Unit 5 Notes
advertisement

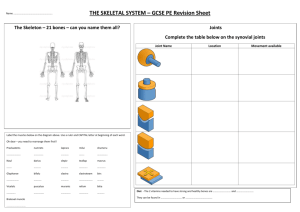
Unit 5 Bones Some Bone Facts… • One of the hardest and strongest materials in body, but very light in weight • Calcium helps to make your bones hard, and collagen fibers help to make your bones slightly flexible • Smallest bone is in the middle ear, Largest bone is the femur (thigh bone) • Comprises approximately 20% of body weight (varies) • 206 total bones as an adult; 80 axial and 126 appendicular Differences between Males & Females… • Male – – Heavier, larger – More defined markings (such as eyebrow, jaw) – Deep pelvis • Female – Lighter, smaller – Less defined markings – Flatter, wider pelvis to allow for childbirth Let’s start off by talking about bones on a tissue-level… The 3 Types of Bone Cells • Osteoblast: bone-forming cell – Uses calcium from blood and forms collagen fibers to build bone tissue • Osteoclast: bone-destroying cell – Breaks down bone matrix for remodeling using acids and enzymes, releases calcium into blood – Regulated by several hormones, including parathyroid hormone (PTH) from the parathyroid gland, calcitonin from the thyroid gland, and growth factor interleukin-6 • Osteocyte: mature bone cell 2 Types of Bone Tissue • Compact Bone – Homogeneous, dense, smooth – Composed of regular, repeating patterns – Has several major components… Parts of Compact Bone Tissue • Lacunae – Cavities containing bone cells (osteocytes) – Arranged in concentric rings • Lamellae – Rings around the central canal – Sites of lacunae • Canaliculi – Tiny canals – Connect lacuna (holding osteocytes) to central canal – Form a transport system Parts of Compact Bone Tissue • Osteon – One system of lamella rings • Haversian (Central) Canals – Canal found at center of osteon – Run parallel to bone – Carries blood vessels and nerves through the bone • Volkmann’s (Transverse/Perforating) Canals – Connect Haversian Canals perpendicular to bone 2 Types of Bone Tissue • Spongy Bone (sometimes called Trabecular bone) – Has very similar structures to Compact Bone, but is not in set, dense pattern – Much lighter, but still strong – Has needle-like pieces and empty space in bone 2 Major Sections of Long Bone • Diaphysis • Epiphysis 2 Major Sections of Long Bone • Diaphysis – Long Shaft – Made of mostly compact bone – Periosteum membrane (dense connective tissue) covers the outside; contains blood vessels, some nerve endings, osteoblasts, and osteoclasts – Sharpey’s fibers hold Periosteum to the outer diaphysis – Has inner Medullary cavity filled with fat tissue (Yellow Marrow); helps lighten the bone – Endosteum separates Diaphysis and Medullary cavity, contains osteoblasts & osteoclasts 2 Major Sections of Long Bone • Epiphysis – Ends of long bone – Composed mainly of spongy bone covered with a thin layer of compact bone – Entire epiphysis covered by articular (hyaline) cartilage, which provides smooth surface for movement – In adults, red marrow can be found here (blood cells made from red marrow through hematopoiesis) 2 Major Sections of Long Bone • Diaphysis and Epiphysis separated by epiphyseal line (which was once the epiphyseal or growth plate in young children) Bone Remodeling • Bone remodeling is a process that involves bone deposit and removal (resorption) • Remodeling units are clusters of adjacent osteoblasts and osteoclast • In healthy adult, total bone mass remains constant (meaning that deposits and removals are happening at an equal rate) • Bone remodeling occurs at a rate of 10% per year • Both happen in the adult on the periosteum and endosteum surface • Two control loops regulate bone remodeling… Bone Remodeling • Hormonal Mechanism: Calcium levels in blood – If blood needs Ca+2, parathyroid hormone (PTH) gets released to stimulate osteoclasts, which will destroy bone to release more Ca+2 – If blood has too much Ca+2, calcitonin released by thyroid gland to stimulate calcium deposited back in bone • Mechanical Mechanism: pull of gravity and muscles – Bones need to strengthen in areas where bulky muscles attached and stress is felt – Called Appositional Growth – Bones become wider (but not thicker!) due to osteoclast and osteoblast activity • http://highered.mcgrawhill.com/sites/0072495855/student_view0/ chapter6/animation__bone_growth_in_wid th.html • http://highered.mcgrawhill.com/sites/0072495855/student_view0/ chapter6/animation__osteoporosis.html How do bones change with age? • Fetus – Skeleton mostly hyaline cartilage – Has approximately 300 cartilage “bones”, many which fuse together How do bones change with age? • Before Birth / Young Child (ages 0 to 3) – Bones develop using hyaline cartilage as “model” – Ossification: Bone formation • First, hyaline cartilage covered with bone matrix by osteoblasts • Second, enclosed hyaline cartilage is digested away, leaving medullary cavity – Medullary cavity filled with Red Marrow (for Red Blood Cell production) How do Bones change with age? • Child (ages 3 – 18) – Epiphyseal plate (still made of cartilage, between diaphysis and epiphysis) provides base for length growth – Medullary cavity changes from Red Marrow to Yellow Marrow – Hyaline cartilage remains in isolated areas (bridge of nose, ribs, joints) – More bone is made than lost • Adult (ages 18-50, can vary) – Epiphyseal plate cartilage hardens and turns to bone… now known as epiphyseal line – Bone created and destroyed at fairly equal rates (bone remodeling) – Bone still changing constantly in response to body changes Newborn 1 Year 13 Years 18 years How do Bones change with age? • Elderly (ages 50 to ??) – More bone is lost than is made Trabeculae in normal bone x40 Trabeculae in osteoporotic bone x40 How do bones repair themselves? • If a fracture occurs, there are some main steps that a bone takes to repair itself – Hematoma (blood-filled swelling) forms due to ruptured blood vessels in blood – Fibrocartilage callus forms, acting as a splint – Bony callus forms as osteoblasts and osteoclasts replace fibrocartilage with spongy bone – Bone remodels in response to normal stresses, forming a permanent patch Fractures • Closed (Simple) Fracture: bone breaks cleanly but does not penetrate the skin • Open (Compound)Fracture: broken bone ends penetrate through the skin Fractures • Reduction: setting the fracture back into place – Closed Reduction: bone ends are coaxed back into position by the physician’s hand – Open Reduction: surgery is performed, and the bone ends are secured with pins or wires – After bone reduced, bone immobilized with a cast for 6 to 8 weeks Types of Fractures • Transverse: Cuts directly across the bone • Oblique: Cuts at an angle across the bone • Linear: often called a “hairline” fracture, does not displace the bone Fracture Types… • • • Comminuted: Bone breaks into many fragments, common in elderly Compression: bone is crushed, common in porous bones Depression: Broken bone portion is pressed inward, typical of skull fracture Comminuted Fracture Compression Fracture Depression Fracture Fracture Types… • Impacted: broken bone ends are forced into each other, common in falls • Spiral: ragged break due to excessive twisting, common sports fracture • Greenstick: bone breaks incompletely, common in children Impacted Fracture Spiral Fracture Greenstick Fracture Joints • The Function of Joints… – Hold bones together securely – Give the rigid skeleton mobility • Can be classified functionally or structurally… Joints • Functional Classification… dependent on how the joint moves – Synarthroses – immovable joints – Amphiarthroses – slightly moveable joints – Diarthroses – freely moveable joints – Immovable and slightly moveable joints more common in axial skeleton, while freely moveable joints more common in the limbs Joints • Structural Classification… dependent on which thing separates the bony regions at the joint! – Fibrous: separated by dense (fibrous) connective tissue • Ex: Sutures of the Skull • Usually immovable = synarthroses Joints • Cartilaginous: separated by fibrocartilage – Ex: vertebrae, pubic symphysis – Usually slightly moveable = amphiarthroses Joints • Synovial: separated by fluid-filled sac • Remember synovial membranes from the last unit??? • Usually freely moveable = diarthroses Joints • Distinguishing Features of Synovial Joint – Articular cartilage (hyaline cartilage) covers the ends of bones – Joint surfaces are enclosed by synovial membrane and a fibrous capsule – Have a joint cavity filled with synovial fluid – lubricates the joint – Ligaments reinforce the joint Joints • Types of Synovial Joints Include… – Plane Joint • Movement Allowed: slipping or gliding • Example: intercarpal joints of wrist • Non-Axial – Hinge Joint • Movement Allowed: angular movement in one plane • Example: elbow, phalanges • Uni-Axial Joints – Pivot Joint • Movement Allowed: rotates around long axis • Example: radioulnar joint • Uni-axial Skeletal System – Condyloid Joint • Movement Allowed: side-to-side and back & forth, cannot rotate around long axis • Example: knuckles • Bi-axial – Saddle Joint • Movement Allowed: same as condyloid • Example: thumb • Bi-axial Skeletal System – Ball and Socket Joint • Movement Allowed: rotation, most freely moving • Example: shoulder and hip • Multi-axial A few famous Synovial Joints… • Temporomandibular Joint – Where mandible and temporal bone meet – Problems with this joint leads to jaw issues (popping, pain when chewing, difficulty opening mouth, headaches) – Gliding and Hinge joint A few famous Synovial Joints… • Coxal Joint (Acetabulofemoral Joint) – Occurs where the head of the femur fits into the acetablum of the coxal bone – With age, this joint can become very worn down or broken at the neck of the femur, requiring a hip replacement – Ball and Socket Joint A few famous Synovial Joints… • Knee Joint (Tibiofemoral Joint) – Kneecap held on by a patellar ligament – Joint Cavity contains two cartilages – the lateral meniscus and the medial meniscus – The knee is held together using SEVERAL ligaments – Hinge and Pivot Joint Joints • Shoulder Joint (Humeroscapular joint) – The humerus and the glenoid fossa of the scapula are joined – The shoulder is held together using SEVERAL ligaments – Rotator cuff muscles also help to hold this joint in place – Ball and Socket Joint The Skull • Consists of the cranium and the bones of the face – The cranium encloses cranial cavity, protects the brain – Facial bones surround and protect the entrances to the respiratory and digestive tracts, provides attachment points for muscles to show feeling Facial Bones • • • • • Maxillary bones Mandible Palatine bones Nasal bones Vomer • Inferior nasal conchae • Zygomatic bones • Lacrimal bones • Hyoid Cranial Bones • one occipital bone • two temporal bones – foramen magnum • auditory ossicles • two parietal bones • one frontal bone – frontal sinuses • one sphenoid • one ethmoid Skull Sutures • Lamboid: separate Occipital and Parietal • Sagittal: separate Parietals • Squamous: separate Temporal and Parietal • Coronal: separate Frontal and Parietal Skull Sutures Figure 7.3a, b Paranasal Sinuses • Hollow portions of bones surrounding the nasal cavity • Functions of paranasal sinuses: • Lighten the skull • Give resonance and amplification to voice Mandible Hyoid Bone • The only bone that does not articulate with another bone • Anchors using ligaments to the Temporal bone • Serves as a moveable base for the tongue Foramen Magnum • Hole in the Occipital bone that provides passageway for the spinal cord Special Characteristics of the Fetal Skull • Infant’s face small in comparison to cranium • Skull large in comparison to infant’s body • Skeleton unfinished; has areas of hyaline cartilage that must be converted to bone • Fontanels: fibrous membranes between cranial bones that allow fetal skull to be compressed during birth, allow brain to grow This is a joint between: the lower end (1) and medial malleolus (2) of the tibia and the lateral malleolus (3) of the fibula and the trochlear surface of the talus (4) 3-5 weeks in utero. cartilage model 6 weeks in utero. Primary centre of ossification appears in shaft which is surrounded by a collar of compact bone. 2-5 years. Bone marrow cavity is formed in the shaft and secondary centres of ossification are present in the ends of the bone. Adult. Adult bone. Epiphyseal plates are closed and growth is finished. 8 months in utero - birth. Bone shaft is now fully ossified.