vomiting that leads to weight loss greater than 5% of pre-pregnancy weight – electrolyte imbalance – ketonuria, • occurs in about 1% of pregnancies Hyperemesis Gravidarum • Non-Prescription – Stimulation of the P6 (Neiguan) point • located three-fingers’ breadth proximal to the wrist, has been used for thousands of years by acupuncturists to treat nausea and vomiting from a variety of causes. – Ginger • Powdered ginger (1 to 1.5 grams in divided doses over 24 hours) is more effective than placebo, and equivalent to vitamin B6 (pyridoxine) – Avoidance of triggers – Dietary changes Hyperemesis Treatment • i) Diclectin (up to 4 tablets per day) • iii) Then add Gravol or Promethazine • iv) Dehydration No dehydration IV fluid Multivitamin IV gravol Metoclopromide Zofran Chlorpromazine • v) At any time add non-pharmacological • vi) Thiamine if vomiting > 3/52 Case 4 • 32 yo G3P2, 28 weeks GA • Sent from walk in clinic with hypertension and weight gain (5 lb/past week) • New-onset mild headache, dizziness • V/S T 36.9, HR 115, RR 22, BP 162/98 • Urine dip 2+ protein Hypertensive disorders of Pregnancy • No pre-exsisting HTN • Pre-exsisting HTN • Gestational HTN • Pre-eclampsia • Chronic HTN • Pre-eclampsia (superimposed on chronic) Pre-eclampsia • New onset after 20 weeks of gestation • Hypertension – Systolic blood pressure 140 mmHg or – Diastolic blood pressure 90 mmHg AND • Proteinuria of 0.3 grams or greater in a 24hour urine specimen – A random urine protein determination of 30 mg/dL or 1+ on dipstick is suggestive, but not diagnostic • Edema no longer required - up to 1/3 never develop Etiology • • • • Abnormal placental development Placental ischemia Altered ratio of prostacyclin and thromboxane Platelet aggregation thrombin activation fibrin depostition in systemic vascular be • Vasospasm and thrombosis organ dysfunction Risk Factors • • • • • • Nulliparity Multiple gestations Age extremes DM Molar pregnancy Family history Pre-eclampsia • Clinical spectrum – Mild vs Severe • HELLP / Eclampsia related disease process Severe Pre-eclampsia • DBP > 110 • Persistent proteinuria 2+ • Plus any of the following: – Headache or visual disturbances – Oliguria or increased creatinine – HELLP – Pulmonary edema – Fetal growth retardation Pre-eclampsia Complications • • • • • • • • • • • HELLP Seizures Pulmonary edema CHF Renal Failure DIC HELLP Liver/splenic rupture (congestion) Fetal Premature delivery Placental abruption Pre-eclampsia Complications • Stroke may occur at a systolic BP of 160. • Stroke leading cause of death in preeclampsia. • Pulmonary edema from fluid administration is also a leading cause • Betamethasone should given to women with preeclampsia at 24 to 34 weeks of gestation. HELLP • • • • Hemolysis, Elevated Liver enzymes, Low Platelets ?Severe form of pre-eclampsia. Controversial • 15 to 20% do not have prior hypertension or proteinuria HELLP • • • • • • • • • • Proteinuria Hypertension 86 to 100 82 to 88 RUQ/epigastric pain 40 to 90 Nausea, vomiting 29 to 84 Headache 33 to 61 Visual changes 10 to 20 HELLP • No consensus regarding the degree of laboratory abnormality to dx HELLP – Platelets < 100, 000 – AST > 70 – LDH > 600 or total bili >1.2 – Evidence of hemolysis on peripheral smear or in labs Management • Delivery pregnancies ≥34 weeks of gestation • Nonreassuring tests of fetal status – biophysical profile, fetal heart rate testing • • Presence of severe maternal disease: multiorgan dysfunction, DIC, liver infarction or hemorrhage, renal failure, or abruptio placenta. Management • Platelets if – bleeding or less than 20 – less than 40 before C-section • immediately prior (transient effect) – FFP and PRBC’s as indicated • Dexamethasone 10 mg IV q12h Complications • Progression to other organs / systems – – – – – – DIC — 21 percent Abruption — 16 percent Acute renal failure — 8 percent Pulmonary edema — 6 percent Subcapsular liver hematoma — 1 percent Retinal detachment — 1 percent • Hepatic infarction — AST>1000 to 2000 IU/L • Hepatic Rupture – Presents (usually) as an acute abdomen – 50% mortality Eclampsia • Eclampsia = seizures or coma in the setting of signs and symptoms of preeclampsia without other neuro symptoms. • Almost always self-limiting • Seldom last longer than 3 to 4 minutes • Uusual duration 60 to 75 seconds. • Warning signs for – – – – Headache nausea and vomiting visual disturbances and mean arterial pressure greater than 160 Eclampsia • <32 weeks' gestation, seizures may develop abruptly and hypertension may not be associated • <20 weeks of gestation is rare – ?molar pregnancy or antiphospholipid syndrome • Can occur after delivery – usually during the first 48 hours – Can be 28 days after delivery. Treatment Priniciples • Prevention of maternal hypoxia and trauma • • Manage severe HTN (160/110) – hydralazine • 5 mg IV, followed by 5 to 10 mg Q20 – labetalol • 10 or 20 mg IV followed by 2X Q10 up to 80 mg • • Prevention of recurrent seizures • Eclamptic Seizure • Magnesium sulfate was significantly more effective than either diazepam or phenytoin: • 6g over 15 minutes • 2g/hr infusion – only if a patellar reflex is present – respirations are greater than 12 per minute – urine output is over 100 mL in four hours. Additional seizure • Bolus of 2 grams of magnesium sulfate over 15 to 20 minutes • After 2 doses of Mg – Diazepam can be given at increments of 5 mg – Phenytoin 10-20 mg/kg Eclampsia • Seizures resistant to magnesium • CT head should be performed to exclude cerebral venous thrombosis or an intracranial bleed • Also consider hypertenisve encephlopathy – Fundoscopic examination Magnesium Toxicity • Frequent monitoring – loss of deep tendon reflexes at 4.0-5.0 (mmol/L) – respiratory paralysis at 5-7.5 (mmol/L) – cardiac arrest at 10-12.5 (mmol/L) • Pts with renal disease should have their levels checked every 2-4 hours • If magnesium toxic, – 10 mL IV of 10% calcium gluconate – Hemodialysis lowers magnesium levels to the nontoxic range within 3 to 4 hours. Venous Thromboembolic Disease • There is a 4 to 50-fold increase in the incidence in pregnancy • Occurring in 0.5 to 3.0 per 1000 pregnancies • Spread almost equally across all three trimesters and peripartium Pathophysiology • Stasis – venous pooling and valvular incompetence – compression of large veins by the gravid uterus. • Endothelial injury – Delivery is associated with vascular injury and changes at the uteroplacental surface • Hypercoagulability – increases in factors I, II, VII, VIII, IX, and X – decrease in protein S – increase in resistance to activated protein C in 2nd and 3rd trimesters Clinical Pitfalls • The clinical exam notoriously insensitive and nonspecific • DVT – lower extremity swelling and discomfort are common in advanced pregnancy • PE – Dyspnea in up to 70 percent of normal pregnancies • Wells Score has not been validated in pregnancy. D-Dimer • High Negative predictive value of a normal Ddimer when combined with a low pretest probability of VTE. • 149 pregnant women presenting with suspected DVT, in whom this diagnosis was ruled out by US. D-Dimer NEGATIVE in • First 100% • Second 76% • Third 49% Ann Intern Med. 2007 Aug 7;147(3):165-70. Work Up • Treatments for DVT and submassive PE are identical • If you Dx DVT. Stop diagnostics and treat. • If DVT -ve. You must continue. – <30% with PE have DVT at presentation Imaging • No census - CT vs V/Q • Lack of prospective studies in the pregnant population, • However - preference of CT – superior performance in the general population – availability – and safety profile in pregnancy (less radiation exposure to fetus) Imaging • Radiation dose to the fetus is 3 to 131 mcGy • Less than those calculated for V/Q scanning (<55mcGy) • ~Fetal radiation exposure a chest radiograph, V/Q scanning, and pulmonary arteriography is less than 5000 mcGy – <100 to 200 X dose of fetal anomalies. • Possible small increase in the risk of childhood leukemia from 1 in 2800 (baseline risk) to 1 in 2000 Radiology 2002 Aug;224(2):487-92. Treatment • • • • Heparin - doesn’t cross placenta/breast milk SC LMWH - in most IV UFH - hypotension due to acute PE or an elevated risk of bleeding • • IV UFH or SC UFH with severe renal failure • Thrombolytic therapy – with life-threatening acute PE • persistent and severe hypotension due to the PE – maternal mortality rate = 1%