the whole conference report here
advertisement

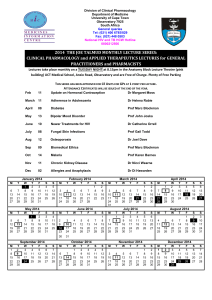
A report of the First International Conference on: Global Health Futures: Creating integrated solutions to the epidemic of long-term disease 13th-15th November 2013, Marriott Hotel, Bengaluru, India The recently Global Burden of Disease report published in the Lancet shows, while people are living longer, chronic illness is on the rise across the world. The College of Medicine and SOUKYA bought together experts from across the globe to tackle the issues around long-term illness and to formulate solutions (See Appendix 3 “The Bangalore Declaration”) Key themes: Modern conventional medicine cannot provide all the answers and sustainable integrated solutions are the only option. The current health systems across the world are unaffordable and can’t match the epidemic in long term disease, high tech solutions are not the answer for long-term disease. Integrated solutions go beyond medicine. Whole-person care, patient information and guided self-care need to be taken more seriously in solutions of long term disease. We need to focus on how health and wellbeing are produced and to consider culturally relevant healing traditions Lifestyle approaches as treatment, not prevention. These low-tech, low cost interventions now have a compelling evidence base. The need to explore preventative solutions that help people to manage the risks of developing long term conditions. Importance of evidence-based medicine (EBM). The best medicine integrates clinical expertise and compassion with best available evidence. The future of integrated care needs to include: evidence, education, regulation of practitioners and products, accreditation, changes in primary care models, updated treatment guidelines. Asset-based community development offers a global opportunity for health improvement. Well established techniques enable communities to grow, flourish and gain more control over their environments. Action towards health improvement must lead away from an almost total dependency on professional interventions and tools, toward community-building and citizen action. Health is not a product of health systems but of humanness interacting with itself, its environment and its economy. Importance of embracing the digital revolution – Patient Passports where patient own their own record 1 Anything that makes for a more sustainable physical environment will simultaneously be promoting a healthier environment. Speakers included: Sir John Oldham (National Clinical Lead for Quality and Productivity), HRH, The Prince of Wales (video message), His Excellency Dr Bhardway (Governor of Karnataka), Professor Dean Ornish, Dr Michael Dixon, Dr Isaac Mathai, Professor George Lewith, Professor David Peters, Professor Justin Wu and Sir Jonathan Porrit. Closing ceremony attended by Archbishop Desmond Tutu and several Indian ministers and dignitaries. Programme (See Conference Timetable - Appendix 3 ) Day 1: Morning session (Chair Sir Graeme Catto). Welcome address: Integrated health and care: Why does it matter and why have a conference about it. Michael Dixon: Chair, College of Medicine, UK. Key themes: Modern conventional medicine cannot provide all the answers and integrated solutions are the only option for three reasons: 1. Money – The current health systems across the world are unaffordable and can’t match the epidemic in long-term disease. 2. Current solutions aren't working and we don’t have the right criteria for treating long-term conditions. 3. Quality of life issues need to be taken into consideration. We need to create systems that provide care, including guided self-care, comfort and compassion. Integrated medicine - A question of science and belief? Professor George Lewith, University of Southampton, UK. Key themes: We are all living longer with chronic co-morbidities and the present healthcare system is unaffordable. Patients need to be encouraged to participate in guided self-care practices. Complexities of evidence-based medicine (EBM). The best medicine integrates clinical expertise and compassion with best available evidence. Many paradoxes – the implicit assumption that all medicine provided by the NHS is evidence based is untrue – only about 35% of treatments used have a solid evidence-based. (citation?) Patients are the motivators driving integrated care - science will always lag behind clinical demand. 2 We must consider the advance of scientism and learn to have some wisdom about how we manage the interface between basic science and clinical care with the patient as our partners and due respect for scientific advances. Integrated approaches to long-term disease in the West - Australia as an example. Professor Kerryn Phelps. Key themes: Chronic diseases (as throughout the world) are responsible for a large portion of the disease burden in Australia. We need to think more about what individuals can do for themselves rather than what mainstream medicine can do for them. Offered a vision of what integrated healthcare could look like in the future. Needs to include: evidence, education, regulation of practitioners and products, accreditation, changes in primary care models andupdated treatment guidelines. CAM is increasingly popular in Australia (3.8% of population had consulted a therapist in last 2 weeks), but individuals have to pay themselves. Open minded patient-centred integration has not yet been achieved. Good examples of partial integration include SOLARIS, St Vincent’s Prostate Cancer Centre andthe Alfred Cancer Centre. There is very little funding available for CAM research at present – cost effectiveness studies needed. Professional education needs to include an integrated model. Vision of future: Plans need to be whole of life, whole of person (building resilience) and whole of system. Integrating approaches to long-term disease in the East.Prof Ranjit Chaudhury Key themes: Long- term health conditions are increasing in India. Many traditional practices - Ayurveda, Unani, Yoga, Naturopathy, Homeopathy, Siddha, S are recognised by the government. There’s been a change in perception of integrated medicine in recent years owing to: limits of allopathic medicine, the professional middle classes turning to use of traditional medicine, international interest and the commercial potential of traditional medicine. All government hospitals and primary healthcare centres in Delhi provide Ayurvedic and homeopathic services. Some major teaching hospitals also provide Ayurvedic, Unani and homeopathy – all provided by qualified doctors, but although tolerance is increasing there are few fully integrated services. 3 Dr Mathai welcome address: Key themes: Thanked – H.E. Dr Bhardwaj for his deep interest, commitment and understanding of integrative medicine, the sponsors, the media and his late father who taught him how to practice holism. Gave overview of the background to the Global Holistic Summit. Address by Dr Michael Dixon: Key issues: Overview of the key principles of the College of Medicine - Service, science and healing and how these will be areas that will be addressed in the content of the conference. Integrated Medicine involves the best of both worlds gives personalised, patient-centred healthcare. Patients need medicine that includes them, which allows them to be involved in the co-production of better health and care and respects mind set and cultural beliefs of where they live. Integrated solutions go beyond medicine. Patient information and self-care need to be taken more seriously in solutions of long-term disease. We need a “wellness” service not a “sickness” service. The need to explore preventative solutions that help people to manage the risks of developing long-term conditions. Video message from HRH the Prince of Wales: Key messages: Expressed sadness about not being able to attend the conference as he has greatly admired the many ancient traditions of healing in the East. Gratified that integrated solutions to the epidemic of long-term disease are being explored. Expressed gratitude to Dr Mathai and the SOUKYA foundation and the support of the Indian Government. Importance to include the best of both worlds – conventional treatments and traditional complementary approaches. Lifestyle, social (gave example of Hazel Stuteley’s work at Connected Communities) and environmental issues need to be attended to if the health system is to remain financially sustainable. Beauty is a vital ingredient of overall wellbeing – we are what we are surrounded by, as well as what we eat. 4 H.E. Dr Bhardwaj (Governor of Karnataka) released Dr Mathai’s book on women's holistic health to Professor Kerryn Phelps before giving the Inaugural Address: Key issues: Thanks and welcome. India and UK have much in common. We need to work together to find integrated (mind, body, spirit and nature) solutions together for long-term conditions. Emphasised the need for more research. Dr Harry Brunjes (Vice-president, College of Medicine) gave a vote of thanks to all involved on behalf of the College of Medicine. Day 1 – afternoon session (Chair - Dr Michael Dixon) Asset- based community development offers a global opportunity for health improvement. Dr Brian Fisher MBE (HELP project) and Hazel Stuteley OBE (Connecting Communities,C2) Key issues: Health organisations (whether statutory or private) need to be working with the people we serve in the spirit of co-production. We now have evidence how communities add social value. We need to move away from individual healthcare to community. Asset-based (unlike deficit- based approach) working underpins the approach. Explore where resources/ assets are in people/communities and harness for the good of community. C2 helps communities identify their own needs and aspirations and to take action to make aspirations happen and to improve the quality of their lives and the societies of which they are part. HELP approach based very much on Hazel Stuetely’s 7 step approach model, Connected Communities (C2). Principles - start with the issues that matter to people – they identify the agenda. We now have evidence that community development does not only make statutory services more responsive, but also helps tackle health inequalities. It also saves money – social return (SROI: for every £1 invested get £4 back). We need more research and improved health outcomes. Introduced paper co-written by Samueli Institiute about opportunities for global community development (see Appendix 2). 5 Hazel Stuteley OBE(Connected Communities: Gave overview of Falmouth project (including video)“We thought we were doing up houses, we were doing up people's lives” quote from service user. Integrated approaches for musculoskeletal approaches. Rosena Johnston (Chartered physiotherapist, faculty member College of Medicine) Simon Fielding OBE (Osteopath, trustee College of Medicine). The workshop gave an overview of an integrated approach to tackling back pain and a practical demonstration of exercises that can facilitate better spinal health. Key issues: Psychosocial factors play an important role. Risk factors include heavy manual work and poor posture associated with sedentary occupation and obesity. Single mono therapies don't work (analgesics etc). An integrated multi-disc approach which includes exercise, manual therapy, analgesic and self-management provide the best outcome. There is good evidence for behavioural and cognitive interventions such as CBT. The Sarah Key method was demonstrated - a five stage approach to back pain. AYUSH - An introduction to Ayurvedic and other Eastern traditions and techniques. Session Chair - Dr R K Manchanda. The role of Ayurveda in contemporary medical milieu. Professor Gangadharan, Medical Director of the Institute of Ayurveda and Integrative medicine, Bangalore. Key issues: Overview of Ayurveda (literal translation -- the 'Science of Life', - history, origin (1500-1000 BC) discussion and the limitations of science. Traditional approached need a different framework of understanding. Discussed work of the I-AIM Health Centre, Bangalore. Panchakosha - Integrated approach of Yoga therapy. Dr Nagendra H R, Key issues: An overview of the Pancakosha model (five layered existence of human beings) was given for functional integration of different systems of healthcare. Exploration of an integrated approach of yoga therapy. 6 The role of Unani in integrated medicine today. Dr Quamri Dept of General Medicine, Bangalore. Key issues: The presentation gave an overview of the practical application of Unani – a Graeco-Arabic system of medicine which is part of the AYUSH system of medicine. Unani includes a number of modalities including pharmaco therapy (plants - mostly, some minerals and animals), regimental therapy (exercises, massage, cupping, leeches, diaphoresis, bathing and irrigation) dieto therapy and surgery. Unani medicine focuses on the concept of the four humours: phlegm, blood, yellow bile and black bile. Global awareness and usage of Siddha Medicines. Dr Kumaravel A Key issues: Siddha medicine is one of the most ancient medical systems in the world. It is thought to have originated over 2500 years ago in Southern India. Goals are to attain perfection. The philosophy states that all objects (including human body, plants, minerals, animals etc.) are composed of five basic elements viz, Earth, Water, Fire, Air and Sky. It has a unique system of diagnosis. Scope for Integration of Naturopathy in the epidemic of long term diseases. Dr Babu Joseph Key issues: Overview of naturopathy including fasting, massage, water and mud therapy, yoga and meditation. Characteristics of naturopathy - drugless, non-invasive, rational and evidence-based. Chief principle - human body has remarkable recuperative powers when left alone. Fasting abstinence of food except water (sometimes coconut or honey water for period of time). Integrated Medicine and Homeopathy - the Royal London Hospital for Integrated Medicine (RLHIM) Model. Dr Peter Fisher Key issues: The RHLIM is part of University College London/NHS:their services are commissioned by the NHS. Clinical services are based around diagnoses or groups of patients rather than therapies. Services include: Allergy, Children’s, Chronic Fatigue Syndrome, Chronic Pain, Musculoskeletal Medicine, Insomnia, Rheumatology, Skin, Stress and Mood disorder, 7 Women’s and Weight Loss. The services offer homeopathy and a range of other therapies supported by a comprehensive pharmacy service. Context - multi-morbidity is very common which challenges the whole way we think of medicine. Adverse drug events are escalating and poly-pharmacy is a key problem area. Research in homeopathy shown to reduce medication (Rossignol et al., Rossi et al. Sinha et al..) Collecting PROMS (patient related outcome measures) on all patients. Qualitative study is underway exploring what enables/what prevents self-care. A recent survey showed a 98% satisfaction ratio (NHS choices). Keys to success include: Patient-centeredness, quality and safety, innovation - responsive to need, integration - best of complementary and conventional. Discovering and Delivering Novel Ayurvedic Formulation through Contemporary Science and Validation of Ayurvedic formulations - Preclinical to Clinicals. Dr Pralhad Patki Key issues: There is a need for safety and efficacy of Ayurvedic based formulations. The Himalaya Drug Company conducts rigorous clinical testing of all their products at ethically recognised clinical centres as per AYUSH guidelines. Recognised by Indian Government. Research tie- up with universities accredited to grant pHD certificates. Research published in peer-reviewed journals. Outside monitoring - two independent authorities. Their products are GMP and WHO certified (not yet EU). Involved with drug discovery and development. 1. Establishing authenticity 2. Control over the quality of raw materials. 3. Clinical studies to establish safety and efficacy (multi-centre trials). Presently developing a promising drug for HBV virus (hepatitis B) and conducting trials on Curcumin enemas in IBD (Curcumin gets destroyed in small or large intestine if given orally). Also looking at developing immuno-stimulant drugs. Their research agenda takes a ‘Green chemistry approach’ with the aim of removing harmful side-effects. Day 2 Morning Chair – Sir Graeme Catto Overview - lifestyle changes may reverse ageing - Prof Dean Ornish Key issues: Optimal lifestyle program includes nutrition (low fat diet), stress management (yoga, breathing, imagery, meditation), exercise (moderate), love & support (including support groups). 8 The Ornish approach offers lifestyle as treatment, not prevention. Low tech, low cost and effective intervention. Trials have shown the potential of the approach in -reversing heart disease, inhibiting early stage prostate tumour growth and reversing early stage prostate cancer, positively changing gene expression, increasing telomerase increase 10% increases longevity (as telomeres get longer our lives get longer ) positively affect angiogenesis. Lifestyle changes can be better than drugs at preventing and treating Type 2 Diabetes (New England Journal of Med). Explored what enables people to make changes. Scaring people doesn't work and can be counterproductive. Joy of living more effective than fear of dying. Fear is not a sustainable motivator and simply giving information is not enough. Adherence to Ornish programme 8590% (3780 people). Medicare has now authorised coverage for Ornish programme in Diabetes and early prostate cancer. Importance of community/love - Difference between - I llness and We llness (I and we). “The future treatment of long term disease in practice - where, how and by whom” . Sir John Oldham (Clinical lead for Long Term disease, UK) Key issues: In Scotland majority of over 65s have two or more conditions. Majority of over 75s have three or more conditions. LTCs 70% health and social care cost. If growth continues huge proportion of GDP will be spent on coping with LTCs. Need a whole person individualised approach and understand the population. LTCare development programme. Early results show substantive alterations to reduced unplanned admissions and length of stay. 900K saved social care budget Greenwich. Need to embrace the digital revolution. Patient passport: Isle of Wight: barcode gives access to electronic medical record. Patient owns record and gives permission to change. What if patient gave permission to acupuncturist, yoga, nutritionist to put in information… patientslikeme (website) - use social media to start to generate the change. People on average spend three hrs a year with professional, rest of time have to selfmanage. Instead of us doing something to people, do it with people. Eg of self-dialysis project in Sweden. Patients have their own card to manage dialysis machines. 9 Integration in Acute Care Hospital Settings: A Trojan Horse or a Gift Horse? Dr Elad Schiff, Israel Key issues: Few examples of CAM integration in Israel. Find a Trojan horse that will let you enter institution. They used a feasibility pilot study. CM in hospitals can serve as an Archimedean point. CIM provided at all surgery stations: acupuncture, hypnosis, guided imagery. Symptom control. Surgery prep. (guided imagery). All offered free-of-charge. Daily tai chi in central room by doctors. Patients active and empowered. Doctors as models. Burn out workshops for medical team - hypnosis. Teaching medical students. Safety measure. Quality assurance. Ticket in is research. PROMs. Data collected over 2000 patients. Symptom control reduced approx 50%. Treatments more effective when symptoms severe. Now viewed as gift horse which has important role. Integrating the best of Traditional Chinese Medicine (TCM) with conventional healthcare. Professor Justin Wu (Chinese University of Hong Kong) Key issues: Most people in Hong Kong have tried TCM. Gave overview of a big data project of TCM (business model). Integration of biomedical databases using text mining - bioinformatics analysis. Clustering demonstrates the most commonly used herb combinations for specific disease entities, or particular conditions. Currently exploring most popular remedies for treatment of stroke. Then identify patients who have been given the remedies and correlate with clinical outcomes. Conduct an audit. Gave examples of integration. First Institute of CU medicine in Hong Kong. East-West Centre for Research and Education. Integrative Medical Clinic in Prince of Wales Hospital teaching hospital of CU medicine in HK. Two integrative models are provided (lower back pain and stroke rehabilitation). Education provided in TM in medical school. Challenges: clinical governance, quality assurance, liability, credentialing, sharing of patient records and reimbursement. Profile of heart diseases in India. Risk factors recent advances and the role of social health schemes. Dr C N Manjunath (From Sri Jayadeva Institute of Cardiology in Bangalore). Key issues: Shift from communicable disease to non-communicable disease in developing nations. CVDs are expected to be the fastest growing chronic illnesses between 2005 and 2015.CVD now accounts for 25% of deaths. Prevalence of diabetes increasing. Owing to decreasing 10 physical activity, increasing stress levels, smoking (50% males either smoke or chew tobacco, 15% women) and increasing intake of saturated fats and tobacco. Lifestyle changes can be simple and cost effective. Needs holistic, integrated and multidisciplinary approach. Telemedicine network needed to coordinate treatment. Day 2 afternoon Chair - Michael Dixon Integrated approaches to women's health. Mr Michael Dooley, Poundbury Clinic, UK (Chair of Faculty of Women’s Health, College of Medicine) Key issues: Too high proportion of women still die or are maimed in childbirth (30 women will have died and 600 will be maimed through childbirth across world in next 30 mins). Set a challenge -- to save 100 women’s lives and to prevent 1000 fistulas by next conference. Explained role of Faculty of Women's Health - development of integrated care for women, share good and bad practice, encourage EBM, develop affordable care for women, develop MDT meetings and developing training and research. Gave overview of Poundbury Clinic - an integrated clinic for women’s health. Patient-centred care, find a diagnosis if possible, review treatment options, develop a treatment plan, patients choice of practitioners, team work with mutual respect, MDT meetings andeducation and audit. Health of mother environment for the embryo key issue. The first nine months in womb is very important for health of individuals. Excessive weight gain in mother - children prone to obesity. Malnutrition may lead to chronic health problems for baby - high b/p, cholsterol etc. Solution - education, good diet, folic acid and vitamin b12, avoid alcohol and smoking, exercise - not excessive, avoid stress,and havefirst class antenatal care. Worldwide 72.4 million women infertile. Causes - lifestyle issues – obesity (doubles risk of infertility, underweight more of a risk BMI 19-25). Micronutrients for men improves sperm quality. 13% causes infertility caused by smoking. Stress issues play a big part. Five pillar approach - lifestyle, emotional, educational programme, develop a proactive selfmanagement programme. 11 Maximising the benefit of self-care in chronic disease - lessons from the UK. Professor David Peters, University of Westminster (Chair of Self-Care Faculty, College of Medicine) Key issues: Changing pattern of disease in developing world. Chronic diseases are taking over from acute disease and infection (mostly preventable). 60% of adults in England report having a chronic health problem and 80% of GP consultations are taken up by these individuals. Depression a common co-morbidity. Healthcare services we now take for granted will have to be delivered at 60% of the projected costs in 10 years time. The cost of the NHS is doubling every 10 years. Essential we move from treatment to prevention. Caring crisis in UK exemplified by Francis report. 290 recommendations.A recent survey (Pulse) showed that GPs (220) were under significant stress and 41% were exhibiting signs of burn out. Urgent need to look at lifestyle issues – what it is that stops people being well. Need to give people good quality information to enable people to make an informed choice and change behaviour. NHS Mid-life Check/Expert Patient Programme and Self-Care Library housed on College of Medicine website. Information not enough. Good examples: David Reilly, Healing Shift, Age of Enablement, Harry Burns Fifth Wave, College of Medicine’s Innovations Network, got to move system from treatment to prevention. Integrated Self-Care in Family Practice, Culm Valley Surgery (Michael Dixon), Intelligent Waiting Room, Health Facilitator, Altogether Better, SustainCare, Community Prescriber Network, the, Foundation for Positive Mental health andPaul Gilberts Compassion Based Therapy. Can East and West be bridged? Can they learn from each other? Can we develop a convincing story of what universal integrated health and care looks like? Professor Sian Griffiths Key issues: Increasing use of traditional, complementary and alternative medicine in the West (increasing across the globe). TCM very popular in China and throughout Asia. Bejong Declaration called for good communication about TCM and improved regulation, policy and standards, training and education. World Health Assembly also committed to development of TCM. WHO traditional Medicine strategy called for an improved knowledge base and for safety and efficacy to be established. Integrated Medicine Centre at Chinese Medicine looking at these issues. TCM is part of self-care culture. TCM given official recognition at handover of Hong Kong in 1997. Training parallels that of Western Medicine. 1/3rd Western doctors admitted to using TCM for themselves (unofficially majority of people use it). 2005 survey showed 67% of people in Hong Kong using TCM. 16% go to both Western and TCM. TCM is more prevalent in rural areas. Although efficacy established for some therapies (Tai Chi), need more evidence and cost effectiveness trials. 12 Integration achievable through political commitment, creation of policy frameworks, professional and public education and engagement. Developing a model for providing integrated care in Communities. Or, could integration be the “fool's gold? Prof David Colin-Thome Key issues: NHS struggling and not performing as well as it should. Care outcomes not been that good particularly for heart disease and cancer. UK lagging behind other countries. Also significant care crisis. Structural approaches (mergers etc.), reforms and integrative approaches will only work if they make a difference to people. Integrative approaches must be based around the individual needs of individuals and communities. Co-morbidity a major problem in the UK. Have we lost focus of the individual user of the service or are we giving too much focus on provider? How do we shift what we measure so it’s more meaningful to individuals?Consultations need to be a meeting of two experts (rare for this to happen). Patients need to be given more power joint care planning. Community-orientated primary care needed where not only care given to individual but is also a resource for the community. Primary care providers need to come together with some agreed outcomes to create an integrated community based healthcare organisation. Creating the right healing environment for long term disease - presentation by Samueli, USA (video link) Key issues: Spending a lot on healthcare not getting outcomes expected/should. Need new ways of delivering healthcare. Poor health not just owing to ageing population, children also developing chronic diseases earlier. New vision needed - focus on self-care (salutogenesis), balanced within current healthcare system. Salutogenesis - the process through which health and wellbeing are produced – the flip side to pathogenesis (mechanism by which a disease is caused). Studies of regions in world where individuals lived long and healthy lives shows key issues are: psychological resilience and stress management, exercise and rest, optimum nutrition, social cohesion - physical environment (non toxic) andspiritual environment. Relaxation/biofeedback/mindfulness – very helpful to improve stress. Top four factors -not smoking, maintaining healthy weight, exercise, fruit and veg (7). Two examples from Samueli Institute: Samueli EG Total Force Fitness (army) and the Well Community Project Framework (Brian Fisher to provide examples). 13 Day 3 (15/11/13) Morning Chair Professor David Colin-Thome Integration, healing and soul, Dr Kim Jobst, UK Key issues: Meaning determines everything that takes place in our lives and is central to the healthcare revolution we are presently experiencing. Although, we’re facing a crisis with healthcare, environmentally and many other different levels this also gives an opportunity. Disease is a healthy manifestation of something that needs to change. Disease is a manifestation of health. Understanding this facilitates transformation at the level of mind, body and soul. We need to realise our own uniqueness at an individual and community level. We all have our own unique self-healing capacity (pharmacopeia) in our own human body. Exploring these issues enables transformation to take place at the deepest level. How can integrated approaches become more effective? -Woodson Merrell, Director of Integrative Medicine, Continuum Centre for Health and Healing (CCHH), New York Key issues: Integrative approach at the CCHH: Stress management, diet/nutritional status, detoxification, exercise, rest and connectedness (social support system). Evidence exists for : Lifestyle medicine (Dean Ornish etc.), a vegan diet (Kjelden-Kragh, J), environmental toxins - (EWG U.S.), nutritional deficiencies, turmeric and herbs, acupuncture for analgesia, hypnosis QOL benefits, glucosamine beneficial in moderate to severe pain after six weeks. Continuum Centre for Health and Healing, New York was established in 2000. 35 practitioners all licensed and credentialed. Includes research, education and training. Including cost effectiveness studies. Key ingredients to success: Find champions - leading physicians, Deans, Donor, legislative (political). Closed with Physician's Prayer, Rachel Naomi Remen MD Creating a more healthy and sustainable physical environment - How do we do it and what are our respective roles? Sir Jonathon Porritt, Chairman of the UK Sustainable Development Commission Key issues: Anything that makes for a more sustainable physical environment will simultaneously be promoting a healthier environment. Healthcare professionals must engage both at the local level to promote ‘health creating communities’ and with education to help shape healthier lifestyles through schools and colleges. 14 Much research into how nature can accelerate the healing process. Fish tanks in doctors waiting rooms- small one has marked effect on reported stress – the bigger the fish tank the bigger the effect! Same effects when having contact with virtual images of nature, urban woodland. Need to have a more holistic appraisal of cost benefits. Nothing changes without fighting existing reality. Need to act as well as reflect – need to go on fighting. Test of a good healthcare system is the degree to which healthcare professionals engage with everyone else outside the system. Preventing Coronary Heart Disease – A combined approach . Dr Vijay Kakkar (awarded OBE in 2009 for services to medicine) Key issues: CV disease in India increasing - doubling of mortality expected in next decade. Current strategies only provide partial protection. It’s now accepted that atherosclerosis is a chronic inflammatory disease which may result from chronic infection from bacteria/viruses (often early in life) such as Human Cytomegalic Virus. Intrinsic factors such as lipids, diabetes contribute to an auto-immune response, which can lead to a breakdown of the body's immune systems. This new information has provided unique opportunities for vaccine development. 20 scientists involved in development - including University of London & Bangalore. RCT double-blind trial underway. Published data supports the anti-inflammatory, immune-modulatory and even anticoagulant properties of Ayurvedic therapy. Low dose heparin given as an example of how homeopathy of yesterday (1967) has become allopathy of today (1975 supported by MRC after a multi-centre trial. 1985 given as routine prophylaxis in over 24 countries and in 2005 used in 81 countries saving approximately 1 million lives). Enabling communities to improve their resilience, their self-confidence and their health - Cormac Russell Speaking on behalf of Illinois. Key issues: Health is a political issue; if we are to see global health improvement then we need to shift the conversation from ‘medical problems’ to ‘political’ and ‘communal’ issues. We can’t therefore meaningfully speak about health improvement without also speaking about environmental, democratic, and economic improvements. Action towards health improvement must lead away from an almost total dependency on professional interventions and tools, toward community-building and citizen action. Health is not a product of health systems but of humanness interacting with itself, its environment and its economy. 15 As community building as a tool for health improvement gathers momentum, the medical system should lead by stepping back…but will it? Like all systems, the medical system must consider the harm it does in expecting people to organise themselves and their ailments the way the system organises itself. Mobilising to grow healthfulness in our communities; will demand some level of relinquishment by the medical system of the resources and ground it currently claims for therapeutic purposes. Resources need to flow towards the domain of greatest competence: citizens organised in communities. In essence, this means even if a small portion of medical system budgets were reinvested in community building and away from medical intervention, huge savings should result. Health is not something we bring to people, it is the net result of a community coming together to use what it has to secure what it needs, including medical systems when required. Afternoon Chair Prof. Sian Griffiths The evidence base for community empowerment and health improvement. Dr Brian Fisher – UK Key issues: Asset-based community development offers a global opportunity for health improvement. Well established techniques enable communities to grow, flourish and gain more control over their environments. We have evidence it works - promotes health protection, resilience, health inequalities improved, impact on behavioural change (evidence accumulated by NICE - improved housing, safer cycling, crime, prevent injuries to children). Saves money.(SROI for every £1 pound a local authority invests a value of 15 pounds is created) This work positively affects the health of professionals as well as residents - transforms the way people practice medicine. Helping communities to take charge of their own health and become more resilient in the U.K. Hazel Stuteley, O.B.E. Key issues: C2 programme (Connecting Communities) is an evidence-based programme with a 15 year track record of transforming the health status of disadvantaged communities across the UK. All communities C2 works in are in top 2% of multiple deprivation. Involves a seven step approach - From isolation to transformation through enabling, connecting and listening. 16 C2 works by delivering a lasting culture shift. The focus is on collaborative, integrated, health creation to harness the collective power of residents working as equals with police, education and Local Authority services. The end result is self-managing, stronger and healthier communities. Example: Beacon project (1995-2013) Overall crime rate down 50%, unemployment down 71% etc. "We thought we were doing up houses, but we were doing up lives" Resident, Beacon project. (See Appendix 2) Extending integrated solutions for the community - Suja Issaac, SOUKYA Key issues: The SOUKYA Foundation has been actively involved in community health for over 17 years. They offer a variety of integrated approaches (AYUSH) alongside western medicine, giving what is best from each system of medicine to support individual’s needs. Holistic Wellness Clinic - opened 1998 offering Integrated Medicine Care - Ayurveda, Homeopathy, Naturopathy and Yoga and a range of complementary therapies - moved to SOUKYA (2002) - certified organic farm. NABH Accredited AYUSH Hospital and a model for holistic way of living. Offers employment to local villagers leading to economic independence, encouraging sustainability. SAHAYA (meaning Help) Holistic Integrative Medical Centre (established 2009) Medical care through Ayurveda, Homeopathy, Naturopathy and Yoga. First independently accredited AYUSH Hospital. Integrative Unit at Bangalore Baptist Hospital (Allopathic Hospital) opened 2011. Various outreach programmes have included extending integrated health solutions to 14 villages to date. Education is given to encourage self-care. Accredited Social Health Activists educate rural people about traditional medicine. Free medical camps and geriatric care is also provided in the community. Outreach programmes also serve employees both in the public sector, fire, police, civil, defence, emergency services, transport and aeronautics. Healthcare is provided in schools for the orphaned, under-privileged and destitute children and for their parents and teachers. Education and research: Offer a six month online research methodology course, seminars and workshops. Currently researching most effective protocols for asthma and allergies and homeopathy for addiction problems. 17 Review of Conference by Michael Dixon and George Lewith. Introduced Bangalore declaration (see Appendix 1 at the end of this document) Next steps: 10 international ambassadors to be elected (first 5): Woodson Merryl, New York Rosena Johnston, Singapore Justin Wu - Hong Kong Maria Britto - Canada Kerryn Phelps - Australia. International examples to be included on College of Medicine’s Innovations Network Diploma to be created for clinicians Biomedical course for CTs Delegates taken to Soukya Holistic Health Centre for final stages of conference Closing Ceremony with Archbishop Desmond Tutu and other dignitaries Classical Dance performance by Dr Mallika Sarabhai, one of India’s leading classical dancers Appendix 1: The Bangalore Declaration Integrated health and care should be the right of all not the privilege of the few. To overcome the escalating global epidemic of long-term disease we need to focus first and foremost on preventing illness and improving the health of all people over their life course. Achieving this will require the political will underpinned by a greater focus on: 1. Creating communities in which the physical, social and nutritional environments are integrated to improve individual and community health. 2. Using resources in future health systems judiciously to ensure sustainability and growth. 3. Creating effective, sustainable and functional connections between health service providers, users and policy makers thereby engaging with education, employment, agriculture and the built environment using a common and accessible language. We believe that globally healthcare services will embrace the principle; health and care will be universally accessible and provided as close to the patient’s home and/or workplace as possible. This 18 means prioritising the role of primary care and conserving expensive integrated technology and hospital care for when it is needed. 4. The balance between western medicine and other therapeutic modalities will integrated using an evidence-based approach wherever possible prioritising wellness and the wishes of the individual patient and family. 5. Patients and carers must be enabled to become fully participatory in their health and guided (self) care and supported by appropriate technology. 6. Health systems and the communities they serve should be redesigned to facilitate improved health. 7. Integrated healthcare will respect different cultural belief systems 8. Communities and citizens will be enabled to take more control over their localities and access the “best of both worlds.” 9. Government will be engaged with environments that enable these processes especially with reference to the most vulnerable in our societies. 10. There will be an investment in education and research with an emphasis on cost effectiveness to allow for a level playing field between lifestyle approaches and biomedicine within an integrated healthcare delivery system Appendix 2: Brian Fisher/Samueli Paper (see separate attachement) Appendix 3: Conference timetable "13 November 2013, Day 1" Morning Chair - Sir Graeme Catto 09:00 - 09:20 Integrated Health and Care - Why does it matter & why have a conference about it ? Dr Michael Dixon 09:20 - 09:50 Integrated Medicine - A question of science or belief? Dr George Lewith 09:50 - 10.20 Integrated approaches to long term disease in the West - Australia as an example Prof Kerryn Phelps 10:20 - 10:50 Chaudhury Integrating approaches to long term disease in the East Padma Shri Prof Ranjit 10:50 - 11:10 11:10 - 11:30 Discussion Prof Phelps and Dr Chaudhury faciliated by Dr George Lewith Tea/Coffee 19 11:30 - 13:00 INAUGURAL CEREMONY National Anthem Welcome Address Dr Issac Mathai Lighting of Lamp Introductory Address Dr Michael Dixon VIDEO MESSAGE HRH THE PRINCE OF WALES Swami Sukhabodhananda Dr Sriprakash K S Prof Dean Ornish Sir Graeme Catto Dr R M Varma Prof Kerryn Phelps Dr Issac Mathai's Book Release"by H.E. Dr. H R Bhardwaj, Governor of Karnataka" Vote of Thanks Dr Harry Brunjes National Anthem 13:00 - 14:00 Lunch Afternoon Chair - Dr Michael Dixon 14:00 - 14:30 improvement Asset-based community development offers a global opportunity for health Dr Brian Fisher and Hazel Stuteley 14:30 - 15:00 Johnston Integrated approaches for musculoskeletal problems Simon Fielding and Rosena 15:00 - 16:30 AYUSH - An introduction to Ayurvedic and other Eastern traditions and Techniques Session Chair - Dr R K Manchanda The role of Ayurveda in contemporary medical milieu Dr Gangadharan PanchaKosha - Integrated approach of Yoga therapy Dr Nagendra H R The role of Unani in integrated medicine today Dr M Mohammed Sayeed Global awareness and usage of Siddha Medicines Dr Kumaravel A Scope of Integration of Naturopathy Dr Babu Joseph Integrated Medicine and Homeopathy - The RLHIM Model Dr Peter Fisher 16:30 - 17:00 Tea/Coffee 17:00 - 17:30 Discovering and Delivering Novel Ayurvedic Formulation through Contemporary Science & Validation of Ayurvedic formulations - Preclinical to Clinicals Dr Pralhad Patki 17:30 - 18:00 Thoughts from the day - Discussion Sir Graeme Catto and Prof George Lewith 19:30 - 20:00 Contemporary Dance Performance Attakkalari Centre for Movement Arts 20:00 - 20:15 Overview - Lifestyle changes may reverse ageing Prof Dean Ornish 20:15 PRIVATE DINNER BY INVITATION ONLY "Evening speaker- Vice President, College of Medicine" Dr Harry Brunjes 20 "14 November 2013, Day 2" Morning Chair - Sir Graeme Catto 08:45 - 09:00 Meditation 09:00 - 09:45 Integrated medicine - The new medical imperative Prof Dean Ornish 09:45 - 10:15 "The future treatment of long term disease in practice - where, how and by whom Clinical lead for Long Term disease" Sir John Oldham 10:15 - 10:45 Panel discussion - Making the changes Prof Dean Ornish and Sir John Oldham 10:45 - 11:15 Tea/Coffee 11:15 - 11:45 Integration in Acute Care Hospital Settings : A Trojan Horse or a Gift Horse Dr Elad Schiff 11:45 - 12:15 Integrating the best of Traditional Chinese Medicine with conventional healthcare Prof Justin Wu 12:15 - 12:45 Profile of heart diseases in INDIA Risk factors recent advances and the role of social health schemes Dr C N Manjunath 12:45 - 13:00 Discussion 13:00 - 14:00 Lunch Afternoon Chair - Dr Michael Dixon 14:00 - 14:30 Integrated approaches to women's health Dr Michael Dooley 14:30 - 15:00 Maximising the benefit of self-care in chronic disease - lessons from the UK Prof David Peters 15:00 - 15:30 Can East and West be bridged? Can they learn from each other? Can we develop a convincing story of what universal integrated health and care looks like? Prof Sian Griffiths 15:30 - 16:00 "Developing a model for providing integrated care in communities. Or, could integration be the current 'fool's gold?" Prof David Colin-Thome 16:00- 16:30 Tea/Coffee 16:30 - 16:45 Creating the right healing environment for long term disease - Video Presentation Samueli Institute 16:45 - 17:45 Where Next ? Panel Discussion "Facilitated by Sir Graeme Catto. Panelist - Sir John Oldham, Prof Kerryn Phelps, Dr Elad Schiff, Prof Justin Wu & Dr K S S Bhatt " 18:30 Seminar - Integration / Homeopathy - Venue : SOUKYA " 15 November 2013, Day 3" Morning Chair Prof David Colin-Thome 8:45 - 09:00 Meditation 09:00 - 9:30 "Integrating Mind, Body and Soul " Dr Kim Jobst 09:30 - 10:00 How can integrated approaches become more effective? Dr Woodson Merrell 10:00 - 10:30 Creating a more healthy and sustainable physical environment - How do we do it and what are our respective roles? Sir Jonathon Porritt 10:30 - 11:00 Tea/Coffee 21 11:00 - 11:30 11:30 - 12:00 Systems Health - The Future of Medicine Dr V A Shiva Preventing Coronary Heart Disease - A Combined Approach Dr Vijay Kakkar 12:00 - 12:30 "Enabling communities to improve their resilience, their self-confidence and their health " Dr Cormac Russell 12:30 - 13:30 Lunch Afternoon Chair Prof. Sian Griffiths 13:30 - 14:00 "Outlining the nature of asset-based community development and explore the evidence for its impact on health protection, responsive services and health inequalities" Dr Brian Fisher 14:00 - 14:30 Helping communities to take charge of their own health and become more resilient in the U.K. Hazel Stuteley 14:30 - 15:00 Extending integrated solutions for the community Suja Issac 15:00 - 15:30 How do we create healthy communities? Panel Discussion "Dr Brian Fisher, Sir Jonathon Porritt, Prof David Colin-Thome, Suja Issac and Hazel Stuteley" 15:30 - 16:00 Review of Conference Dr.Michael Dixon and Dr.George Lewith 16:00 Tea/Coffee /Delegates transport to SOUKYA 18:00 - 19:00 Closing Ceremony "Nobel Laureate Archbishop Desmond Tutu, Shri. K. Siddaramaiah Hon'ble Chief Minister, Shri U T Khader Hon'ble Minister of State, Health & Family Welfare GOK, Shri Nilanjan Sanyal Secretary to GOI & Dept of AYUSH and other dignitaries" 19:00 Classical Dance performance Dr Mallika Sarabhai The College of Medicine and SOUKYA are grateful to our lead sponsor/sponsors: Supported by: World Health Organisation Ministry of Health, Government of India Ministry of Health, Government of Karnataka Department of AYUSH, Government of India and Karnataka For more information about the College of Medicine and how to join, visit: www.collegeofmedicine.org.uk For more information about SOUKYA initiatives, visit: www.soukya.com 22