The Puzzle of Schizophrenia: Linking Neurochemistry, Cognition
advertisement
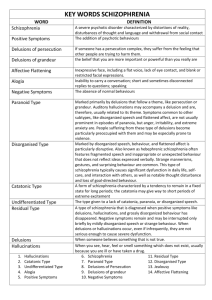
The Puzzle of Schizophrenia: Linking Neurochemistry, Cognition, and Symptoms Michael Kiang, MD, MS Dept. of Cognitive Science, UCSD Schizophrenia affects 1% worldwide onset throughout lifespan, most commonly late adolescence or twenties #7 cause of years lived with disability; #3 for 15-44 age group (WHO Global Burden of Illness Study) Schizophrenia "positive" symptoms (psychosis) “negative” symptoms Schizophrenia "positive" symptoms (psychosis) – hallucinations “negative” symptoms Schizophrenia "positive" symptoms (psychosis) – hallucinations – delusions “negative” symptoms types of delusions – persecutory: being harassed, cheated or persecuted – reference: events, objects, or others' behavior refers to oneself, or have a particular and unusual significance – grandiose: exaggerated conception of one's importance, power, or identity – guilt – control: one's actions or thoughts are being controlled by external forces; e.g. thought withdrawal/insertion/broadcasting/control – somatic (bodily) “A dog lay in wait for me as he sat on the steps of a Catholic convent. He got up on his hind legs and looked at me seriously. He then saluted with his front paw as I approached him. Another man was a little way in front of me. I caught up to him hurriedly and asked if the dog had saluted him too. An astonished ‘no’ told me I had to deal with a revelation addressed to me.” Kurt Schneider, Klinische Psychopathologie (Clinical Psychopathology), 1931 Compton (2003): "Internet delusions." A 53-year-old woman, with a history of one hospitalization 1.5 years previously, presented to the hospital after calling the police due to increasing worries at home—“the control had gotten especially strong.” She described…that the Internet had been controlling her and her home for the past 3 years. For example, when she walked around in her home, if she bumped into furniture, she attributed this to the Internet controlling her. She believed that the Internet also controlled her appliances turning on and off, that it changed channels on the television, and that it caused her to burn herself on the iron or stove. Other psychiatric symptoms included auditory hallucinations of voices whispering to her, passive suicidal thoughts, and vague worries that her grandson was in danger in some way. When asked about computers and the Internet, the patient denied having any familiarity with computers or having ever used computers in any capacity. When asked to describe what the Internet is, she commented that she assumes that it is “some big computer somewhere.” Schizophrenia "positive" symptoms (psychosis) – hallucinations – delusions – disorganized speech – disorganized behavior Disorganized Speech in Schizophrenia sequences of concepts appear unrelated unusual wording irrelevant responses thought disorder Schizophrenia "positive" symptoms (psychosis) – delusions – hallucinations – disorganized speech – disorganized behavior “negative” symptoms – flat affect – poverty of speech – apathy / social withdrawal / poor hygiene – cognitive deficits Schizophrenia diagnostic criteria (DSM-IV): A) 2 or more of the following, for at least 1 month: • delusions • hallucinations • disorganized speech • disorganized behavior • negative symptoms – only 1 required if delusions are bizarre; or hallucinations consist of a voice keeping up a running commentary on the person’s behavior or thoughts, or 2 or more voices conversing with each other B) symptoms cause social/occupational dysfunction C) some sign of the disturbance has lasted at least 6 months D) not caused by a substance or a medical illness Schizophrenia genetic predisposition (e.g. twin studies) unknown environmental contribution (prenatal, childhood, adult?) Mortensen et al. (1999) Mortensen et al. (1999) Schizophrenia no diagnostic findings on neuropathology / structural brain imaging on average, smaller temporal lobe gray matter volume Discovery of Antipsychotic Medication Paris, 1952: surgeon Laborit tested chlorpromazine (known as antihistamine) for surgical shock – it calmed agitated patients, caused a "marked indifference" Paris, 1953: psychiatrists Delay and Deniker found that it improved psychotic symptoms Montreal, 1954: first use of antipsychotics in North America (Lehmann) 1960s: deinstitutionalization Danvers State Hospital, Danvers, MA In CA, from 1955 to 1980, institutionalized population declined from 37 000 to 2 500 Antipsychotic Medication: Problems not fully effective at reducing symptoms in all patients Antipsychotic Medication: Problems not fully effective at reducing symptoms in all patients frequently do not reduce negative symptoms as effectively as they do positive symptoms Antipsychotic Medication: Problems cause Parkinsonian side effects – slowing of movements (bradykinesia) – tremor – rigidity Antipsychotic Medication: Mechanism Seeman (1975): discovered dopamine receptor to which antipsychotics bind (block) since then, all effective antipsychotic medications have been found to bind to this receptor (D2) nigrostriatal mesocortical mesolimbic (nucleus accumbens) Controls Patients dopamine level D2-selective radiolabelled ligand Dopamine Dopamine D2 receptor Abi-Dargham et al (2000) Controls Patients dopamine level D2-selective radiolabelled ligand Dopamine Dopamine D2 receptor Abi-Dargham et al (2000) Controls Patients dopamine level deplete dopamine D2-selective radiolabelled ligand Dopamine Dopamine D2 receptor Abi-Dargham et al (2000) Pathophysiology of Schizophrenia Biochemical Cognitive Phenomenological Dopaminergic overactivity ??? Delusions, hallucinations, disorganization How Do Delusions Improve? Biochemical Cognitive Phenomenological Dopamine D2 receptors blocked ??? Delusions improve How Do Delusions Improve? Although D2 blockade is rapid, improvement in delusions is gradual (usually over a period of weeks) Pathophysiology of Delusions: A Hypothesis (Kapur, 2003) In psychosis, increased dopamine activity causes abnormal salience of ordinary stimuli nigrostriatal mesocortical mesolimbic (nucleus accumbens) Pathophysiology of Delusions: A Hypothesis (Kapur, 2003) In psychosis, increased dopamine activity causes abnormal salience of ordinary stimuli Persistent abnormal salience leads to delusion formation, as an attempt to explain this abnormal sense of significance Abnormal Salience “A dog lay in wait for me as he sat on the steps of a Catholic convent. He got up on his hind legs and looked at me seriously. He then saluted with his front paw as I approached him. Another man was a little way in front of me. I caught up to him hurriedly and asked if the dog had saluted him too. An astonished ‘no’ told me I had to deal with a revelation addressed to me.” Kurt Schneider, Klinische Psychopathologie (Clinical Psychopathology), 1931 Pathophysiology of Delusions: A Hypothesis (Kapur, 2003) In psychosis, increased dopamine activity causes abnormal salience of ordinary stimuli Persistent abnormal salience leads to delusion formation, as an attempt to explain this abnormal sense of significance Antipsychotics decrease dopamine activity and reverse abnormal salience An extended period free of abnormally salient stimuli allows delusion to gradually extinguish Belief Perseverance More favorable toward CP 2 Change in Attitude 1.5 1 0.5 0 Proponents Opponents -0.5 -1 -1.5 -2 -2.5 Less favorable toward CP After Pro-CP study After Anti-CP study Lord et al. (1979) Time Antipsychotic treatment initiated 6Abnormal salience of stimuli 6Preoccupation 6Negative Mood 6Conviction 6Action Studying How Delusions Improve Dimensions of Psychosis questionnaire Based on detailed interview about a principal delusion, interviewer rates: – conviction – external perspective (insight) – cognitive preoccupation – emotional involvement – behavioural impact Behavioural impact Emotional involvement Cognitive preoccupation Conviction External perspective Mizrahi, Kiang, Mamo et al. (2006) Summary symptoms tend to co-occur, but not all are present in each patient interaction of genetic and environmental factors causes illness brain studies suggest an abnormality of dopaminergic function further research required on how this is related to symptoms, or whether it is the primary brain abnormality Total Prison Mental Hospital Harcourt (2006)