FRACP Part I Exam Respiratory Teaching Session
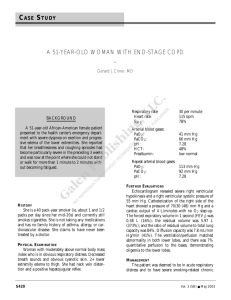
advertisement

FRACP Part I Exam Respiratory Teaching Session Past Papers Review • 1. 2. 3. 4. 5. Options: Excessive PTHrP Secretion Increased Bone Resorpsion Increased 1,25 (OH) Vitamin D Reduced Renal Clearance Minerolocorticoid Deficiency Hypercalcemia in Sarcoidosis • • • Hyperabsorpsion of dietary Ca occurs in 30-50% of Sarcoidosis patients Excessive Ca is initially excreted in urine leading to hypercalciuria 30-50% Sarcoid patients have Hypercalciuria – potentially can lead to nephrocalcinosis – in 50% of renal patients with renal insufficiency – Nephrolithiasis – 1-14%. Initial presenting sx in 4-14% of Sarcoid patients. – Granulomatous interstitial nephritis – most patients have systemic active sarcoid. Renal biopsy shos noncaseating granulomas, mononuclear cells, intersitital fibrosis – Polyuria – nephrogenic or central diabetes insipidis (Pituitary Sarcoid) • • 10-20% have hyperalcemia – aggravated by sunlight exposure Etiology – Increased 1,25 dihydroxyvitamin D production by Monocytes (mainly Macrophages) in lungs and lymph nodes • Mainly due to increased intestinal Ca absorpsion • Increased Bone Resorpsion – Excessive PTHrP also contributes • PTHrP is found in 85% of biopsies of granulomatous tissue • • • • • Which intervention is least likely to improve this gentleman’s problems? A. Thiazide B. Avoidance of Sunlight C. Restriction of Dietary Calcium D. Prednisone E. Reduce Dietary Oxalate Treatment of Hypercalcemia in Sarcoidosis • Treatment Aim: – Reduces intestinal absorption of Ca and – reduce Calcitiol Synthesis • • Restriction of Ca intake (Aim dietary Ca of < 400mg/day) Reduce Oxalate intake – – to prevent marked increase in Oxalate absorption and hyperoxaluria which increases the risk of nephrocalcinosis Eliminate Vit D supplement Avoidance of sun exposure Thiazide diuretic is CONTRAINDICATED in Sarcoidosis – Thiazide is usually used to inhibit hypercalciuria related renal stones – Contraindicated in Sarcoidosis – inhibition of hypercalciuria leads to aggravates underlying hypercalcemia Low-dose Glucocorticoid therapy – inhibition of mononuclear cells and inhibition of Ca absoroption – 10-30mg prenisone is usually adequate in sarcoidsosi – Treatment response: Serum Ca falls within 2 days. – Full hypocalcemic response takes up to 7-10 days Second Line Treatment: – Bisphosphone Choroquine/Hydroxycholorquine to reduce inflammatory activity of the disease • • • • • Asbestosis • Interstitial lung disease secondary to Asbestos exposure • Severity is directly proportionate the amount of asbestos bodies deposited in lung tissue • CT evidence of interlobular thickening. Subpleural based band like densities. • Basilar and Dorsal lung parenchymal interstitial changes – interlobular/ intralobular Asbestos bodies Asbestosis on CT Diagnosis of Pleural TB • Pleural Biopsy – Most sensitive test – – – • • • Pleural Fluid Culture: 42% sensitive Mantoux test – high false negative rate: up to 31% - due to suppression of sensitised T-cells Sputum culture : More likely to be positive in Parenchymal disease – – – • – Sensitivities: 78-95% Useful as an aid to differential diagnosis – in high pretest probability, lymphocytic pleural effusion with negative microbiology on culture and histology Specificity: 95% Interferon- Gamma: – – – • Sensitivity: 20-50% Sensitivity in Patients with Parenchymal disease: 90% Sensitivity in those without parenchymal disease:11 % Adenosine deaminase: – – • Combination of histological exam + Tissue culture – Sensitivity > 90% Plerual biopsy culture is 60% sensitive Histological examination – Granulomatous tissue – 70% sensitive. > 6 samples – sensitivity 80% Sensitivity: 89%, Specificity 97%, Positive likelihood ratio: 23. Useful in differentiating TB pleurisy from other lymphocytic pleural effusions. TB PCR: Sensitivity ranges between 41% to 80%. Expensive. 2003 Respiratory Questions • Benefits of pulmonary rehabilitation in COPD • • • • • • • • • • Improves exercise capacity (Evidence A) Reduces the perceived intensity of breathlessness (Evidence A) Can improve health-related quality of life (Evidence A) Reduces the number of hospitalizations and days in the hospital (Evidence A) Reduces anxiety and depression associated with COPD (Evidence A) Strength and endurance training of the upper limbs improves arm function (Evidence B) Benefits extend well beyond the immediate period of training (Evidence B) Improves survival (Evidence B) Respiratory muscle training is beneficial, especially when combined with general exercise training (Evidence C) Psychosocial intervention is helpful (Evidence C) » Global Initiative for Chronic Obstructive Pulmonary Disease, based on an April1998 meeting of the National Heart, Lung, and Blood Institute and the World Health Organization. LVRS • Feasible in a small subset of severe COPD patients – Highly selective – Upper lobe predominant Emphysema + Poor exercise tolerance – DLCO & FEV1 have to be > 20% • Mortality signicifantly increased in the group with DLCO & FEV1 < 20% • Non upper lobe dominant emphysema has higher mortality rate compared to Placebo group • Severe COPD with good functional status again has increased mortality Inhaled Corticosteroids in COPD 4 Major studies • ISOLDE – – • Lung Health Study – – • N=290 FEV1 86% predicted 1200mcg Budesonide/d for 6 months then 800mcg Budesonide/d for 30 months No Treatment effect on frequency of exacerbation or lung function decline Euroscope Study – – – 1. 2. N=1116. Moderately severe COPD. (FEV1 64% predicted) 1200mcg Inhaled Triamcinolone 1. Less outpatient visits for respiratory complaints 2. Less Respiratory Symptoms 3. Reduction in frequency of severe exacerbations Copenhagen City Lung Study – – – – • N= 751. 1000mcg Fluticasone/d for 6 months No significant difference in FEV1 decline. Small reductionin frequency of exacerbtions and slower rate of decline in health status N=912 FEV1 77% predicted Budesonide 800mcg / day – significantly more dysphonia/ bruising Prolonged therapy with high dose ICS required to achieve modest effects No beneficial effect on disease progression Tiatropium Bromide in COPD • Anticholinergic - M1/ M3 Muscarinic receptor antagonist. Does not block M2 receptor like Iprotropium (M2 facilitates bronchodilatation.) – more symptomatic relief – Fewer exacerbations – Delay in first presentation to hospital with exacerbations when compared with LABA • More bronchodilatation and better symptomatic relief than regular Ipratropium Varenicline • New therapy in smoking cessation • Partial Nicotine Acetylcholine receptor agonist • Patients treated with Varenicline are more likely to achieve both short term and sustained smoking cessation (up to 1 year) when compared with Buproprion or Placebo • OR of Smoking Cessation: Varnicline: 3.2, Buproprion 1.7 Indications for long-term oxygen therapy • General indications – PaO2 55 mmHg or SaO2 88% • In the presence of cor pulmonale – – – – PaO2 59 mmHg or SaO2 89% EKG evidence of P pulmonale Hematocrit >55% Clinical evidence of right heart failure • Specific situations – PaO2 60 mmHg or SaO2 90% with lung disease and other clinical needs such as sleep apnea with nocturnal desaturation not corrected by CPAP. – If the patient meets criteria at rest, O2 should also be prescribed during sleep and exercise, and appropriately titrated.If the patient is normoxemic at rest but desaturates during exercise or sleep (PaO2 55 mmHg), – Consideration of nasal continuous positive airway pressure (CPAP) or bilevel noninvasive nocturnal ventilation is warranted in patients with desaturation during sleep. Fertility in CF CF Male: • 95% have defects in sperm transport Absence of Vas deferens CF Females 20% infertile Due to Thick Cervical Mucus secretions Secondary Amenorrhea Exercise Physiology • VO2 (Oxygen Uptake) VO2 = Cardiac Output x (A-V Oxygen content) VO2 Max • Definition: • the maximum capacity of the cardiovascular system to deliver oxygen to the exercising muscles and the ability of the exercising muscles to consume oxygen at maximum exercise capacity. • VO2 Max is limited by Maximum Cardiac output during exercise • Maximal HR decreases as a function of age: • Maximal HR = 208- 0.7 x age (years) Determination of VO2 Max: • • • • Alveolar Volume (VA) x kCO = DLCO VA= number of contributing alveolar units kCO – efficiency of individual units DLCO: Gas exchange capacity of lung as a whole SVC Obstruction Lung Cancer – Commonest cause for SVC obstruction – 2-5% of lung Cancer patients • • • 20% SCC develop SVC obstruction due to central airways involvement Marker for poor prognosis in NSCLCA – median survival 5 months Management: – – – 1. Lymphoma • 2. Non Hodgkins Lymphoma Mediastinal metastasis 1. 2. 3. 3. Tissue diagnosis, Chemo/Radiotherapy, Endovascular stent – in refractory disease or rapid symptomatic progression Germ Cell Cancer Metastastic Breast Cancer Thymoma Non Malignant Causes 1. 2. Mediastinal Fibrosis – Endovascular stent, SVC bypass surgery Thrombosis of indwelling catheter devices e.g. Pacemaker Etiology of Pancoast’s syndrome • NSCLCA – Commonest – Squamous Cell CA • Lyphoma • TB • Primary Chest wall tumors • Typically T3/T4 on presentation (Involvement of surrounding solid organs) • Investigation: Transthoracic FNA Pancoast tumor • Right Shoulder Pain – Commonest first symptom (44-96%) – invasion into brachial plexus, 1st or 2nd ribs, Vertebral bodies, parietal pleura, chest wall • Horner’s Syndrome – 14-50%. – Paravertebral sympathetic chain and inferior stellate ganglion • Neurological complication of the upper limbs – C8/T1 Nerve root involvement • 10% profound weight loss • 10% have Recurrent laryngeal nerve palsy • Lung Cancer + Pleural Effusion + Liver Mets • T4 (pleural effusion) • * Refer to Lung Cancer Staging Table on UTD CT+PET Scan Is superior to CT alone in Lung Cancer Staging • Useful in assessing mediastinal disease – If there is no mediastinal lymphadenopathy, in the absence of metastasis – stage IIIA, if there is mediastinal disease Stage IIIB – surgical treatment is inappropriate