Pregnancy and Endocrinology
advertisement

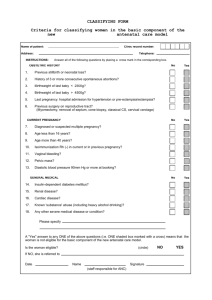
Pregnancy & Endocrinology William Harper Hamilton General Hospital McMaster University www.drharper.ca Objectives Thyroid Disorders & Pregnancy Normal thyroid phsyiology & pregnancy Hypothyroidism & pregnancy Thyrotoxicosis & pregnancy Postpartum thyroid dysfunction Diabetes & Pregnancy Gestational DM Type 1 & Type 2 DM & Pregnancy Case 1 31 year old female Somalia Canada 3 years ago G2P1A0, 11 weeks pregnant Well except fatigue Hb 108, ferritin 7 (Fe and LT4 interaction?) TSH 0.2 mU/L, FT4 7 pM Started on LT4 0.05 TSH < 0.01 mU/L FT4 12 pM, FT3 2.1 pM Case 1 1. 2. How would you characterize her hypothyroidism? What are the ramifications of pregnancy to thyroid function/dysfunction? TSH Low High FT4 & FT3 FT4 Low Low High 1° Hypothyroid 2° thyrotoxicosis Central 1° Thyrotoxicosis Hypothyroid If equivocal TRH Stim. •Endo consult •FT3, rT3 •MRI, α-SU High MRI, etc. RAIU Case 1 GH, IGF-1 normal LH, FSH, E2, progesterone, PRL normal for pregnancy 8 AM cortisol 345, short ACTH test normal MRI: normal pituitary TGAB, TPOAB negative Normal pregnancy, delivery, baby, lactation Thyroid & Pregnancy: Normal Physiology Increased estrogen increased TBG (peaks wk 15-20) Higher total T4 & T3: normal FT4 & FT3 if normal thyroid fn. and good assay many automated FT4 assays underestimate true FT4 level (except Nichols equilibrium dialysis free T4 assay) if suspect your local FT4 assay is underestimating FT4 can check total T4 & T3 instead (normal pregnant range ~ 1.5x nonpregnant) hCG peak end of 1st trimester, hCG has weak TSH agonist effect so may cause: slight goitre mild TSH suppression (0.1-0.4 mU/L) in 9% of preg mild FT4 rise in 14% of preg Thyroid & Pregnancy: Normal Physiology Fetal thyroid starts working at 12-14 wks T4 & T3 cross placenta but do so minimally Cross placenta well: ATD (PTU & MTZ): MTZ > PTU TSH-R Ab (stim or block) Fetal goitre (can compress trachea after birth) MTZ aplasia cutis scalp defects Other MTZ reported embryopathy: choanal atresia, esophageal atresia, tracheo-esophageal fistula Therefore do NOT use MTZ during pregnancy, use PTU instead No TSH & FTI at end of 1st trimester as expected from hCG effect Requirement to increase LT4 dose occurred between weeks 4 -20 Despite exponential rise in estradiol throughout pregnancy (note y-axis units) TBG levels plateau at 20 wks • LT4 dose requirement tied to rising TBG levels (THBI inversely proportional to TBG level) • By 10 wks need average increase of 29% LT4 dose • By 20 wks need average increase of 48% LT4 dose • No increase of dose beyond 20 wks required * Regardless of cause of hypothyroidism (Hashimoto’s, thyroidectomy) initial LT4 dose increase is usually required early (~ week 8), before 1st prenatal visit! Thyroid & Pregnancy: Hypothyroidism 85% will need increase in LT4 dose during pregnancy due to increased TBG levels (ave dose increase 48%) Risks: increased spont abort, HTN/preeclampsia, abruption, anemia, postpartum hemorrhage, preterm labour, baby SGA Fetal neuropsychological development (NEJM, 341(8):549-555, Aug 31, 2001): – Cognitive testing of children age 7-9 – Untreated hyothyroid mothers vs. normal mothers: • Average of 7 IQ points less in children • Increased risk of IQ < 85 (19% vs. 5%) – Retrospective study, data-dredging? LT4 dose adjustment in Pregnancy: - Optimize TSH preconception (0.4 – 2.5 mU/L) - TSH at pregnancy diagnosis (~3-4 wk gestation), q1mos during 1st 20 wks and after any LT4 dose change, q2mos 20 wks to term - Instruct women to take 2 extra thyroid pills/wk (q Mon, Thurs) for 29% dose increase once pregnancy suspected (+ commercial preg test) - If starting LT4 during preg: initial dose 2 ug/kg/d and recheck TSH q4wk until euthythyroid TSH Dose Adjustment TSH increased but < 10 Increase dose by 50 ug/d TSH 10-20 TSH > 20 Increase dose by 50-75 ug/d Increase dose by 100 ug/d Pregnancy: screen for thyroid dysfn ? Universal screening not currently recommended: Definitely screen: Goitre, FHx thyroid dysfn., prior postpartum thyroiditis, T1DM Ideally, check TSH preconception: ACOG, AACE, Endo Society, ATA Controversial! 2.5-5.0 mU/L: recheck TSH during 1st trimester 0.4-2.5 mU/L: do not need to recheck during preg If TSH not done preconception do at earliest prenatal visit: 0.1-0.4 mU/L: hCG effect (9% preg), recheck in 5wk < 0.1 mU/L: recheck immediately with FT4, FT3, T4, T3 Thyrotoxicosis & Pregnancy Causes: Graves’ disease TMNG, toxic adenoma Thyroiditis Hydatiform mole Gestational hCG-asscociated Thyrotoxicosis • • • • Hyperemesis gravidarum hCG 60% TSH, 50% FT4 Resolves by 20 wks gestation Only Rx with ATD if persists > 20 wk Thyrotoxicosis & Pregnancy Risks: Maternal: stillbirth, preterm labor, preeclampsia, CHF, thyroid storm during labor Fetal: SGA, possibly congenital malformation (if 1st trimester thyrotoxicosis), fetal tachycardia, hydrops fetalis, neonatal thyrotoxicosis Thyrotoxicosis & Pregnancy Diagnosis difficult: hCG effect: • Suppressed TSH (9%) +/- FT4 (14%) until 12 wks • Enhanced if hyperemesis gravidarum: 50-60% with abnormal TSH & FT4, duration to 20 wks FT4 assays reading falsely low T4 elevated due to TBG (1.5x normal) NO RADIOIODINE Measure: TSH, FT4, FT3, T4, T3, thyroid antibodies? Examine: goitre? orbitopathy? pretibial myxedema? Pregnant & Suppressed TSH TSH 0.1 – 0.4 TSH < 0.1 Recheck in 5 wks FT4, FT3, T4, T3 Thyroid Ab’s Examine Still suppressed Normalizes Hyperemesis Gravidarum • Very High TFT’s: • TSH undetectable • very high free/total T4/T3 • hyperthyroid symptoms • no hyperemesis • TSH-R ab + • orbitopathy • goitre, nodule/TMNG • pretibial myxedema Don’t treat with PTU Abnormal TFT’s past 20 wk Treat Hyperthyroidism (PTU) Thyrotoxicosis & Pregnancy: Rx No RAI ever (destroy fetal thyroid) PTU Start 100 mg tid, titrate to lowest possible dose Monitor qmos on Rx: T4, T3, FT4, FT3 – TSH less useful (lags, hCG suppression) Aim for high-normal to slightly elevated hormone levels – T4 150-230 nM, T3 3.8-4.6 nM, FT4 26-32 pM 3rd trimester: titrate PTU down & d/c prior to delivery if TFT’s permit to minimize risk of fetal goitre Consider fetal U/S wk 28-30 to R/O fetal goitre If allergy/neutropenia on PTU: 2nd trimester thyroidectomy Thyrotoxicosis & Lactation ATD generally don’t get into breast milk unless at higher doses: PTU > 450-600 mg/d MTZ > 20 mg/d Generally safe I prefer PTU > MTZ for preg lactating Take ATD dose just after breast-feeding Should provide 3-4h interval before lactates again Neonatal Grave’s Rare, 1% infants born to Graves’ moms 2 types: Transplacental trnsfr of TSH-R ab (IgG) Present at birth, self-limited Rx PTU, Lugol’s, propanolol, prednisone Prevention: TSI in mom 2nd trimester, if 5X normal then Rx mom with PTU (crosses placenta to protect fetus) even if mom is euthyroid (can give mom LT4 which won’t cross placenta) Child develops own TSH-R ab Strong family hx of Grave’s Present @ 3-6 mos 20% mortality, persistant brain dysfunction Postpartum & Thyroid 5% (3-16%) postpartum women (25% T1DM) Up to 1 year postpartum (most 1-4 months) Lymphocytic infiltration (Hashimoto’s) Postpartum Exacerbation of all autoimmune dx 25-50% persistant hypothyroidism Small, diffuse, nontender goitre Transiently thyrotoxic Hypothyroid Postpartum & Thyroid Distinguish Thyrotoxic phase from Grave’s: No Eye disease, pretibial myxedema Less severe thyrotoxic, transient (repeat thyroid fn 2-3 mos) RAI (if not breast-feeding) Rx: Hyperthyroid symptoms: atenolol 25-50 mg od Hypothyroid symptoms: LT4 50-100 ug/d to start • Adjust LT4 dose for symtoms and normalization TSH • Consider withdrawal at 6-9 months (25-50% persistent hypothyroid, hi-risk recur future preg) Postpartum & Thyroid Postpartum depression When studied, no association between postpartum depression/thyroiditis Overlapping symtoms, R/O thyroid before start antidepressents Screening for Postpartum Thyroiditis HOW: TSH q3mos from 1 mos to 1 year postpartum? WHO: – – – – Symptoms of thyroid dysfn. Goitre T1DM Postpartum thyroiditis with prior pregnancy Objectives Thyroid Disorders & Pregnancy Normal thyroid phsyiology & pregnancy Hypothyroidism & pregnancy Thyrotoxicosis & pregnancy Postpartum thyroid dysfunction Diabetes & Pregnancy Gestational DM Type 1 & Type 2 DM & Pregnancy Gestational Diabetes Mellitus (GDM) “Glucose intolerance with onset/discovery during pregnancy” Some T2DM picked up during pregnancy Rarely some T1DM may present during pregnancy Prevalence higher than previously thought in Canada: 3.5 - 3.8% non-Aboriginal (but multi-ethnic) population 8.0 - 18.0% Aboriginal Gestational Diabetes Mellitus (GDM) Prior “selective screening” resulted in missed cases: Caucassians < 25 y.o. No personal or FHx of DM No prior infant with birth weight > 4 kg Treatment of GDM reduces perinatal morbidity Diagnosis GDM maternal anxiety ? Evidence controversial for this Therefore all women should be screened * Presence of multiple risk factors warrants earlier screening (preconception, 1st & 2nd trimester) GDM: Morbidity Maternal Fetal/Neonatal Macrosomia (birth trauma,cesarian) Macrosomia (shoulder dystocia) Preeclampsia RDS Polyhydramnios Neonatal hypoglycemia Perinatal mortality (fetus) Neonatal hypocalcemia Postpartum IFG, IGT, DM 3-6 mos: 16-20 % Lifetime: 30-50 % Neonatal jaundice Obesity later in life? IGT, IFG, or DM later in life? GDM Treatment CBG qid: FBS, 1-2h pc Dietary: 3 small meals, 3 small snacks If glycemic targets not met: Insulin Multiple Daily Injection (MDI) best Insulins: regular, lispro, aspart ? (still new) No glargine (stimulates IGF-I receptors) GDM Treatment No OHA’s, not standard of care yet. Glyburide Minimal crossing of placenta, 3rd trimester most organogenesis complete 1 RCT: 404 women, mild GDM, glyburide vs. insulin, no difference in outcomes Further study before safety established Metformin Retrospective cohort: • preeclampsia & stillbirth • Bias: DM women older, more obese GDM: Labour & Postpartum NPO during Labour: Monitor CBG q1h, target BS 4 – 6.5 mM Hypoglycemia (BS < 4 mM): IV D5W Hyperglycemia (BS > 6.5 mM): IV D5W & IV insulin gtt Postpartum: D/C all insulin (IV and SC) CBG in recovery: • > 10 mM CBG qid, may need Rx for T2DM • < 10 mM stop CBG monitoring FBS or 2hPG in 75g OGTT within 6 mos postpartum and prior to any future planned pregnancies Encourage: breast feeding, healthy diet, exercise to prevent future Type 2 DM, GDM Screen for future T2DM (GDM is a risk factor) T1DM, T2DM & Pregnancy Congenital anomalies: 2-3x increased risk Cardiac malformations Neural Tube Defects 1 % risk Folate 1-4 mg/d (Prenatal vitamin 0.4-1.0 mg) d/c ACE-I and ARBs methyldopa, etc. Dilated eye exam: preconception & 1st trimester T2DM: d/c OHA insulin Good glycemic control prior to conception: Prevent unplanned pregnancies: OCP or 2x barrier Initiate MDI and qid (FBS, 2hPC) prior to preg CSII also another option T1DM, T2DM & Pregnancy < 8.0 ? T1DM & T2DM: Labour & Postpartum NPO during Labor: Monitor CBG q1h, target BS 4.0 – 6.5 mM IV D5W & IV insulin gtt (Hamilton Health Sciences Protocol) Postpartum: D/C all IV insulin Insulin resistance/requirements rapidly fall during & after labor T2DM: monitor CBG qid • Restart insulin if CBG > 10 mM T1DM: postpartum honeymoon • CBG q1h x 4h, then q2h x 4h, then q4h • Restart MDI insulin S.C. when CBG > 10 mM No OHA, ACE-I or ARB during breast feeding! END