Thyroid & Pregnancy
advertisement

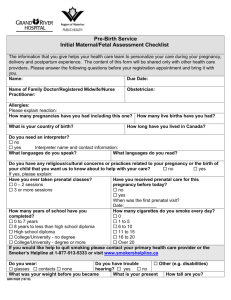
HORMONAL DISORDERS OF PREGNANCY Thyroid & Pregnancy: Normal Physiology • Increased estrogen increased TBG (peaks wk 15-20) • Higher total T4 & T3: • normal FT4 & FT3 if normal thyroid fn. and good assay • hCG peak end of 1st trimester, hCG has weak TSH agonist effect so may cause: • slight goitre • mild TSH suppression (0.1-0.4 mU/L) in 9% of preg • mild FT4 rise in 14% of preg Thyroid & Pregnancy: Normal Physiology • Fetal thyroid starts working at 12-14 wks • T4 & T3 cross placenta but do so minimally • Cross placenta well: • MTZ > PTU • TSH-R Ab (stim or block) • ATD (PTU & MTZ): • Fetal goitre (can compress trachea after birth) • MTZ aplasia cutis scalp defects • Other MTZ reported embryopathy: choanal atresia, esophageal atresia, tracheo-esophageal fistula • Therefore do NOT use MTZ during pregnancy, use PTU instead Thyroid & Pregnancy: Hypothyroidism • 85% will need increase in LT4 dose during pregnancy due to increased TBG levels (ave dose increase 48%) • Risks: • increased spont abort, HTN/preeclampsia, abruption, anemia, postpartum hemorrhage, preterm labour, baby SGA • Fetal neuropsychological development (NEJM, 341(8):549-555, Aug 31, 2001): – Cognitive testing of children age 7-9 – Untreated hyothyroid mothers vs. normal mothers: » Average of 7 IQ points less in children » Increased risk of IQ < 85 (19% vs. 5%) – Retrospective study, data-dredging? LT4 dose adjustment in Pregnancy: - Optimize TSH preconception (0.4 – 4.0 mU/L) - TSH at pregnancy diagnosis (~3-4 wk gestation), q1mos during 1st 20 wks and after any LT4 dose change, q2mos 20 wks to term - Instruct women to take 2 extra thyroid pills/wk (q Mon, Thurs) for 29% dose increase once pregnancy suspected (+ commercial preg test) - If starting LT4 during preg: initial dose 2 ug/kg/d and recheck TSH q4wk until euthythyroid TSH Dose Adjustment TSH increased but < 10 Increase dose by 50 ug/d TSH 10-20 TSH > 20 Increase dose by 50-75 ug/d Increase dose by 100 ug/d Pregnancy: screen for thyroid dysfn ? • Universal screening not currently recommended: • ACOG, AACE, Endo Society, ATA • Controversial! • Definitely screen: • Goitre, FHx thyroid dysfn., prior postpartum thyroiditis, T1DM • Ideally, check TSH preconception: • 2.5-5.0 mU/L: recheck TSH during 1st trimester • 0.4-2.5 mU/L: do not need to recheck during preg • If TSH not done preconception do at earliest prenatal visit: • 0.1-0.4 mU/L: hCG effect (9% preg), recheck in 5wk • < 0.1 mU/L: recheck immediately with FT4, FT3, T4, T3 Thyrotoxicosis & Pregnancy • Causes: • • • • • Graves’ disease TMNG, toxic adenoma Thyroiditis Hydatiform mole Gestational hCG-asscociated Thyrotoxicosis » » » » Hyperemesis gravidarum hCG 60% TSH, 50% FT4 Resolves by 20 wks gestation Only Rx with ATD if persists > 20 wk Thyrotoxicosis & Pregnancy • Risks: • Maternal: stillbirth, preterm labor, preeclampsia, CHF, thyroid storm during labor • Fetal: SGA, possibly congenital malformation (if 1st trimester thyrotoxicosis), fetal tachycardia, hydrops fetalis, neonatal thyrotoxicosis Thyrotoxicosis & Pregnancy • Diagnosis difficult: • hCG effect: » Suppressed TSH (9%) +/- FT4 (14%) until 12 wks » Enhanced if hyperemesis gravidarum: 50-60% with abnormal TSH & FT4, duration to 20 wks • FT4 assays reading falsely low • T4 elevated due to TBG (1.5x normal) • NO RADIOIODINE • Measure: • TSH, FT4, FT3, T4, T3, thyroid antibodies? • Examine: goitre? orbitopathy? pretibial myxedema? Pregnant & Suppressed TSH TSH 0.1 – 0.4 TSH < 0.1 Recheck in 5 wks FT4, FT3, T4, T3 Thyroid Ab’s Examine Still suppressed Normalizes Hyperemesis Gravidarum • Very High TFT’s: • TSH undetectable • very high free/total T4/T3 • hyperthyroid symptoms • no hyperemesis • TSH-R ab + • orbitopathy • goitre, nodule/TMNG • pretibial myxedema Don’t treat with PTU Abnormal TFT’s past 20 wk Treat Hyperthyroidism (PTU) Thyrotoxicosis & Pregnancy: Rx • No RAI ever (destroy fetal thyroid) • PTU • Start 100 mg tid, titrate to lowest possible dose • Monitor qmos on Rx: T4, T3, FT4, FT3 – TSH less useful (lags, hCG suppression) • Aim for high-normal to slightly elevated hormone levels – T4 150-230 nM, T3 3.8-4.6 nM, FT4 26-32 pM • 3rd trimester: titrate PTU down & d/c prior to delivery if TFT’s permit to minimize risk of fetal goitre • Consider fetal U/S wk 28-30 to R/O fetal goitre • If allergy/neutropenia on PTU: 2nd trimester thyroidectomy Thyrotoxicosis & Lactation • ATD generally don’t get into breast milk unless at higher doses: • PTU > 450-600 mg/d • MTZ > 20 mg/d • Generally safe • I prefer PTU > MTZ for preg lactating • Take ATD dose just after breast-feeding • Should provide 3-4h interval before lactates again Neonatal Grave’s • Rare, 1% infants born to Graves’ moms • 2 types: Transplacental trnsfr of TSH-R ab (IgG) • Present at birth, self-limited • Rx PTU, Lugol’s, propanolol, prednisone • Prevention: TSI in mom 2nd trimester, if 5X normal then Rx mom with PTU (crosses placenta to protect fetus) even if mom is euthyroid (can give mom LT4 which won’t cross placenta) Child develops own TSH-R ab • Strong family hx of Grave’s • Present @ 3-6 mos • 20% mortality, persistant brain dysfunction Postpartum & Thyroid • • • • 5% (3-16%) postpartum women (25% T1DM) Up to 1 year postpartum (most 1-4 months) Lymphocytic infiltration (Hashimoto’s) Postpartum Exacerbation of all autoimmune dx • 25-50% persistant hypothyroidism • Small, diffuse, nontender goitre • Transiently thyrotoxic Hypothyroid Postpartum & Thyroid • Distinguish Thyrotoxic phase from Grave’s: • No Eye disease, pretibial myxedema • Less severe thyrotoxic, transient (repeat thyroid fn 2-3 mos) • RAI (if not breast-feeding) • Rx: • Hyperthyroid symptoms: atenolol 25-50 mg od • Hypothyroid symptoms: LT4 50-100 ug/d to start » Adjust LT4 dose for symtoms and normalization TSH » Consider withdrawal at 6-9 months (25-50% persistent hypothyroid, hi-risk recur future preg) Postpartum & Thyroid • Postpartum depression • When studied, no association between postpartum depression/thyroiditis • Overlapping symtoms, R/O thyroid before start antidepressents • Screening for Postpartum Thyroiditis HOW: TSH q3mos from 1 mos to 1 year postpartum? WHO: – – – – Symptoms of thyroid dysfn. Goitre T1DM Postpartum thyroiditis with prior pregnancy • • Hyperparathyroidism Rare in pregnancy Complications in the mother include – – – – – – • • 36% nephrolithiasis, 19% bone disease, 13% pancreatitis, 13% urinary tract infections and pyelonephritis, 10% hypertension (100% in all cases of carcinoma thus far reported), and 8% hypercalcemic crisis. Neonatal hypocalcemia is often the initial clue to the presence of maternal hyperparathyroidism. Reported complications include 27.5% fetal mortality and 19% neonatal tetany. • A persistently elevated serum Ca level and a normal or elevated PTH level, despite hypercalcemia, confirm the diagnosis. • Surgery is the treatment of choice for confirmed hyperparathyroidism. In pregnancy, the optimal time for surgery is the second trimester, when the complication risks (abortion or premature labor) are reduced. When surgery is not possible, maintaining adequate hydration and administering oral phosphates may be temporary measures until surgery can be safely performed. • Hypoparathyroidism • The most common cause of hypocalcemia is hypoparathyroidism that usually follows parathyroid or thyroid surgery. • Chronically hypocalcemic pregnant women may have a fetus with skeletal demineralization. • Treatment usually prevents symptomatic hypocalcemia. • Woman is given 1,25-dihydroxyvitamin D3 (calcitriol), dihydrotachysterol, or large doses of vitamin D (50,000 to 150,000 U/day); calcium gluconate or calcium lactate (3 to 5 g/day); and a diet low in phosphates. • The fetal risks from large doses of vitamin D have not been established. PHEOCHROMOCYTOMA • These are chromaffin tumors that secrete catecholamines. Most are located in the adrenal medulla, but 10 percent are located in the sympathetic ganglia. • Maternal death was much more common if the tumor was not diagnosed antepartum • Maternal mortality decreased from 16 to 4 percent. • There were no maternal deaths when the diagnosis was made antepartum. • There are several methods for tumor localization during pregnancy (Sonography, MRI) Pregnancy and Cushing Syndrome • The most common cause of Cushing syndrome is iatrogenic corticosteroid treatment. • The cause of endogenous Cushing syndrome is increased adrenal cortisol production. Most cases are due to Cushing disease, bilateral adrenal hyperplasia that is, stimulated by corticotropin-producing pituitary adenomas. • Maternal complications include hypertension in 60 to 90 percent and gestational diabetes in about 50 percent. • • Heart failure is common during pregnancy, • Perinatal morbidity and mortality are correspondingly high. • Preterm delivery was reported in 60 percent and perinatal mortality in about 25 percent Adrenal Insufficiency and Pregnancy • Untreated adrenal hypofunction frequently causes infertility, but with replacement therapy, ovulation is restored. • If untreated, common symptoms include weakness, fatigue, nausea and vomiting, and weight loss • With treatment, the pregnant woman is observed for evidence of either inadequate or excessive steroid replacement. • During labor, delivery,and postpartum, or after a surgical procedure, steroid replacement must be increased appreciably to approximate the normal adrenal response so-called stress doses. • Hydrocortisone, 100 mg, is usually given intravenously every 8 hours. • Pregnancy and Hyperaldosteronism. Progesterone blocks aldosterone action, thus, there are very high levels of aldosterone in normal pregnancy • Therefore is not surprising that there may be amelioration of symptoms and electrolyte abnormalities during pregnancy SHEEHAN SYNDROME • Pituitary ischemia and necrosis associated with obstetrical blood loss may cause hypopituitarism. • When it occurs acutely, affected women may have persistent hypotension, tachycardia, hypoglycemia, and failure of lactation. • Subsequent deficiencies of some or all pituitary responsive hormones may develop.