BirthProcess
advertisement

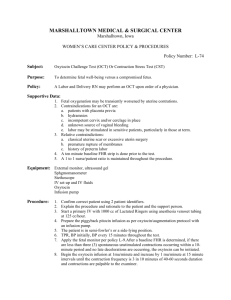
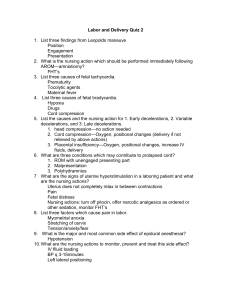
Module C- Birth Process Labor – What causes It ? • The exact cause is unknown- Theories • 1. Hormonal Influence – Progesterone/ Estrogen, Oxytocin • 2. Uterine Stretch Theory • 3. Fetal Endocrine Control Theory • 4. Prostaglandin Theory The Fetus as the Passenger • The passage of fetus via birth canal is influenced by • 1. Size of head, shoulders & hips • 2.Presentation • 3.Position Fetus as the passenger • Head – because of its size, rigidity & characteristics, it is of major obstetrical interest • Cranial Bones: Frontal, Parietal, Occipital,Temporal etc • Bones are united by membranous sutures :Sagittal, Frontal, Coronal, Lamboid • These sutures intersect to form Fontanels: Anterior and Posterior Fontanels • Sutures intersect to form fontanels • Anterior – found @ intersection of 2 parietal & frontal bone • Diamond shape • Larger of two • Closes at 18 months Posterior Fontanelle • @ the junction of 2 parietal & occipital bones • Triangle in shape • Smaller of the two • Closes from birth to 12 weeks • * Dehydration vs Intercranial pressure* Measurements of Interest! • *Transverse Diameter of fetal head – Biparietal= 9.25cm • Maternal Pelvic Measurements: • Diagonal Conjungate DC > 11.5 – Actual diameter of inlet. Sacral promontory & lower margin of symphysis pubis • True conjugate or conjugate vera (CV)- Estimate DC 1.5-2 cm. Smallest diameter of inlet. Distance between posterior aspect of symphysis pubis & sacral promontory • Tuberischii (Biischial) Diameter >8 OK. Actual transverse diameter of outlet. Taken from ischial tuberosities. Molding ? • What molds? Due to the fact that the cranial bones are not united, but are separated by sutures & fontanells, this aids in the ability to overlap & MOLD to fit the pelvis Presentation • -Is that part of the fetus that first enters the pelvis and lies over the inlet • -It may be head, face, breech or shoulder • Presenting Part is that part of the fetus that lies closest to the internal os of the cervix Presentation • Three main presentations are Cephalic, Breech, and Shoulder • Cephalic ---------Occiput – O – Vertex 96% • Chin/Mentum- M- Face • Breech ---------- Sacrum- S - Breech 3% • Shoulder -------Scapula- Transverse Lie = C/S 1% Terms: • Attitude – Relationship of fetal body parts to each other – Flexion vs Extension • Position- the relationship or point of direction on the PP to one of the 4 quadrants of the mothers pelvis: ? LOA, ROA, LOP, ROP, RSA, RSP, etc? • Lie- The relationship of long axis of fetus to long axis of mother- 2 choices: Longitudinal Lie vs Transverse Lie Factors that Facilitate the Labor Process • • • • • Presenting Part Attitude Presentation Position Lie Assessing / Evaluating the progress of Labor • Ischial Spines • STATION • Engagement or Engaged • *Previous measurements Station : Ischial spines & Fetus Biparietal • Head above • Spines • • Head @ IS • Head below • Ischial Sp • -3 -2 -1cm 0 Station +1 +2 +3 cm Labor • Refers to the series of processes by which the products of conception are expelled by the mother Premonitory Signs of Labor • Show- Mucus + Blood = Show. The pressure on cervix causes small capillaries to rupture • Lightening – S/S, Who has it and when? • ROM- What MUST I assess and why Are our patients really in Labor? • • • • • • • • • • Gravida Para Length of previous labor ? Lightening Show- Amount, Color, Odor ROM- (AROM, SROM , PROM), FHR, TIME, Color, Odor, Gush Contractions-Frequency, Duration, Intensity, Felt where? Dilatation Effacement Station Has the patient’s water broken?? • The fluid can be viewed microscopically – Look for Ferning • You can use litmus paper to see pH changes. Amniotic fluid is alkaline • Blue means Baby True verses False Labor • ContractionsRegular,Frequency, Duration, Quality all increase in time & duration • Activity – Increase discomfort • Felt where? • GI- Upset • BOW – May rupture • Show – None to some • Changes In Cervix - Yes • • Irregular, short duration • Relieved by walking • • • • • Only in abdomen No GI upset Intact No show * Except* No cervical change Uterine contractions • Braxton Hicks • Pain vs Contractions • 3 methods of assessing Contractions • Each contractions has 3 phases – Increment, Acme (Peak), decrement • Duration 45-90 sec. • Primary powers/forces • Frequency – Varies • 50-60 mm Hg of pressure (IUPC) • External – Mild +1, Moderate +2, Strong +3 Cervical assessment during the labor process • Effacement of Cervixmeans the shortening & thinning of the cervical canal. • Expressed in terms or % • The 2-3cm in length and 1 cm thick Cx will be taken up into the lower uterine segment • Primigravida- 80-100% • Multigravida – 50-80% on admission Effacement • • • • • • • Expressed in terms or % Less than 50% = Thick Cervix 60% = Fairly thick 70-80% = Fairly thin 80-90% = Thin 90-99% = Paper Thin 100% = Completely Effaced Dilatation of the Cervix • The enlargement of the cervical os from a few mm in size to a size large enough for fetus to pass. When the cx can not be felt = 10 cm. (FT-10) • Involuntary • Caused by 1. Drawing up of musculofascial components of cx with contractions (good ones) 2. Pressure on ex by BOW & PP • Should I ever NOT do an exam? • Do students do vaginal exams? Duration of Labor – How long is too long?? • The length depends on many factors: • 1. Size of baby • 2.Size of pelvis • 3.Presentation • 4.Position • 5.Anesthesis & medications • 6.Relaxation ability • 7.Gravida & Para • *Average – 13-14 Primigravida and 8 hours in Multigravida Four Stages of Labor • 1st Stage- Dilating Phase • 2nd StageDescent/Expulsion Phase • 3rd Stage- Placental Phase • 4th Stage – Recovery Phase FIRST STAGE OF LABOR • 1st TRUE LABOR CONTRACTION TO COMPLETE DILATION OF CERVIX • LATENT – FT- 4 cm • ACTIVE – 5- 10 cm • WHAT IS TRANSITION?!!!!!! SECOND STAGE OF LABOR • CERVIX 10 CMDELIVERY OF BABY • ARE DRUGS GIVEN NOW? • ANESTHESIA • LENGTH – FEW MINUTES – HOURS • WHAT AFFECTS THE LENGTH HERE? • WHAT DO THE NURSES DO DURING THIS STAGE? 3RD STAGE OF LABOR • Placental Phase • From the delivery of baby to the delivery of placenta • Signs that placenta has separated • Length – minutes usually • What drugs are given here? • What are the nurses responsibilities during this phase? • Family interaction 4th STAGE OF LABOR • Recovery Phase • From delivery of placenta to the first few hours postpartum • What drugs are given here? • What are the nursing responsibilities? Assess fundus, lochia, vital signs • Possible complications: Hemorrhage, urinary retention, hypotension, s/e from anesthesia/drugs Maternal Adaptation to Labor • Cardiovascular Volume • Blood Pressure • Respiratory changes • WBC’s INDUCTION OF LABOR Induction – Artificially bringing on of Labor after a period of viability • • • • • • Criteria Methods of induction Special nursing interventions Complications Contraindications Uses for Oxytocin Criteria for doing an Induction • • • • • • • PROM PIH Hemolytic Disease Post maturity Diabetes Convenience Other • Indications: – – – – – – – – – PIH SROM at or near term without onset of labor Chorioanmionitis Maternal medical conditions that worsen with continuation of pregnancy Conditions in which the intrauterine environment is hostile to fetal well-being Abruptio placenta Fetal death History of rapid labors Living a long distance from the hospital Methods of Inductions • Long ago- Castor oil and SS enema • Rupture BOW • Oxytocin by IV administration • Advantages vs Disadvantages • Complications Mechanical Methods • Placing moisture absorbing inserts into the cervix. – Dilapan – synthetic material – Lamicel – synthetic sponge containing MgSO4 – Laminaria tents – sterile, cone-shaped preparations of dried seaweed Special Nursing Interventions With Inductions • Observe contractions – No closer than q 2 min. and no longer than 90 seconds. If so Stop Pitocin! (Or decrease rate) • If any sign of fetal distress – Stop Pitocin, Turn patient and start O2 Complications • • • • • 1. Uterine tetany – 2. Fetal hypoxia 3. Ruptured uterus – 4. Fetal Anoxia 5. Maternal hemorrhage • Contraindications: – – – – – Complete placenta previa Abnormal presentations Fetal part above the pelvic inlet Active genital herpes infection Previous surgery in the upper uterus • Classical C/S – One or more low-transverse C/S with caution – Over-distended uterus – Severe maternal conditions (heart disease or severe hypertension) – Non-reassuring FHR pattern Contraindicated uses • 1. Normal labor • 2. CPD • 3. Overdistended uterus • 4.Fetal distress- What types would you see? • 5. Multiparity – Greater than 4 Cervical Ripening METHODS • Prostaglandins - E2 (PGE2) – Prepidil Gel – 0.5 mg intracervically Repeat up to three times in 24 hours at 6 hr. intervals. May begin Oxytocin 6 hr after last dose. – Cervidil vaginal insert – 10 mg in a time released vaginal insert. Rate of release is 0.3 mg/hr. Remove at onset of active labor or 12 hr. after administration. May begin Oxytocin 30 min. after last dose. Induction Protocol • Patient in lateral position • Continuous monitoring of FHR and contractions. • Record VS, FHR and UC for 15-20 minutes before Oxytocin started. • Maternal VS q 15min while increasing dose and q30 min once dose is stable. • Temperature q4h unless membranes ruptured. • Main IV fluids of LR at 125 cc/hr. • Mix Pitocin 10 Units in 1000cc D5W • Piggyback on IV pump at closest port to insertion site. • Start at 2 mUnits/min and increase by 2mUnits q15 minutes until adequate labor pattern is established. • IV infusion rate should be maintained so that contractions: – Do not exceed a frequency of 5 in a 10 minute period – Montevideo units are 150-250 Montevideo Units Average Intensity of contraction X Number of contractions in 10 minutes Montevideo Units Example: 50 mmHg pressure X 4 contractions 200 MVU • Signs of Hypertonic Uterine Activity: – Cont. duration > 90 seconds – Cont. less than 2 min apart or less than 60 seconds between contraction. – Uterine Resting tone > 20 mm Hg pressure with IUPC – Peak pressure > 90 mm Hg pressure with IUPC – MVU > 250 – FHR with late decelerations WHAT TO DO! • Nursing Care: – Reduce or stop the oxytocin infusion – Increase the rate of the primary nonadditive infusion – Keep the laboring woman in a lateral position – Give oxygen by face mask at 8-10 L/min – Notify the physician Uses for Oxytocin • • • • • • • Induction Stimulation Stress test (OCT) Milk letdown * Dosage * Rate *Bishop score 2 types of Uterine Dysfunction • Hypotonic • Tone less than 50mm causing poor contractions and little cervical change • Tx: Rupture BOW / Oxytocin Adm. • Causes: CPD, Malposition, uterine atony from long labor • Complications: Exhaustion, dehydration, Intrapartal infection • Hypertonic • Tone greater than 50mm * Uterus in state of tetany, both upper & lower contr. • Tx: Stop Pitocin, Tocolytics ie Brethine, Ritodrine, MgSO4 • Causes: Pitocin overstimulation, spontaneous labor • Complications: Uterine rupture, Fetal hypoxia, excessive pain NORMAL LABOR • SLOW • LATENT • • FAST SLOW ACTIVE NEAR COMPLETE DELIVERY • FORCES > • PASSANGER < • PASSANGER PASSAGE Operative Obstetrics • Lacerations -1st,2nd, 3rd Degree • Episiotomy – Midline*, Mediolateral (rarely done) • Forceps (Low forceps / outlet )/ Vacuum extraction • C- Section Episiotomy- Incision of perineum to facilitate delivery • Midline- Advantage- Easier to repair, less uncomfortable. Disadvantage.- Greater chance of tearing into the rectum • Mediolateral – Adv. Less chance of tear, Disadv. – Harder to repair & > pain • Reasons to do an Episiotomy• 1.Easier to repair than tear/laceration • 2.Direction can be controlled • 3.Less pounding of fetus/Overstretching less • 4.Shortens 2nd stage of Labor • What is ironing the perineum?? Indications for C/S • • • • • • • • • CPD Previous C/Section ? PIH Abruptio Placenta / Placenta Previa Fetal distress Diabetes Herpes simplex II Infertility Others Types of C/S • 1. Lower segment section • 2. Classical • 3. Caesarian Hysterectomy • *Preparing for C/S • *Post- op care & special considerations VBAC • Criteria • Common complications • What are the risks? C/S- Why? • Variation in Pelvis • 1.CPD – Treatment • 2.Oversize baby – Complications and common causes • 3.Shoulder Dystocia – What’s done here? • 4. Hydrocephalus Fetal Monitoring Clinical Prep : Fetal Monitoring • Random Auscultation vs Continuous Fetal Monitoring • Which patients do we monitor? • EFM (Electronic Fetal Monitoring) is a useful tool in evaluating fetal response to labor. • Fetal O2 supply must be maintained during labor Fetal Response to the Intrapartum Period • Fetal O2 supply can be reduced by: • 1. Decreased blood flow thru maternal vessels as a result of maternal hyper/hypotension • 2.Maternal hemorrhage or anemia • 3. Fetal circulation: Cord occulsion, placenta separation, Old placenta • 4. Fetal condition: IUGR • 5. Contractions too close or too long Monitoring Options • External – Tocotransducer & ultrasound • Combination – Toco & Fetal Spiral Electrode (FSE)* • Internal – FSE & IUPC (Internal uterine pressure catheter)* • *Membranes must be ruptured, best in detecting ST variability Terms you need to know! • Baseline FHR- FHR between contractions & periodic changes • Tachycardia- Baseline above 160 BPM • Bradycardia- FHR below 110 BPM • Variability – Fluctuation, Beat to beat changes. Normal irregularity of cardiac rhythm. STV/LTV • Examples of periodic changes: • Accelerationsacceleration with FM is a reassuring pattern • Decelerations • 1. Early • 2. Late • 3. Variables • FHT – 120-160 – Could be as low as 110 and still be normal. – Bradycardia - <100 BPM – Tachycardia – >180 BPM • Variability: – Short-term variability (beat-to-beat) – 5-10 BPM. Only accurate on a FSE. – Long-term variability (reactivity) – periodic accelerations that are >15 BPM lasting >15 seconds in duration Decelerations DECELERATIONS • Look at three things • 1.Shape of the decelerations- Uniform vs variable shape • 2. Time relationship to contractions- Does the deceleration occur with the C, after the C or does it VARY? • 3. Range of decelerations – Does the deceleration go down to 60 / 100 / or 120 etc Early Decelerations • Occur with contractions and are usually caused by head compression. – Start with the contraction (early) Mirror image – Peak with the contraction – Return to baseline as contraction goes away – – Usual range is 100-140 – Has uniform shape Nursing Interventions for early Decelerations • NONE • Usually benign • No Treatment except to continue to assess and monitor Variable Decelerations • Occur with or without contractions and are caused by cord compression. – Look like a U, V or W (variable shape) – Rapid onset with rapid return to baseline. – May drop below 100 BPM. Vary in rate ie 60-100 – Can progress to terminal bradycardia. Nursing Interventions for Variable Decelerations • Change maternal position-- R-L, L-R • Change it again if not better (Knee chest if severe) • Amnioinfusion • Administer O2 (Makes nurses feel better) Late Decelerations • Occur as a result of utero-placental insufficiency (decreased tissue perfusion to the fetus). – Start at the peak of the contraction. (Late) – Lowest point at the end of the contraction. Rarely goes below 110 – Slow return to baseline after end of contraction. – May also see a loss of variability. – Could be associated with maternal hypotension as a result of regional anesthesia. Causes for Late Declerations • • • • • • • • Occurs with 1. Maternal supine hypotension 2. Excessive Oxytocin 3.PIH 4.Post mature syndrome 5.Amnionitis/SGA 6. Anesthesia 7.Cardiac disease Nursing Interventions for Lates • Turn patient if cause is supine hypotension • Start O2 • Decrease uterine activity (Stop pitocin, administer Brethine) • Correct Hypotension • Lates should not occur longer than 30 minutes without seeing improvement Fetal Monitoring & Decelerations • Decelerations – Which ones are OK & which ones are not? • Is it good to be Early for work? OK • Is it OK to be Late for work? NO • What if I do both? Then it may or my not be OK. Variable Complications of the Intrapartum Period • RUPTURED UTERUS Who is at Risk? • Previous C/S – Classical vs. low segment • Induction – Pitocin, Cervadil or Cytotec • Long, strong labor • High Parity – Thin uterine wall • Blunt abdominal trauma TYPES OF UTERINE RUPTURE • COMPLETE – a direct break between the uterus and peritoneal cavity. • INCOMPLETE – rupture into the covering of the uterus or into broad ligaments but not into the peritoneal cavity. • DEHISCENCE – partial separation of an old uterine scar. Little or no bleeding may occur. Signs and Symptoms • • • • • • Sudden severe abdominal pain / tenderness Absent FHT No palpable contractions felt Vaginal bleeding Abdominal distension and rigidity Shock – – – – – Hypotension Elevated pulse rate Elevated respiratory rate Pale, clammy skin anxiety Management • Stabilize the Mom and Fetus if possible – Increase IV fluids – O2 administration – T & C, and administer blood (O-) • Emergency C/S • Hysterectomy if complete rupture • Antibiotics INVERSION OF THE UTERUS • Cause: – Pulling on umbilical cord prior to release from uterine wall – Pressure on uterine fundus while relaxed – Abnormally adherent placenta – Congenital weakness of the uterine wall – Fundal placental implantation • Signs and Symptoms: – Fundus cannot be felt or is depressed – Interior of uterus may be seen thru cervix or protruding out of the vagina – Massive vaginal bleeding – Shock • • • • Hypotension Decreased PR and RR Pale, clammy skin Restlessness – Severe pelvic pain Treatment: Dr. will attempt to replace the uterus through the vagina to a normal position, or Laparotomy replacement is attempted Hysterectomy may be required. Two IV lines with large bore needles Fluids and blood replacement Oxytocin to control blood loss after repositioning. Observe for shock and treat accordingly. Keep UOP >30 ml/hr. NPO until stable Preterm Labor • Labor occurring after 28th week but, before the 37th week gestation • Infant mortality and morbidity increase the earlier the delivery • 2nd leading cause of infant mortality – Prematurity and low birth weight • Cause: – Not fully known • Risk Factors: – Maternal • • • • CV or Renal disease Diabetes PIH Uterine or cervical anomalies • Cervical Incompetence • UTI • Anemia (See chart on page 750) – Fetal • Multiple pregnancy • Hydramnios • Fetal Infection – Placenta • Previa • Abruptio • PROM Assessment Data: EDC Course of pregnancy (problems) Fetal condition Maternal condition Contractions Greater than 6/hr with cervical changes Cervical changes Length < 25mm (allows greater entrance of microorganisms that weaken membranes and cause PROM – Infections • GBS • UTI – fFN test (fetal fibronectin) • should be – after 22 weeks gestation. Normal 23 weeks prior to onset of labor. – Salivary estriol • Elevates about 5 weeks before onset of labor. – PROM in previous pregnancy – CBC • Especially Hgb and Hct – L/S ratio • For fetal maturity PTL • Treatment: – Prevention • • • • • Early prenatal care Assessment of those at increased risk Promote adequate nutrition Teaching early signs of PTL Encourage patient to seek care if symptoms occur even if they seem mild • Treatment of infections ASAP with appropriate antibiotics PTL – Will not stop labor if: • Active labor with dilation >4 cm • Severe PIH • Fetal complications (Rh or gross anomalies) • RBOW with infection • Hemorrhage • Fetal demise PTL Care – Medical Care: • Bed rest • Monitor contractions and FHT • Position on left side • IV fluids • Limit vaginal exams • Assess and treat infections UTI +GBS • Assess and treat anemia • No sexual stimulation • Emotional support Drug Management – Drug management: • MgSO4 – 0.5 – 3 Gm IV usual dose – Usually first choice – Acts as CNS and smooth muscle relaxant – Always have Calcium gluconate on hand as antidote Give 5-10 mEq (5-10 ml) IV over a 3 min. period • Brethine (Terbutaline) – Asthma drug – Beta-adrenergic agonist that causes relaxation of the smooth muscles – 0.25 mg SQ and 5 mg po then 2.5-5 mg po q2-4 hours – Must be taken around the clock! – Side Effects » Fetal and maternal tachycardia » Nervousness » Pulmonary edema » Increased serum glucose » Decreased serum potassium Drug Therapy – Ritodrine (Yutopar) – • Beta-adrenergic agonist and causes smooth muscle relaxation. • 10 mg po q2h X 24 hr then 10-20 mg q4-6 hr • May also be give IV on pump at 0.1 – 0.35 mg / minute (Mix 150 mg in 500 ml D5W = 0.3 mg/ml) • Side Effects: – Tachycardia – Palpitations – Pulmonary edema Drugs affecting the Fetus • Glucocorticoids (Betamethasone or Celestone) – Used to stimulate fetal lung production of surfactant – 12 mg IM repeated in 12 to 24 hours – Works in 1 day – Lasts for 7 days – Must repeat weekly if undelivered and still at risk for PTL Home Treatment – Home Treatment • Bed rest on left side – with BRP – Increases placental blood flow – Decreases pressure on cervix – Complications: » CV deconditioning » Muscle and Ca loss » Weight loss » Depression » Anxiety What’s OK and Not OK • Brethine (or Yutopar) po – Be sure patient knows how to check pulse rate – Teach patient about chart to ensure pills taken as directed – Make sure she knows to take around the clock (set alarm clock) • No sexual stimulation • Increased fluids – Oral fluids – juice, milk, gelatin, etc – IV fluids – be careful if pts. on Brethine will be at risk for pulmonary edema – Encourage pt. to drink 1-2 8oz. glasses of water if begin to have contractions – Adequate hydration decreases the release of antidiuretic hormone and possibly oxytocin from the posterior pituitary gland and increases uterine blood flow thereby stabilizing decidual lysosomes so certain acids (arachidonic) will not be freed to be converted into prostaglandins. – Hydration also decreases the risk of UTI What else? • Report contractions >6/hr • Delegate home responsibilities to others • Home assessment – Stairs – Telephone access – Change in home routines – Change in expectations • Activities to do while on bed rest • Games to play with other children – Emotional Support – Delivery • Vaginal or C/S depends on individual • Increased risk for prolapsed cord Prolapsed Cord • Occult – cannot be seen or felt • Apparent – cord can be seen at the vaginal opening or felt on vaginal exam Occult Prolapse- Hidden What would you feel and hear? What would you see and hear? Which patient’s can have this? • Most commonly occurs: – – – – – – – – At the time of rupture of membranes If the presenting part is not engaged Abnormal presentation – breech, transverse lie, Small fetus Long cord Low lying placenta Hydramnios Multiple births • Signs and Symptoms: – Variable decelerations (especially at time of ROM) – Fetal tachycardia progressing to bradycardia • Treatment: – Change position to opposite side – Knee chest or trendelenburg position – Vaginal exam and place pressure on presenting part – If cord protruding from vagina – cover with wet gauze soaked in sterile saline – Prepare for immediate C/S – NEVER try to replace the cord Uterine Dystocia Dystocia- Long or difficult laborCauses 1. Dysfunctional Labor – ineffective contractions or ineffective bearing down. 2. Alterations in pelvic structure 3. Fetal causes – 1. 2. 3. 4. abnormal presentation or position anomalies size number 4. Maternal position 5. Psychological responses to labor DYSFUNCTIONAL LABOR • Usually occurs before 4 cm dilatation • Cause unknown • May be related to fear and tension • Signs and Symptoms: – Pain out of proportion to intensity of contractions – Pain out of proportion to effectiveness of contractions – poor effacement and dilatation – Contractions increase in frequency – Contractions uncoordinated – Uterus remains contracted between contractions (poor resting tone) • Results: – Maternal loss of control and exhaustion – Fetal asphyxia with meconium aspiration • Treatment: – Analgesia to allow rest (if no ROM or CPD) – Discontinue Pitocin if being induced – Sleeping pill if late in afternoon to allow overnight rest – When contractions resume may be normal SECONDARY OR HYPOTONIC UTERINE DYSFUNCTION • Most common type of dysfunction • Initially makes normal progress into the active stage of labor and then contractions become weak and ineffective or stops altogether. • Cause: – – – – Unknown CPD Malposition Overdistension of the uterus • Results: – Infection – maternal and fetal – Exhaustion – Psychological trauma – Fetal and neonatal death • Treatment: – Rule out CPD – Oxytocic stimulation or augmentation – Amniotomy (AROM) INADEQUATE VOLUNTARY EXPULSIVE FORCES • Compromised bearing down efforts prolong the second stage • Cause: – Heavy sedation – Conduction anesthesia (epidural or spinal) – Exhaustion due to: • • • • long labor lack of sleep hunger positioning • Signs and Symptoms: – No voluntary urge to push or bear down – Inadequate/ineffective pushing • Results: – Spontaneous vaginal birth prevented – Fetal asphyxia – Need for use of forceps or vacuum extractor • Treatment: – Coach mother in bearing down efforts – Position mother in favorable position for pushing – Low forcep or vacuum assisted birth – Episiotomy – C/S birth only if non-reassuring fetal status ALTERATIONS IN PELVIC STRUCTURE PELVIC DYSTOCIA • Occurs whenever there are contractures of the pelvic diameters that reduce the capacity of the bony pelvis. • Cause: – – – – – Congenital abnormalities Malnutrition Neoplasms Lower spinal disorders Immature pelvis in adolescent mothers • Signs and Symptoms: – Failure to progress Arrested descent – Weak uterine contractions during the first stage of labor – Cervical edema • Results: – Increased perinatal morbidity and mortality – Extensive perineal lacerations • Treatment: – C/S – Vacuum assisted vaginal birth (if completely dialated) SOFT TISSUE DYSTOCIA • Results from obstruction of the birth canal by an anatomic abnormality other than the bony pelvis • Cause: – Placenta Previa – Uterine fibroids – Ovarian tumors – Full bladder or rectum – Cervical edema Fetal causes of Dystocia ANOMALIES • • • • Gross ascites Abnormal tumors Myelomeningocele Hydrocephalus CEPHALOPELVIC DISPROPORTION • CPD • Also called Fetopelvic Disproportion (FPD) • Related to excessive fetal size >4000 gm • Cause: – Diabetes – Large parents – Multiparity Malposition • Most common is persistent occipitoposterior • Interferes with the fetal ability to exit the pelvis Malpresentation • Most common is breech – 3-4% of all deliveries – 25% of preterm births • Transverse lie • Face and brow presentations also a problem MUTIFETAL PREGNANCY • In only half of twin pregnancies do both fetuses present in the vertex position. • Second baby may turn to another position during the delivery of the first baby. • Usually have to attempt an intrapartal version. • May deliver first baby vaginally and second baby by C/S. POSITION OF THE MOTHER • The incidence of dystocia is increased in women confined to the recumbent or lithotomy position. • Increases the need for: – Augmentation of labor – Forceps or vacuum extractors – C/S • Knee-chest positon – Helpful for rotation of the fetus from posterior to anterior position • Sitting and squatting – Facilitates fetal descent during pushing PSYCHOLOGICAL RESPONSE • Hormones released in response to stress can also cause dystocia. – Pain – Absence of support person – Lack of knowledge NURSING DIAGNOSES FOR DYSTOCIA • ANXIETY R/T – Slowed labor progress – Perceived threat to well-being of self or fetus • PAIN R/T – Dystocia – Obstetric procedures • RISK FOR FETAL INJURY R/T – Obstetrical procedures – Prolonged labor process • RISK FOR MATERNAL INJURY R/T – Interventions implemented for dystocia • RISK FOR INFECTION R/T – Premature rupture of membranes – Operative procedures – Prolonged labor • FATIGUE R/T – Prolonged labor – Length of pushing • RISK FOR ALTERED PARENT-INFANT ATTACHMENT R/T – Unplanned cesarean birth – Increased pain • INEFFECTIVE INDIVIDUAL COPING R/T – Lack of knowledge regarding measures used to enhance labor and facilitate birth – Pain – Fatigue – Lack of support system • SITUATIONAL LOW SELF-ESTEEM R/T – Inability to labor and give birth as expected The Nurses contribution to Pain relief for the labor patient • Expectations • Why is controlling pain during labor important? • Pain tolerance vs pain threshold • Causes of pain during labor • Descriptions of pain during labor • Factors that cause greater discomfort • How can the nurse help/ Anesthesia/analgesia • Analgesia – Pain relief or less pain sensation • Anesthesia – Loss of sedation • When should patients receive anesthesia or analgesia? Assessment Requirements regardless of type of Anesthesia • Neuro – Level of consciousness • CV – B/P, P, with observation of color/temp and IV patency • Respiratory- Respiratory rate & rhythm with lung sound, ? Use of accessory muscles • GI – Nausea, vomitting • GU – Urinary output Drugs in L&D • • • • • • • • Phase Drugs Progress Latent Stadol /Demerol 1-3cm Active Stadol / Demerol* 3-9 cm 2nd stage Narcan / Pitocin Complete 3rd stage Pitocin Birth---*Avoid giving Narcotics late in labor In case of C/S Administer Bictra/ Choice of anesthesia is best discussed during pregnancy rather than labor Types of anesthesia • IV - Sodium Pentothal – Used for emergency only – causes Fetal depression and maternal laryngospasms • Regional • 1. Local infiltration • 2. Pudendal Block • 3. Caudal • 4.Lumbar Epidural* • 5.Saddle/spinal block Types of Anesthesia • Assess for allergies to “caine” drugs • Local Infiltration – repair Episiotomy or lacerations • Pudendal Block – external/internal, no affect on contractionsBlocks the perineal area for delivery Peridural anesthesia • Caudal - 1st & 2nd stage- Introduced in peridural space @ sacral hiatus • Lumbar “Epidural” – 1st & 2nd stageApproach from lumbar region- Most common Spinal anesthesia • Saddle block- Affects the portion that touches a saddle of a horse. Enters the subarachnoid space. Vaginal delivery • Spinal – Enters the subarachnoid space. Vaginal or C/S • Special nursing interventions required Common complications • Hypotension from Epidural due to : • 1.Rapid absorption of anesthetic agents • 2.Position (Supine Hypotension) • Hypotension from spinals due to: • 1.Peripheral vasodilation & altering return blood flow • 2.Position factor Nursing interventions • Increase IV fluids • Use Left pelvic tilt • Administer Ephedrine 5-10 mg IV as ordered by MD • Administer O2 8-12 L as ordered • Assess for fetal distress – What might you expect to see? Answer: • Fetal distress ie Fetal Bradycardia or Late decelerations • Causes: • 1. Rapid absorption of drug (Marcaine) • 2.Result of hypotension (mother) • 3.Inadequate placental perfusion for multiple causes. Can you list some of them? Other complications from anesthesia • • • • • Post spinal Headache A. Occurs 24-72 hours B. Last few days to several weeks C. Mild--------to severe!! D. H/A is positional- May be felt in back, neck, head & / or shoulders • E. Cause- Loss of cerebral spinal fluid • Treatment – analgesics, flat in bed, BR, Rest in prone position, increase hydration, *Epidural blood patch • Anaphylaxis – always possible