Peripheral Nerve Injuries
advertisement

Peripheral Nerve Injuries
PATHOLOGY
Nerves can be injured by ischaemia ,compression,
traction, laceration or burning. Damage varies in
severity from transient and quickly recoverable
loss of function to complete interruption and
degeneration.
There may be a mixture of types of damage in the
various fascicles of a single nerve trunk.
Nerve injury and repair
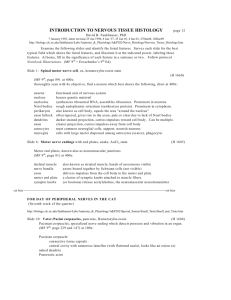
(a) Normal axon and target organ (striated muscle).
(b) Following nerve injury the distal part of the
axon disintegrates and the myelin sheath breaks
up. The nerve cell nucleus becomes eccentric and
Nissl bodies are sparse. (c) New axonal tendrills
grow into the mass of proliferating Schwann cells.
One of the tendrill will find its way into the old
endoneurial tube and (d) the axon will slowly
regenerate.
Nerve injury and repair
Introduction
Anatomy
Peripheral nerves are made up of
axon
endoneurium
Connective tissue perineurium
epineurium
Nerve trunks myelinated fibre
unmyelinated fibre
Myelin, protein-lipid complex
function, insulating layer
increase conduction rate
axon
Ranvier node
Myelinated nerve are separated by nodes of
Ranvier, at these points , the axons are bare.
Impulses jump from one node to the next --Saltatory Conduction
Conduction in unmyelinated nerve is slower and
dependent on the diameter of axon.
Pathological processes
Cause: damage of cell body,axon, myelin
sheath, connective tissue, blood supply
Three basic processes
1. Wallerian degeneration
2. Axon degeneration
3. Demyelination
Nerve injuries types
Neurapraxia
Axonotmesis
Neurotmesis
Neurapraxia
Seddon(1942) coined the term 'neurapraxia' to
describe a reversible physiological nerve
conduction block in which there is loss of some
types of sensation and'muscle power followed by
spontaneous recovery after a few days or weeks.
It is due to mechanical pressure causing
segmental demyelination and is seen typically in
'crutch palsy', pres- sure paralysis in states of
drunkenness ('Saturday night palsy') and the
milder types of tourniquet palsy.
Neurotmesis
In Seddon's original classification, neurotmesis
meant division of the nerve trunk, such as may
occur in an open wound. It is now recognized
that severe degrees of damage may be inflicted
without actually dividing the nerve. If the injury is
more severe, whether the nerve is in continuity
or not, recovery will not occur. As in
axonotmesis, there is rapid wallerian
degeneration, but here the endoneurial tubes
are destroyed over a variable segment and
scarring thwarts
CLASSIFICATION OF NERVE INJURIES
Seddon's description of the three different types of
nerve injury (neurapraxia, axonotmesis and
neurotmesis) served as a useful classification for
many years. Increasingly, however, it has been
recognized that many cases fall into an area
somewhere between axonotmesis and
neurotmesis. Therefore, following Sunderland, a
more practical classification is offered here.
First degree injury This embraces transient
ischaemia and neurapraxia, the effects of which
are reversible.
Second
degree injuryOF
ThisNERVE
corresponds
to
CLASSIFICATION
INJURIES
Seddon's axonotmesis. Axonal degeneration
takes place but, because the endoneurium is
preserved, regeneration can, lead to complete,
or near complete, recovery without the need for
intervention.
Third degree injury This is worse than
axonotmesis. The endoneurium is disrupted but
the perineurial sheaths are intact and internal
damage is limited. The chances of the axons
reaching their targets are good, but fibro- sis and
crossed connections will limit recovery.
1.Wallerian degeneration
Distal axon degeneration, following
section
or
severe
injury,
with
degeneration of the myelin. The process
occurs within 7-10 days of injury and this
portion of the nerve is inexcitable
electrically.
2. axon degeneration
Distal
degenerated
inexcitable electrically.
nerve
is
Regeneration can occur since the
basement membrane of the Schwann cell
survives and act as a skeleton along
which tha axon regrows up to a rate of
about 1mm per day.
3. Demyelination
Segmental destruction of the myelin sheath
occurs without axonal damage. The primary
lesion affects the Schwann cell and causes
marked slowing of conduction or conduction
block.
Local demyelination is caused by
inflammation, eg: Guillain-Barre syndrome.
Symptoms of PNS
Sensory symptoms
Motor symptoms
Negative symptoms:
Large myelinated fibre disease (loss of touch and jointposition sense, proprioception) leading to:
Difficulty discriminating textures
feet and hands feeling like “cotton wool”
Gait unsteady through loss of position sense
Small unmyelinated fibre disease (loss of pain and
temperature appreciation), causes
Painless burns and trauma
Damage to joints (Charcot’s joint ), resulting in painless
deformity
Positive symptoms
Large myelinated fibre disease cause paraesthesia (
pins and needles) .
Small unmyelinated fibre disease produce painful
positive symptoms:
Burning sensation
Dysaesthesia—pain on gentle touch
Hyperalgesia—lowered threshold to pain
Hyperpathia—pain threshold is elevated but pain is
excessively felt
Lightening pains—sudden, very severe, shooting pains,
which usually suggest a diagnosis of tabes dorsalis (late
syphilis)
Motor symptoms:
Weakness—the main presenting feature,
usually distal (e.g. difficulty clearing the kerb
when walking or weak hands)
Sometimes can be proximal (e.g. difficulty
climbing stairs or combing hair)
Cramps and twitching of muscles
(fasciculation) more commonly due to
neuronopathies (diseases affecting the
anterior horn cell, eg. motor neuron disease)
Signs of Peripheral Neuropathy
Sensory examination:
Large myelinated sensory fibres include:
Light touch
two-point discrimination
Vibration sense
Joint-Position sense
Small unmyelinated and thinly myelinated
sensory fibres include:
Temperature perception
Pain perception
Polyneuropathy: “glove-and-stocking”
distribution of sensory loss.
Joint-position sense is lost, gait is abnormal
(sensory ataxia), Romberg’s test (+). It can be
compensated for by vision, therefore the stance
becomes unsteady when the eyes are closed.
Motor examination:
Classical features of a lower motor neuron
abnormality include:
Distal Wasting of muscles, can occur with
generalized weight loss, but weakness is rare.
Weakness of muscles
Depressed or absent tendon reflex
Fasciculation
Investigation of peripheral neuropathy
Blood tests: FBC, ESR, CRP, urea and electrolytes, liver
function tests, VitB12、protein electrophoresis.
Nerve conduction studies -differentiate axonal
degeneration (reduced amplitude) from demyelination
(reduced conduction velocity). Characterize whether
sensory motor fibres; localize the sites of abnormality.
Electromyography (EMG): discern complete of partial
denervation /reinnervation; localization depending on the
distribution of muscles affected.
Nerve biopsy:
sural nerve is the one most commonly biopsied
provided that its conduction is abnormal.
Cerebrospinal fluid (CSF) examination:
Guillain-Barre syndrome or chronic inflammatory
demyelinating polyradiculoneuropathy: protein
content is usually raised.
Trigeminal Neuralgia
Introduction
A severe paroxysmal facial pain syndrome
Pain is confined mainly to the area supplied by the
second and third divisions of trigeminal nerve.
Characteristically, lightninglike momentary jabs of
excruciating pain occur and spontaneously abate.
Develops in middle to later life
Uncertain cause.Microvascular compression is the
cause in some cases.
Clinical features
—Most patients are over 40 years old
—Female more than male, 3:2 or 2:1
—Pain area: in a maxillary or mandible distribution , most
are unilateral
—Pain quality: severe paroxysmal lightninglike jabs of
excruciating pain and stop spontaneously. Pain-free
Interval may last for minutes to weeks.
—Trigger zones: cheek, nose or mouth by touch, cold, wind,
drinking, talking or chewing can precipitate the pain.
—Long-term relapse and remission course
—Physical examination: no abnormal signs.
Treatment
Carbamazepine 600-800 mg/d orally is
preferred. Side effects include drowsiness,
unsteadiness of gait, nausea, vomiting.
Phenytoin 200-400mg/d orally is the second
choice, can combine with carbamazepine.
Intravenous administration of phenytoin 250mg
will abort an acute attack.
Lamotrigine 400mg/d or baclofen 10mg t.i.d has
been used in refractory cases.
Posterior fossa microvascular decompressive
surgery has been used in drug-resistant cases.
Bell’s palsy (Idiopathic facial palsy)
Facial nerve or nerve sheath swell may be
the reason of Bell’s palsy.
The cause is unclear, but it associated with
cooling, viral infection (herps simplex virus
type 1 in the geniculate ganglion) and
diabetes.
Clinical Features
—Abruptly unilateral paralysis of muscles supplied by
facial nerve, presenting with reduced wrinkling
action, inability of closing the eye, loss of nasolabial
fold, dropping of the side of mouth, weak cheek.
—Generally is preceded or accompanied by pain about
the ear.
—Maybe accompanied impairment of taste, lacrimation
or hyperacusis according to the lesion site.
—Physical examination: facial weakness, rare other
abnormality.
Diagnosis
Treatrnent
Exclude tumors that
might compress the
nerve.
Most patients can recover
spontaneously.
Prednisone: 60mg/d orally for
3 days, tapering over the next
7 days.
For patients who have a poor
prognosis suggested by
severe pain at onset and EMG
evidence of denervation.
Acyclovir or other antiviral
agents are not confirmed.
Acute inflammatory demyelinating
Polyradiculoneuropathy (GuillainBarre syndrome, GBS)
Introduction
Acute/subacute onset
Inflammatory demyelinating
polyradiculoneuropathy
Symmetrical, progressive lower motor neurons
paralysis of limbs.
Etiology and Pathology
Commonly preceded by viral infection,
vaccination to 1-4 weeks.
It appears to be an immunological basis.
Pathological lesion are demyelinating on
anterior roots and peripheral nerves
sometimes with axonal degeneration.
Clinical findings
1. Weakness: symmetrically begins with legs, usually
severer in proximal than in distal of lower neurons
lesion (hypotonia, hyporeflexia, wasting of affected
muscles). The respiratory muscles palsy may be
involved and cause respiratory failure, which is life
threatening.
2. Sensory involvement: distal and symmetrical, as
glove-and-stocking sensory loss, usually less
marked than motor symptoms.
3. Cranial nerves involvement: produce
ophthalmologic, facial palsy, bulbar palsy that
predisposes to aspiration pneumonia.
oculormotor nerve: Ⅲ、Ⅳ、Ⅵ
facial nerve:
Ⅷ
bulbar palsy: Ⅸ、Ⅹ
4. Autonomic dysfunction: tachycardia, cardiac
irregularities, labile blood pressure, disturbed
sweating, sphincter disturbance are rare.
5. CSF: albuminocytologic dissociation: a
characteristic abnormality, with increased protein
concentration but a normal cell count.
Diagnosis
Progressive weakness of more than one limb
Distal or proximal hyporeflexia
Relatively symmetrical deficit
Mild sensory involvement
Cranial nerve involvement
Recovery beginning within 4 weeks after progression
stops
Autonomic dysfunction
No fever at onset
CSF albuminocytologic dissociation
Nerve conduction slowing or block by several weeks
Treatment
1. Plasmapheresis. May reduce the time required for
recovery or decrease the likelihood of residual
neurologic dificits.
2. Intravenous large dose of immunoglobulin 0.4g/kg/d
for persistent 5~7 days appears to be equally effective.
The two therapies are not additive.
3. Symptomatic therapy:
closely monitor and assist respiration. If patient is short
of breath, the vital capacity falls below about 1L, blood
oxygen saturation declines to 80% or oxygen pressure
lower 70mmHg. The tracheotomy is necessary for
patients with respiratory canal blocked by secretion or
sputum.
Sometimes treatment with pressor agents is
required to counter hypotension
Low-dose heparin may help to prevent
pulmonary embolism.
4. Corticosteroids may affect the outcome
adversely or delay recovery, and are not
indicated.
Prognosis:
Self-limiting and cease to progress by about 4
weeks, improvement occurs over weeks or
months following onset.
70-75% of patients recover completely, 25% are
left with mild neurological deficits, and 5%
die,usually as a result of respiratory failure.
Poor prognosis: Campylobacter jejuni infection,
axonal degeration,more rapid onset of
symptoms, the need for ventilatory support.