BM - Home
advertisement

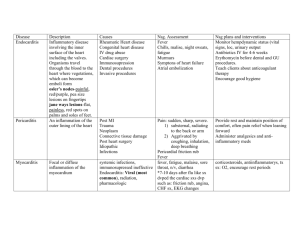
ELUSIVE BUG?!! Gebre K Tseggay, MD November 30, 2005 The Patient • 73yo WF with h/o MV-repair, presented with a dry cough and worsening shortness of breath which started as a “chest cold” 2 weeks earlier. She denied subjective fever or chills, but reported several weeks h/o fatigue and significant limitation in her daily activities. She denied ill contacts. A CXR suggested a RLL infiltrate and levofloxacin was started in the ER. Although she did not have fever in the ER, she had intermittent, mostly lowgrade fever after admission. • TEE, done 4 days into Rx, showed two mitral valve annular vegetations. • Endocarditis was presumed and ID consult called. • PMH/PSH: – Severe MR (s/p MV-annuloplasty about a year ago), and has had significant weight loss since her mitral valve surgery. – Left nephrectomy for atrophic kidney (4 decades ago), – Clipping of brain aneurysm (2 decades ago), – Hypertension, osteoporosis, & essential tremor. • MEDS: Levaquin 500mg q24h, Lovenox, ASA, dobutamine. • FH: N/C. • SH: No cig, alcohol, drugs. She lives alone, but her daughter lives next door. Volunteers regularly at an elementary school. • EPIDEMIOLOGIC Hx: No ill contacts, no recent travel, no arthropod or other animal bites/scratches. Last dental visit a year earlier. She has a dog, and has bird cages in yard (but no pet birds). Her daughter has cats. • ALLERGY: Penicillin, Sulfa • EXAM: Cachectic elderly pt. Alert, well oriented. • T 97.8F, P 74, 22, BP 152/78, RR 20/min, O2Sat 89% on RA • HEENT: PEERLA, EOMI, without conjunctival/buccal mucosa petechiae. • Lungs: Few crackles over rt base. • Heart: RR, without murmur. • Abd: soft, NT, normoactive BS, no HSM • Ext: no e/c/c. • Skin: without rash, no obvious peripheral stigmata of SBE. • • • • • • WBC 5.2, Hgb 13.5, Plt 199K, BUN 16. cr 0.8. ESR 20, CRP 8.4 mg/dL BC : negative (was drawn after a dose of Levaquin) CXR: RLL atelectasis vs infiltrate EKG: SR, LVH, non-specific ST-T changes TEE: Reduced LV systolic function and moderate-sized, mobile vegetations attached to the posterior mitral valve ring. Questions A culture-negative infective endocarditis? Vs Vegetations of a non-infectious etiology? Proposed scheme for the pathogenesis of infective endocarditis NON-INFECTIOUS CAUSES Of ENDOCARDITIS • Antiphospholipid syndrome: Primary or Secondary (e.g. w SLE or malignancies) • Neoplasia Associated: Atrial Myxoma, Marantic endocarditis, Carcinoid • AI associated: Rheumatic carditis, SLE, PAN, Behcet’s disease • Postvalvular surgery: Thrombus, stitch, or other postsurgical changes • Miscellaneous: eosinophilic heart disease, ruptured mitral chordae, myxomatous degeneration AHA Scientific STATEMENT on infective endocarditis. Circulation. June 14, 2005 ©2005 UpToDate® Vegetations (arrows) due to viridans streptococcal endocarditis involving the mitral valve. CAN YOU HAVE INFECTIVE ENDOCARDITIS with Negative Blood Cultures? • Yes, BCx may be negative in up to 2.5-30% of IE due to: – Administration of abx before blood cultures – Inadequate microbiological techniques – Infection with highly fastidious bacteria – Infection with nonbacterial pathogens Impact of Taking Antibiotics Before Blood Cultures Are Obtained • It’s the leading cause of BC-negative IE. • Reduces the recovery rate of bacteria by 35-40%. – The length of time the BCx will remain negative is determined by the susceptibility of the organism and the duration of antibiotic use before blood cultures are drawn. – BC of pts who receive longer course of high dose, bactericidal abx may remain negative for weeks. – If the initial BCx were negative after only a few days of abx, infective endocarditis pts may have a positive BCx after only several days without antibiotics. Tunkel AR, Kaye D. N Engl J Med. 1992; 20: 1215–1217 Back to Our Patient • Antibiotic (levofloxacin) was discontinued on day 5 • How long can you safely hold antibiotics? – “If the initial blood cultures are negative, a delay of 2 to 4 days will allow additional blood cultures to be obtained without the confounding effect of further antibiotic therapy and without increased morbidity from IE.” Circulation. 1998;98:2936-2948. AHA Scientific Statement • Blood cultures were taken daily (and some held for 3 weeks). • UNFORTUNATELY, ALL BLOOD CULTURES REMAINED NEGATIVE!! ARE THE CRITERIA FOR DIAGNOSIS OF INFECTIVE ENDOCARDITIS APPLICABLE EVEN IN PATIENTS WITH NEGATIVE BLOOD CULTURES? Definition of Infective Endocarditis According to the Modified Duke Criteria I. Definite IE Pathological criteria • Microorganisms demonstrated by culture or histological examination of a vegetation, a vegetation that has embolized, or an intracardiac abscess specimen; or • Pathological lesions; vegetation or intracardiac abscess confirmed by histological examination showing active endocarditis Clinical criteria • 2 major criteria; or • 1 major criterion and 3 minor criteria; or • 5 minor criteria II. Possible IE • 1 major criterion and 1 minor criterion; or • 3 minor criteria III. Rejected - Firm alternative diagnosis explaining evidence of IE; or - Resolution of IE syndrome with antibiotic therapy for <4 days; or - No pathological evidence of IE at surgery or autopsy, with antibiotic therapy for <4 days; or - Does not meet criteria for possible IE as above MAJOR CRITERIA 1. POSITIVE BLOOD CULTURE • Typical microorganism for infective endocarditis from two separate blood cultures -Viridans streptococci, Streptococcus bovis, HACEK group, Staphylococcus aureus, or -Community-acquired enterococci in the absence of a primary focus, or • Persistently positive blood culture, defined as recovery of a microorganism consistent with infective endocarditis from: Blood cultures drawn >12 h apart; or All of 3 or a majority of 4 or more separate blood cultures, with first and last drawn at least 1 h apart • Single positive blood culture for Coxiella burnetii or phase I IgG antibody titer of >1:800 2. EVIDENCE OF ENDOCARDIAL INVOLVEMENT • Positive echocardiogram Oscillating intracardiac mass on valve or supporting structures or in the path of regurgitant jets or in implanted material, in the absence of an alternative anatomic explanation, or - • Abscess, or New partial dehiscence of prosthetic valve, or New valvular regurgitation (increase or change in preexisting murmur not sufficient) MINOR CRITERIA 1. Predisposition: predisposing heart condition or injection drug use 2. Fever > 38.0°C (> 100.4°F) 3. Vascular phenomena: major arterial emboli, septic pulmonary infarcts, mycotic aneurysm, intracranial hemorrhage, conjunctival hemorrhages, Janeway lesions 4. Immunologic phenomena: glomerulonephritis, Osler's nodes, Roth's spots, rheumatoid factor 5. Microbiologic evidence: positive blood culture but not meeting major criterion as noted previously or serologic evidence of active infection with organism consistent with IE BACK TO OUR PATIENT (and The Modified Duke Criteria) • • • • Has evidence of endocardial involvement = I major criterion Has a predisposing condition = 1 minor criterion Has fever = 1 minor criterion 1 major + 2 minor criteria= ‘Possible’ infective endocarditis Definite IE 2 major criteria 1 major criterion and 3 minor criteria 5 minor criteria Possible IE 1 major criterion and 1 minor criterion 3 minor criteria Not a Duke’s Criteria, but………. CULTURE-NEGATIVE ENDOCARDITIS JAMA. Vol. 293 No. 24, June 22/29, 2005 ETIOLOGY OF CULTURE-NEGATIVE INFECTIVE ENDOCARDITIS – Partially-treated bacteria. – Fastidious bacteria. – Non-bacterial pathogens (e.g., fungi) Fastidious bacterial endocarditis: – – – – – – – – – HACEK (Haemophilus sp, Actinobacter, Cardiobacterium, Eikenella, Kingella) Abiotrophia spp Bartonella quintana, B. henslae Q-fever Brucellosis Whipple’s… Chlamydia … Mycoplasma… Other? Relative frequency of bacteria as etiologic agents of IE (Only infectious agents reported more than 50 times in the literature are listed) • Bacterium • • • • • • • • • No. of cases reported Coxiella burnetii Brucella spp. Abiotrophia spp. Actinobacillus actinomycetemcomitans Haemophilus aphrophilus Cardiobacterium hominis Corynebacterium diphtheriae Haemophilus parainfluenzae Listeria monocytogenes 359 120 100 93 78 76 67 66 58 Clinical Microbiology Reviews, January 2001, p. 177-207, Vol. 14, No. 1 Blood Culture-Negative Endocarditis in a Reference Center(1983-1991): Etiologic Diagnosis of 348 Cases French National Reference Center for Rickettsial Diseases • C. burnetii • Bartonella sp • Rare fastidious agents 167 (48%) 99 (28%) 5 (1%) (e.g T. whipplei, Mycoplasma hominis, Abiotrophia elegans and Mycoplasma hominis) Among those with IE but with unidentified etiology: • Took abx before blood cultures 79% • No etiology OR explanation found 1% Houpikian P and Raoult D Medicine 2005;84:162 • • • • • Epidemiological Clues in Etiological Diagnosis of Culture-Negative Endocarditis Poor dental health, dental • Alcoholism procedures – Bartonella – Strep viridans – Aeromonas sp – Nutrionally variant streptococci – Listeria – Abiotrophia defectiva – S.pneumoniae – Granulicatella sp – B-hem strep – Gemella sp – HACEK • AIDS Homeless, body lice – Salmonella – Bartonella sp – Strep pneumo Dog-cat exposure – Staph aureus – Bartonella – Pasteurella sp • Injection Drug user – Capnocytophaga sp – S.aureus Contact with contaminated milk – Coag-neg staph – Brucella – B-hem strep – Coxiella burnetii – Fungi – Erysipelothrix sp – Aerobic GNR (including Ps.a) Gastrointestinal lesions – Streptococcus bovis – Enterococcus – Clostridium septicum Culture-negative Endocarditis Diagnosis HISTORY Contact with animals; for example contact with: • a cat (including scratches or bites) or cat flea suggests Bartonella henselae or Pasteurella spp. • Cattle should suggest a role for C. burnetii or Brucella spp. • Parrots, pheasants, and pigeons have been reported to play a role in Chlamydia psittaci endocarditis • Domestic animals such as swine, fish, and poultry is frequently reported in the history of patients with Erysipelothrix endocarditis. • The human body louse is involved in the transmission of Bartonella quintana Dental procedure may suggest HACEK group bacteria Occupational exposure • Farmers and veterinarians are exposed to both C. burnettii and Erysipelothrix. • Butchers, fishermen, and even in homemakers by contact with organic matter in which the Erysipelothrix is commonly found Culture-negative Endocarditis Laboratory Diagnosis •Blood cultures - Hold for prolonged incubation (> 2-3wks) - Other culture techniques (media supplements, lysis-centrifugation, etc..) •Serology •Antigen Testing •Valve Culture •Histopathology •PCR [specific, broad-based (16s rDNA)] Abiotrophia spp. (formerly known as nutritionally deficient streptococci) showing satellite growth with Staphylococcus aureus. Unité des Rickettsies, Marseilles, France ©2005 UpToDate® Immunohistochemical demonstration of Coxiella burnetii in a heart valve of a patient with Q fever endocarditis. Magnification, ×600. Immumoalkaline phophatase staining was used. ©2005 UpToDate® Pathogen Diagnostic procedure Brucella spp. Blood cultures Serology Culture, immunohistology and PCR of surgical material Coxiella burnetii (agent of Q Serology: IgG phase 1 > 1/800 fever) Bartonella spp. Tissue culture, immunohistology and PCR of surgical material Blood cultures Serology Culture, immunohistology and PCR of surgical material Chlamydia spp. Serology § Culture, immunohistology and PCR of surgical material Mycoplasma spp. Serology Culture, immunohistology and PCR of surgical material. Legionella spp. Blood cultures Serology Culture, immunohistology and PCR of surgical material. Tropheryma whippelii (agent of Whipple's disease) Histology and PCR of surgical material Culture-negative Endocarditis Treatment – Selection of the antibiotics is very difficult – May expose to unnecessary toxicity, e.g. using aminoglycosides – Usual treatment directed at the more common bacterial pathogens, by considering: • Epidemiologic features • Clinical course When Choosing Empiric Abx for CNBE Classify pts into two Groups: 1. Those who received abx prior to collection of blood cultures: Native valve: • Acute presentation (Staph aureus>>) • Subacute presentation (S.aureus, strep viridans, enterococci, HACEK) Prosthetic valve: • Within the year post-valve surgery (MRSA/MRSE>>) • > I year after surgery: (OSSA, Strep viridans, enterococci) 2. Organisms that do not grow in routinely used blood culture systems: • Bartonella, Chlamydia, Coxiella burnetti, Brucella, Legionella species, Tropheryma whippleii, non-candida fungi. • Bartonella(quintana>henslae)>>, Coxiella b, and Brucella may be the most commonly identified causes of CNBE (or both?) Treatment of Some Agents of Culture-negative Endocarditis PATHOGEN TREATMENT DURATION • Brucella sp Doxy + rifampin or trim/sulfa >3 mos • Coxiella burnetti Doxy + hydroxychloroquine or Doxy+ quinolone >18 mos >6 mos • Bartonella sp beta-lactams or doxy and aminoglycosides • Chlamydia Doxy (newer quinolones?) • Mycoplasma Doxy (quinolones?) >3 mos • Legionella macrolide + rifampin or newer quinolones >6 mos • Whipple’s >1yr • HACEK Trim/sulfa Beta lactam + aminoglycosides ceftriaxone (or ampicillin+gent) ? 4-6 wks Organisms to consider in empiric treatment of Prosthetic Valve endocarditis ©2005 UpToDate ® Echocardiographic Features That Suggest Potential Need for Surgical Intervention Vegetation • Persistent vegetation after systemic embolization • Anterior mitral leaflet vegetation, particularly with size >10 mm* • >1 embolic events during first 2 wk of antimicrobial therapy* • Increase in vegetation size despite appropriate antimicrobial therapy* Valvular dysfunction • Acute aortic or mitral insufficiency with signs of ventricular failure • Heart failure unresponsive to medical therapy • Valve perforation or rupture Perivalvular extension • Valvular dehiscence, rupture, or fistula • New heart block • Large abscess or extension of abscess despite appropriate antimicrobial therapy . *Surgery may be required because of risk of embolization. Surgery may be required because of heart failure or failure of medical therapy. Echocardiography should not be the primary modality used to detect or monitor heart block. BACK TO OUR PATIENT • ~6 weeks Rx: A f/up TEE showed same mobile MV vegetations, with possible abscess (?) between AV & MV. • When some questions arose about whether she really has an abscess a labeled WBC-scan was done for confirmation. HOSPITAL COURSE (Cont’d) • Surgery was strongly recommended, but, after discussions between patient, family, CTS and Cardiology surgery was deferred fearing she would not survive it. • Transferred to KH where tube feeding was started to improve nutritional status, and abx continued. • She did better overall , her wt rose up to ~100 lbs (from 80’s). More discussions about surgery ensued, but deferred once more after long discussions. • Pt was transferred to a NH, where iv abx were cont’d until 6/2005 (4 months of Rx), then discharged to home on po doxycycline and rifampin. • She was doing “OK” at home until 8/17/2005 (6 months of Rx) HOSPITAL COURSE (Cont’d) • Readmitted with a TIA and TEE showed a moderatesized mobile MV vegetation. • Surgery was done next day. – Findings: posterior leaflet vegetation and a small ring abscess. Debridement of infected material of posterior annulus,vegetectomy, and removal of the old ring was done (valve replacement not done). Valve tissue cultures, PCR, pathology remained non-diagnostic. Some Lab studies done in our patient • Blood culture: – Routine BC – BC for fungus (isolator tube) • Serology (repeated twice): – Brucella, – Bartonella,Coxiella, – Chlamydia, – Mycoplasma, – Legionella, – Fungal serology • ANTIGEN TESTING: – Urine Pneumococcal antigen – Urine Legionella Antigen – Urine histoplasma antigen, – Serum Cryptococcal antigen • • NON-ID tests: ANA, RF, APA PCR: – T. whippeli, Bartonella, Qfever, Chlamydia, Mycoplasma (on valve tissue) • HISTOPATHOLOGY with special stains All remained essentially negative ELUSIVE BUG INDEED!!! Clinical and Laboratory Features of Infective Endocarditis Feature Frequency, % Fever 80–90 Chills and sweats 40–75 Anorexia, weight loss, malaise 25–50 Myalgias, arthralgias 15–30 Back pain 7–15 Heart murmur 80–85 New/worsened regurgitant murmur 10–40 Arterial emboli 20–50 Splenomegaly 15–50 Clubbing 10–20 Neurologic manifestations 20–40 Peripheral manifestations (Osler's nodes, subungual hemorrhages, Janeway lesions, Roth's spots) Petechiae 2–15 10–40 Laboratory manifestations Anemia 70–90 Leukocytosis 20–30 Microscopic hematuria 30–50 Elevated ESR Rheumatoid factor >90 50 Circulating immune complexes 65–100 Decreased serum complement 5–40 BARTONELLA SPECIES • are small, gram-negative bacilli that have recently been shown to cause endocarditis. • Currently, Bartonella quintana, the agent of trench fever, and Bartonella henselae, the agent of cat-scratch disease, are the major causes of Bartonella endocarditis. • Single cases of endocarditis caused by Bartonella elizabethae and Bartonella vinsonii subspecies berkhoffii have also been reported Epidemiologic Findings in 16 Patients with Endocarditis Caused by Bartonella quintana or Bartonella henselae AIM. 15 October 1996 | Volume 125 Issue 8 | Pages 646-652 http://www.hosppract.com/issues/1998/12/celout.htmThe McGraw-Hill Companies.2001 ©2005 UpToDate® The optimum antibiotic treatment for Bartonella endocarditis is unknown Q Fever • zoonotic disease caused by Coxiella burnetii. • Coxiella burnetii is a strict intracellular pathogen that grows in the acidic phagolysosome of the host cell. • Highly infectious. Resistant to desiccation. • Contracted through exposure to infected ruminants (especially parturient goats, sheep, and cattle), with incubation time of 3-30 days. -Ingestion of infected unpasteurized milk may also transmit the disease • Inhalation of aerosols of contaminated soil is the major mode of transmission. • Relatively common cause of IE in geographic areas of the world in which cattle, sheep, and goat farming are common. • Distributed broadly throughout the United States too. • Designated a possible bioterrorism agent Q-Fever Clinical Findings • • Asymptomatic (up to 60% of infections). Acute disease is characterized most frequently by: (1) High fever and headache; (2) Pneumonia or hepatitis in approximately 60% of acutely ill persons; (3) Infrequent acute manifestations: pericarditis, myocarditis, or meningoencephalitis. • Chronic disease occurs in <1% of infected patients: (1) Occurs predominantly in patients with underlying valvular heart disease, vascular aneurysms, or vascular grafts; (2) Manifests primarily as culture-negative endocarditis, (3) Less commonly as vascular or osteoarticular infection Q-fever Endocarditis •Q-fever IE usually affects prosthetic or previously damaged aortic or mitral valves. •It has small vegetations often missed by echocardiography. •. Q-Fever Laboratory Testing (1) Demonstration of fourfold or greater changes in IgG or IgM class-specific testing of paired acute- and convalescent phase serum samples by immunofluoresence antibody; (2) Serology. (1) High Phase II antibody titres indicates recent contact with infection by C. burnetii, usually within last 6-8 months; (2) high Phase I antibodies = chronic infection (e.g SBE) (3) Detection of C. burnetii by polymerase chain reaction or immunohistochemical staining. (4) blood culture. (N.B.: Hazard to laboratory workers) Q-FEVER MANAGEMENT______ • Acute disease: doxycycline 200 mg/day for 2-3 weeks. • Acute disease in patients with valvular heart disease: doxycycline 200 mg/day plus hydroxychloroquine 600 mg/day, for 1 year; dosage of hydroxychloroquine adjusted to maintain plasma level at 1 ± 0.2 µg/ml. • Chronic: doxycycline and hydroxychloroquine, dosage as above, for 1.5-3 years; cessation of therapy determined by appropriate serologic profile. • The optimal regimen or duration of antimicrobial therapy for Q-fever IE is unknown. – Doxycycline with trimethoprim/sulfamethoxazole, rifampin, or fluoroquinolones is the mainstay of therapy. – However, eradication of the organisms from vegetations with medical therapy is unlikely, and reinfection of prosthetic material after surgical replacement of infected valves commonly occurs. – Clinical response tends to persist as long as the drug regimen continues, but viable C burnetii can be recovered from valve tissue even after years of antimicrobial therapy The acidic conditions of the phagolysosome, where the organism resides , may inhibit antibiotic activity Q-fever: Cures of IE after treatment with a combination of doxycycline and hydroxychloroquine (to alkalinize the phagolysosome) • • • • Prevention Minimize or restrict exposures to livestock birthing areas. • Dispose of birth products properly (e.g., incinerate placenta and aborted fetuses). • Report all human cases to state health departments (Q fever is a nationally notifiable disease) WHIPPLE’S SYNDROME • Trophyrema whippeli ©2005 UpToDate® ©2005 UpToDate® ©2005 UpToDate® ©2005 UpToDate® ©2005 UpToDate® BRUCELLA • Brucellae are facultative intracellular Gram-negative bacilli. • Infect humans after ingestion of infected undercooked meat or unpasteurized milk, inhalation of infectious aerosols, or direct contact with infected tissues. • Cause occupational disease of veterinarians, abattoir workers, livestock handlers, and shepherds; http://gsbs.utmb.edu/microbook/ch028.htm ©2005 UpToDate® ©2005 UpToDate® BRUCELLA ENDOCARDITIS • It causes 4% of all IE cases in Spain. • Previously damaged aortic or mitral valves develop bulky vegetations, – Followed commonly by valve destruction, perivalvular abscesses, and CHF. • Few patients with Brucella IE have been cured with antimicrobial agents alone. • Most require valve replacement in combination with antimicrobial agents. • The optimal regimen or duration of antimicrobial therapy for Brucella endocarditis is unknown: doxycycline plus either streptomycin or gentamicin or doxycycline plus trimethoprim/sulfamethoxazole or rifampin have been recommended by some authorities for 8 weeks and up to 10 months after valve replacement. NonBacterial Thrombotic Endocarditis (NBTE) •Most cases of IE, although not all, begin with a damaged endocardial surface. •Damage to the endocardium may be caused by a number of factors, ranging from rheumatic disease to senile degeneration and calcification; indeed, any excessive turbulence or high-pressure gradient may cause injury to the nearby endocardium. • Next, fibrin-platelet aggregates develop at the site of damage to form sterile vegetations, also termed nonbacterial thrombotic endocarditis (NBTE). •NBTE may occur spontaneously in patients with systemic illnesses (for instance, the marantic endocarditis of malignancy or other wasting diseases or Libman-Sacks endocarditis in systemic lupus erythematosus) Etiology of Prosthetic Valve Endocarditis Organism Time of Onset after Valve Implantation and Percentage of Cases 2 months Coagulase-negative 2–12 months > 12 months 54 56 15 Staphylococcus aureus 8 9 13 Gram-negative bacilli 12 3 1 Streptococci --- 3 34 Enterococci --- 6 11 Corynebacteria 8 --- 1 HACEK --- 3 14 Fungi 6 6 3 Miscellaneous 6 6 1 staphylococci © 2004 WebMD Inc. Chronology of important scientific and medical events in the history of infective endocarditis Year Scientist/physician, Country Major findings 1554 Jean François Fernel, France Earliest report of endocarditis in book Medicini 1669 Richard Lower, England Accurately described tricuspid valve endocarditis 1646 Lazarus Riverius, France Described unusual "outgrowths" from autopsy of patient with endocarditis; detected murmurs by placing hand on patient's chest 1708 Giovanni Maria Lancisi, Italy Described unusual structures in entrance of aorta 1715 Raymond Vieussens, France Described abnormality in aortic mitral valve 1749 Jean-Baptiste Sénac, France Described valvular lesions 1769 Giovanni Battistu Morgagni, Italy Linked infectious disease and endocarditis; observed association with the spleen 1784 Eduard Sandifort, France Accurately drew intracardiac abnormalities 1797 Matthew Baillie, England Showed relationship between rheumatism and heart disease 1799 Xavier Bichat, France Described inflammatory process associated with endocarditis 1806 Jean Nicholas Corvisart, France Described unusual structures in heart as "vegetations," syphilitic virus as causative agent of endocarditis, and theory of antiviral treatment of endocarditis 1809 Allan Burns, England Indicated vegetations were not "outgrowths" or "buds" but particles adhering to heart wall 1815 Friedrich Kreysig, Germany Elucidated inflammatory processes associated with endocarditis 1816 Théophile Laënnec, France Invented cylindrical stethoscope to listen to heart murmurs; dismissed link between venereal disease and endocarditis 1832 James Hope, England Confirmed Laënnec's observations 1835– 40 JeanBaptiste Bouillaud, France Named endocardium and endocarditis; described symptoms; prescribed herbal tea and bloodletting as treatment regimen; described link between acute rheumatoid arthritis and endocarditis 1852 William Senhouse Kirkes, England Described consequences of embolization of vegetations throughout body. Described cutaneous nodules (named "Osler's nodes" by Libman) 1858– 71 Rudolph Virchow, Germany Examined fibrin vegetation associated with endocarditis by microscope; coined term "embolism;" discussed role of bacteria, vibrios, and micrococci in endocarditis 1861 JeanMartin Charot, France Confirmed Virchow's theory on emboli 1861 Alfred Vulpian, Germany Confirmed Virchow's theory on emboli 1862 Etienne Described granulations or foreign elements in blood and valves, which Lancereaux were motile and resistant to alkalis , France 1868–70 Samuel Wilks, England Described infected arterial blood as originating from heart; proposed scarlet fever as cause of endocarditis 1869 Emmanuel Winge, Norway Established "parasites" on skin transported to heart and attached to endocardium; named "mycosis endocardii" 1872 Hjalmar Heiberg, Norway Detected microorganisms in vegetations of endocarditis 1878 Edwin Klebs, Germany All cases of endocarditis were infectious in origin 1878 Ottomar Combined experimental physiology and infection to produce animal model Rosenbach, of endocarditis in rabbit; noted valve had to be damaged before bacteria Germany/P grafted onto valve oland 1878 Karl Koester, Germany Micrococci enter vessels that valves were fitted into; valves exposed to abnormal mechanical attacks over long period created favorable niche for bacterial colonization 1879 Joseph Hamburg, Germany Virchow's student; employed early animal model of endocarditis 1879 Germain Sée, France Proposed etiology of endocarditis was based on infectious model and treatment should focus on eliminating "parasitic infection" 1880 Jacques Doleris, France Working with Pasteur, proposed use of routine blood cultures 1881–86 Arnold Netter, France Believed endocarditis could appear during various infections; noted translocation of respiratory pathogen from pulmonary lesion to valve through blood 1883 Michel Peter, France Believed microorganisms were result, not cause, of endocarditis 1884 Joseph Grancher, France Named disease "infective endocarditis" 1886 Valimir Wyssokowitsch and Johannes Orth, Germany Demonstrated various bacteria introduced to bloodstream could cause endocarditis on valve that had previous lesion 1885 Sir William Osler, Canada Synthesized work of others relating to endocarditis 1899 Hermann Lenhartz, Austria Described streptococcal, staphylococcal, pneumococcal, and gonococcal endocarditis 1903 Hugo Schottmüller, Germany First described "endocarditis lenta" 1909 John Alexander Mullen, Canada Credited by Osler as first to observe cutaneous nodes (named "Osler's nodes" by Libman) in patients with endocarditis 1909 Sir Thomas Horder, England Analyzed 150 cases of endocarditis and published diagnostic criteria relating to signs and symptoms 1910 Emmanual Libman, USA Described initial classification scheme to include "subacute endocarditis," with clinical signs/symptoms; absolute diagnosis required blood cultures 1981 Von Reyn, USA Described Beth Israel criteria based on strict case definitions 1994 David Durack, USA New criteria utilizing specific echocardiographic findings 1995 American Heart Association, USA Antibiotic treatment of adults with infective endocarditis caused by streptococci, enterococci, staphylococci, and HACEKa microorganisms 1996 Pierre Fournier, France Modified Duke criteria to allow serologic diagnosis of Coxiella burnetii • Clinical Study of Culture-Negative Endocarditis. Medicine. 82(4):263-273, July 2003 infective endocarditis patients have CNE • Emerging Issues in Infective Endocarditis Beverley C. Millar* and John E. Moore* *Belfast City Hospital, Belfast, Northern Ireland, United Kingdom Suggested citation for this article: Millar BC, Moore JE. Emerging issues in infective endocarditis. Emerg Infect Dis [serial on the Internet]. 2004 Jun [date cited]. Available from: http://www.cdc.gov/ncidod/EID/vol10no6/03-0848.htm About 20% in a Scandinavian population of 1997 American Heart Association, USA Guidelines for preventing bacterial endocarditis 1997 Lamas and Eykyn, UK Suggested modifications to Duke criteria for clinical diagnosis of native valve and prosthetic valve endocarditis: analysis of 118 pathologically proven cases 1998 Working Party of the British Society for Antimicrobial Chemotherapy, UK Guidelines for antibiotic treatment of streptococcal, enterococcal, and staphylococcal endocarditis 1998 Endocarditis Working Group of the International Society for Chemotherapy, Europe Antibiotic treatment of infective endocarditis due to viridans streptococci, enterococci, and other streptococci; recommendations for surgical treatment of endocarditis 2000 Jennifer Li, USA Updated and modified Duke criteria 2002 Beverley C. Millar, UK Modified Duke criteria to include a molecular diagnosis of causal agents 2001– 2003 Didier Raoult, France Described etiology of Bartonella spp., Tropheryma whipplei, and Coxiella burnetii in endocarditis HACEK, Haemophilus aphrophilus, Actinobacillus actinomycetemcomitans, Cardiobacterium hominis, Eikenella corrodens, Kingella kingae group, Bartonella spp., and Coxiella burnetii. MODIFIED DUKE CRITERIA Definite endocarditis Histologic and/or microbiologic evidence of infection at surgery or autopsy OR 2 major criteria 1 major criterion and 3 minor criteria 5 minor criteria Possible endocarditis 1 major criterion and 1 minor criterion or 3 minor criteria • Blood Culture-Negative Endocarditis in a Reference Center: Etiologic Diagnosis of 348 Cases [Houpikian P and Raoult D Medicine 2005;84:162]: • This is a report from the French National Reference Center for Rickettsial Diseases for their experience with culture-negative endocarditis for the 18 year period of 1983 to 2001. Referring physicians were asked to complete a questionnaire and the following were conducted: blood serology, blood cultures, and valve culture and PCR if removed. Patients/specimens were obtained from a variety of sources in France and other countries. The criteria used for endocarditis were the modified Duke criteria. Of the 348 cases, there were 167 (48%) attributed to C. burnetii and 99 (28%) were attributed to Bartonella and 5 (1%) were attributed to rare fastidious agents such as T. whipplei, Mycoplasma hominis, Abiotrophia elegans and Mycoplasma hominis. The results for C. burnetii and Bartonella are summarized in the following table which defines the source of specimens that implicated these two agents. C. burnetii n = 167Bartonella n = 99Serology16799Blood culture1710Valve culture4415Valve PCR4147 • • • • : Circulation. 2005 Mar 22;111(11):1352-4. Impact of a molecular approach to improve the microbiological diagnosis of infective heart valve endocarditis. Breitkopf C, Hammel D, Scheld HH, Peters G, Becker K. Institute of Medical Microbiology, University of Munster Hospital, Munster, Germany. BACKGROUND: Even today, infective endocarditis (IE) remains a severe and potentially fatal disease demanding sophisticated diagnostic strategies for detection of the causative microorganisms. Despite the use of appropriate laboratory techniques, classic microbiological diagnostics are characterized by a high rate of negative results. METHODS AND RESULTS: Broad-range polymerase chain reaction (PCR) targeting bacterial and fungal rDNA followed by direct sequencing was applied to excised heart valves (n=52) collected from 51 patients with suspected infectious endocarditis and from 16 patients without any signs of IE during an 18-month period. The sensitivity, specificity, and the positive and negative predictive values for the bacterial broad-range PCR were 41.2%, 100.0%, 100.0%, and 34.8%, respectively, compared with 7.8%, 93.7%, 80.0%, and 24.2% for culture and 11.8%, 100.0%, 100.0%, and 26.2% for Gram staining. Without exception, database analyses allowed identification up to the (sub)species level comprising streptococcal (n=13), staphylococcal (n=4), enterococcal (n=2), and other signature sequences such as Bartonella quintana and Nocardia paucivorans. Fungal ribosomal sequences were not amplified. All valve tissues of the reference group were negative for both PCR and conventional methods, except one sample that was contaminated by molds. CONCLUSIONS: Culture-independent molecular methods substantially improve the diagnostic outcome of microbiological examination of excised heart valves. Importantly, this was true not only for fastidious, slow-growing, and/or nonculturable microorganisms but also for easy-to-culture pathogens such as streptococci and staphylococci. Both patient management and empiric antibiotic therapy of IE are likely to benefit from improved knowledge of the spectrum of pathogens now causing IE.