Pain - University of Alabama at Birmingham
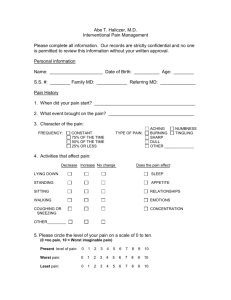
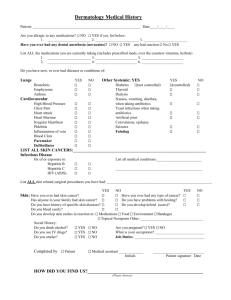
advertisement

Elizabeth Kvale, MD Assistant Professor of Medicine University of Alabama at Birmingham Unpleasant sensory and emotional experience associated with actual or potential tissue damage. Physical pathology does not need to be present Pain is one of the most common reasons Americans 18+ seek medical attentions. 25-50% community-dwelling older adult have pain 45-80% nursing home residents have pain Sensory-Discriminative Pain Perception Affective-Motivational Noxious Stimulus Autonomic & Motor Responses Commons Myths Regarding Pain In the presence of tissue damage there must be pain, and vice versa. It is useful to classify pain as either organic (biological) or functional (psychogenic) A placebo response verifies that pain is psychological in origin BIOPSYCHOSOCIAL MODEL OF PAIN (and symptoms) BIOMEDICAL - Pathology - Injury - Nociception SOCIOCULTURAL - Age, Sex, Race - Income, Education - Social Milieau PSYCHOLOGICAL - Anxiety, Depression - Cognitive Factors - Behavioral Factors Pain Behavior Suffering Pain Nociception Acute pain ◦ identified event, resolves days–weeks ◦ usually nociceptive Chronic pain ◦ cause often not easily identified, multifactorial ◦ indeterminate duration ◦ nociceptive and / or neuropathic Nociceptive – Arthritis, fracture, laceration Visceral – Pancreatitis, M.I., Constipation Neuropathic – Herpes zoster, diabetic neuropathy, Complex Regional Pain Syndromes – RSD Central Pain Pain is a subjective experience – the patient is the best source of information about their pain Pain History – site(s), intensity, temporality, character, exacerbating and alleviating factors Comprehensive and ongoing assessment. Medical history Physical exam Psychosocial Family and culture Pain history (including previous treatment) Comprehensive medication history The nature and intensity of the pain. Current and past treatments for the pain. Underlying or coexisting diseases or conditions. The effect of the pain on the physical and psychological function. Documentation of a history of substance abuse. Documentation of one or more recognized medical indications for the use of a controlled substance. American Academy of Pain Medicine, Long-term Controlled Substances Therapy for Chronic Pain, July 2004 The use of an instrument to assess pain allows you to know and document whether you have helped the patient Grimace, Groan, Rub, Guard, Brace Can be observed and quantified Don’t delay for investigations or disease treatment Unmanaged pain nervous system changes › permanent damage amplify pain Treat underlying cause (eg, radiation for a neoplasm) 74 yo with multiple medical issues, many of which contribute to pain Multiple medications Declining functional ability Recent Falls Lives alone, but with supportive family near Routine assessment and documentation Patient and family education Non-pharmacologic strategies Serial Trial Intervention Documentation Heat Cold Positioning Distraction Relaxation Massage Controlled breathing and guided imagery Music Regular use of acetaminophen Consider nonsteroidal anti-inflammatory › For intermittent pain › Many medical contraindications Consider low dose pain medications › Oxycodone, morphine, hydromorphone › ? Use of combination medications Re-evaluate Match the medication to the amount of discomfort the patient is having severe WHO 3-step Ladder 3 2 moderate A/Codeine 1 mild A/Hydrocodone A/Oxycodone ASA Acetaminophen NSAIDs ± Adjuvants A/Dihydrocodeine Tramadol ± Adjuvants Morphine Hydromorphone Methadone Levorphanol Fentanyl Oxycodone ± Adjuvants A structured approach to “let’s try it and see what happens” Patients and caregivers are essential team members in evaluating and managing pain Caregiver resistance to pain management strategies ensures failure Explore areas of concern or resistance to tailor education efforts most effectively Use a standard scale to track the course of pain Identify objectives that will be used to determine treatment success including but not limited to pain relief, improved physical function, and improved psychological function. Documentation of the need for further diagnostic evaluations or other treatments which may be planned. Adjustment of drug therapy based on the individual medical needs of each patient. Consideration of other treatment modalities or rehabilitation programs depending on the extent and etiology of the pain. Encourage activity and self-care Employ physical modalities: heat, cold, massage, acupuncture, transcutaneous electrical nerve stimulation Recommend cognitive-behavioral interventions: relaxation and imagery, psychotherapy, structured support Educate the patient The risk of under treating pain is a greater concern than the risk of worsening delirium with medications None systemic therapies, intraarticular steroid injections, lidocaine patches, topical preparations Opioids are first-line therapy for severe acute pain and chronic moderate to severe persistent pain due to cancer, AIDS, and other advanced illnesses. Consider the individual’s risk of drug abuse and addiction and provide appropriate and structured therapy. Opioids are metabolized by the liver and excreted by the kidney Peak plasma concentration is reached: 60-90 minutes after oral dosing 30 minutes after SC or IM dosing 6 minutes after IV injection Effective half-lives of 3–4 hours with normal renal clearance Steady state achieved in 24 hours Extended-release forms release over 8, 12, or 24 hours; fentanyl patch provides continuous relief for 48–72 hours Use short-acting opioids to determine opioid requirements over 24 hours If pain remains uncontrolled, increase doses by 25% to 50% for mild to moderate pain and by 50% to 100% for severe pain Provide “rescue” analgesia for breakthrough pain or acute pain flares 5% to 15% of the 24-hr dose Offer every 1 hr orally; 30 min SC/IM; 10 min IV Urine drug screening (UDS) is recommended on initiation of therapy and randomly at subsequent visits Implement as a global policy rather than a targeted policy Evaluate for aberrant drug use and adherence to therapy you are providing Interpretation of UDS results can be challenging Provides a report of all schedule 2 prescriptions filled by patient in state of Alabama Results of report can be shared with patient, but you cannot give a copy of the report to the patient Reports should not be placed in the medical record http://pdmp.alabama.gov/index.html Reduce pain severity Improved and or restore function Improve mood and sleep patterns Reduce misuse or overuse of medication Return to productive activity Increase ability to manage pain Effective treatment should be as costeffective as possible