The Dermis and Accessory Structures
advertisement

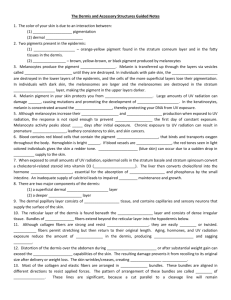
THE DERMIS AND ACCESSORY STRUCTURES Skin Pigment The color of your skin is due to an interaction between: (1) epidermal pigmentation (2) dermal circulation Epidermal Pigmentation Two pigments present in the epidermis: (1) Carotene – orange-yellow pigment found in the stratum corneum layer and in the fatty tissues in the dermis. (2) Melanin – brown, yellow-brown, or black pigment produced by melanocytes Melanocytes *Melanocytes produce the pigment melanin. Melanin is transferred up through the layers via vesicles called melanosomes until they are destroyed. In individuals with pale skin, the melanosomes are destroyed in the lower layers of the epidermis, and the cells of the more superficial layers lose their pigmentation. In individuals with dark skin, the melanosomes are larger and the melanosomes are destroyed in the stratum granulosum layer, making the pigment in the upper layers darker. Melanocytes Melanin pigment in your skin protects you from UV radiation. Long amount of UV radiation can damage DNA, causing mutations and promoting the development of cancer. In the keratinocytes, melanin is concentrated around the nucleus, thereby protecting your DNA from UV exposure. Melanocytes Although melanocytes increase their activity and pigment production when exposed to UV radiation, the response is not rapid enough to prevent sunburn the first day of constant exposure. Melanocyte activity peaks about 10 days after initial exposure. Chronic exposure to UV radiation can result in premature wrinkling, leathery consistency to skin, and skin cancers. Dermal Circulation Blood contains red blood cells that contain the pigment hemoglobin, that binds and transports oxygen throughout the body. Hemoglobin is bright red. If blood vessels are dilated, the red tones seen in light colored individuals gives the skin a redder tone. Cyanosis (blue skin) can occur due to a sudden drop in blood supply to the skin. Epidermis and Vitamin D3 When exposed to small amounts of UV radiation, epidermal cells in the stratum basale and stratum spinosum convert a cholesterol-related steroid into vitamin D3 (choleciferol). The liver then converts choleciferol into the hormone calcitriol, essential for the absorption of calcium and phosphorus by the small intestine. An inadequate supply of calcitriol leads to impaired bone maintenance and growth. The Dermis Two major components: (1) a superficial dermal papillary layer (2) a deeper reticular layer Papillary Layer Consists of areolar tissue, and contains capillaries and sensory neurons that supply the surface of the skin. Reticular Layer Found beneath the papillary layer and consists of dense irregular tissue. Bundles of collagen fibers extend beyond the reticular layer into the hypodermis below. Wrinkles and Stretch Marks Although collagen fibers are strong and resist stretching, they are easily bent or twisted. Elastic fibers permit stretching but then return to their original length. Aging, hormones, and UV radiation exposure reduce the amount of elastin in the dermis, producing wrinkles and sagging skin. Decreased skin turgor, and a sign of dehydration. Stretch Marks Distortion of the dermis over the abdomen during pregnancy of after substantial weight gain can exceed the elastic capabilities of the skin. The resulting damage prevents it from recoiling to its original size after delivery or weight loss. The skin wrinkles/creases, creating stretch marks. Lines of Cleavage Most of the collagen and elastic fibers are arranged in parallel bundles. These bundles are aligned in different directions to resist applied forces. The pattern of arrangement of these bundles are called lines of cleavage. These lines are significant, because a cut parallel to a cleavage line will remain closed, whereas a cut at right angles to the line will be pulled open. Surgeons chose their incision lines based on the lines of cleavage. Dermis Layer – Sensory Receptors Contains many sensory receptors: (1) sensitive to light touch (Meissner’s corpuscles) that are located in the dermal papillae (2) receptors sensitive to deep pressure and vibration (Pacinian corpuscles) Accessory Structures - Hair Hairs are produced from organs called hair follicles. Accessory Structures – Types of Hair Lanugo – extremely fine, unpigmented hairs that form after three months of embryonic development Lanugo is shed before birth and is replaced by: (1) Vellus hairs – fine peach fuzz located throughout the body. Puberty causes some vellus hairs to transition to terminal (airpit, groin, etc) (2) Terminal hairs – heavy, deeply pigmented, sometimes curly hairs (head hair, eyebrows, and eyelashes) Function of Hair Head hair protects scalp from UV radiation and insulates the head Nasal hairs prevent entry of foreign particles into airway (eyelashes perform same function for eyes) A Root hair plexus of sensory nerves allows you to feel even slight movements of each hair shaft Arrector Pili Ribbons of smooth muscle called arrector pili muscles pull on the hair follicles and force the hair to stand erect. Hair Growth Cycle Hairs grow and shed based on hair growth cycle. A scalp hair grows for 2-5 years, at a rate of about 0.33 mm/day Collections of hair can be useful to assay for: (1) lead poisoning (2) arsenic poisoning (3) heavy metal poisoning Healthy adults lose about 50 hairs/day from your head. In males, changing sex hormone level can change terminal hair to vellus hair, in a process called male pattern baldness. Glands Two types of exocrine glands: (1) Sebaceous glands (2) Sweat glands – consists of apocrine and ecrine glands Sebaceous Glands Sebaceous glands are oil glands that discharge a waxy, oily secretion into hair follicles Release sebum (lipids) that inhibit bacterial growth, lubricate keratin (hair/nails), and condition the skin Sebaceous Glands During the last months of fetal development, the sebaceous glands are extremely active and produce secretions to form a protective layer called the vernix casoesea Apocrine Sweat Glands Located in the armpits, around the nipples, and in the groin attached to hairs Produce sticky, cloudy, sometimes odorous secretions The sweat is a nutrient source for bacteria, which intensify the odor Begin secreting at puberty Merocrine/Ecrine Sweat Glands More numerous and widely dispersed than sebaceous glands Palms and soles have greatest number Discharge secretions directly onto skin Merocrine/Ecrine Sweat Glands Function to: 1. Cool the skin through evaporative cooling 2. Excrete water and electrolytes 3. Provide protection to environmental hazards, by diluting harmful chemicals and discouraging growth of bacteria Ceruminous Glands Modified sweat glands in the passageway of the external ear canal Secretions are called cerumen, or earwax Works along with tiny hairs to trap foreign particles and prevent them from reaching the eardrum Nails Form on the dorsal surfaces of fingers and toes Function to protect exposed tips of fingers and toes, and limit their distortion when subjected to mechanical stress, like grabbing objects Nails Nail production occurs at the nail root Underlying blood vessels provide nail its color Small white/pale colored moon called the lunula found at the base of the nail Nails – Indication of Health Can be used to indicate general overall health of an individual EX: yellow nails in individuals with chronic respiratory disorders, thyroid disorders, or AIDS Pitted nails as a result of psoriasis Concave nails as a result of some blood disorders