File - The Free Clinic
advertisement
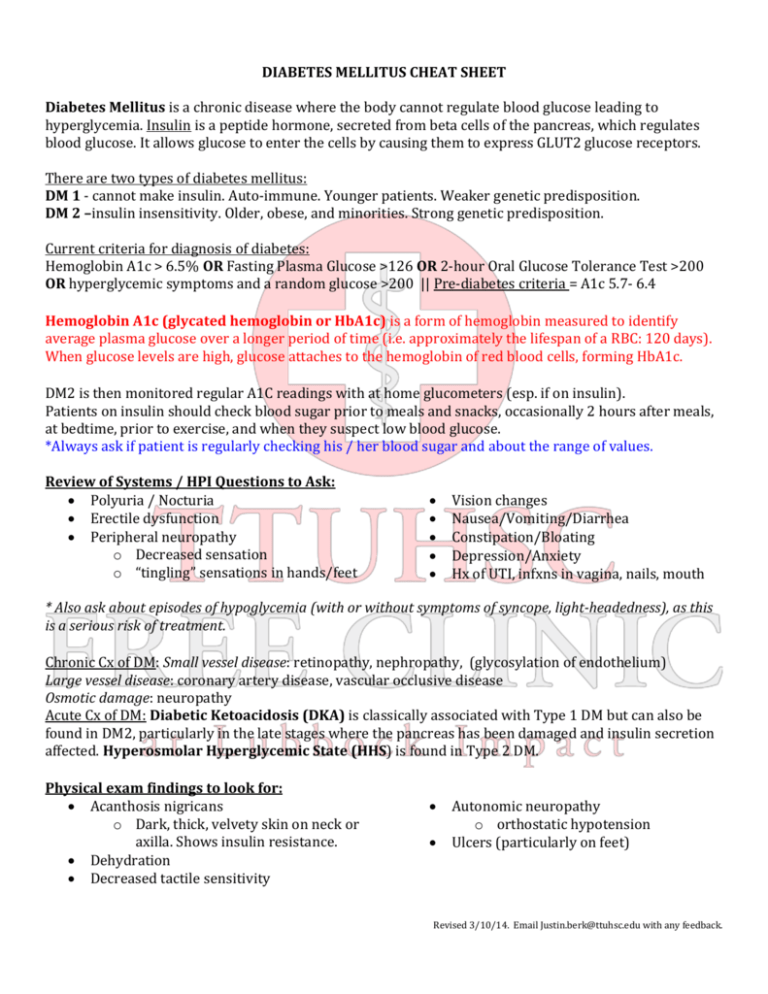
DIABETES MELLITUS CHEAT SHEET Diabetes Mellitus is a chronic disease where the body cannot regulate blood glucose leading to hyperglycemia. Insulin is a peptide hormone, secreted from beta cells of the pancreas, which regulates blood glucose. It allows glucose to enter the cells by causing them to express GLUT2 glucose receptors. There are two types of diabetes mellitus: DM 1 - cannot make insulin. Auto-immune. Younger patients. Weaker genetic predisposition. DM 2 –insulin insensitivity. Older, obese, and minorities. Strong genetic predisposition. Current criteria for diagnosis of diabetes: Hemoglobin A1c > 6.5% OR Fasting Plasma Glucose >126 OR 2-hour Oral Glucose Tolerance Test >200 OR hyperglycemic symptoms and a random glucose >200 || Pre-diabetes criteria = A1c 5.7- 6.4 Hemoglobin A1c (glycated hemoglobin or HbA1c) is a form of hemoglobin measured to identify average plasma glucose over a longer period of time (i.e. approximately the lifespan of a RBC: 120 days). When glucose levels are high, glucose attaches to the hemoglobin of red blood cells, forming HbA1c. DM2 is then monitored regular A1C readings with at home glucometers (esp. if on insulin). Patients on insulin should check blood sugar prior to meals and snacks, occasionally 2 hours after meals, at bedtime, prior to exercise, and when they suspect low blood glucose. *Always ask if patient is regularly checking his / her blood sugar and about the range of values. Review of Systems / HPI Questions to Ask: Polyuria / Nocturia Erectile dysfunction Peripheral neuropathy o Decreased sensation o “tingling” sensations in hands/feet Vision changes Nausea/Vomiting/Diarrhea Constipation/Bloating Depression/Anxiety Hx of UTI, infxns in vagina, nails, mouth * Also ask about episodes of hypoglycemia (with or without symptoms of syncope, light-headedness), as this is a serious risk of treatment. Chronic Cx of DM: Small vessel disease: retinopathy, nephropathy, (glycosylation of endothelium) Large vessel disease: coronary artery disease, vascular occlusive disease Osmotic damage: neuropathy Acute Cx of DM: Diabetic Ketoacidosis (DKA) is classically associated with Type 1 DM but can also be found in DM2, particularly in the late stages where the pancreas has been damaged and insulin secretion affected. Hyperosmolar Hyperglycemic State (HHS) is found in Type 2 DM. Physical exam findings to look for: Acanthosis nigricans o Dark, thick, velvety skin on neck or axilla. Shows insulin resistance. Dehydration Decreased tactile sensitivity Autonomic neuropathy o orthostatic hypotension Ulcers (particularly on feet) Revised 3/10/14. Email Justin.berk@ttuhsc.edu with any feedback. Labs to Order - Microalbumin annually - A1C every 3 months / every 6 months if at goal - Creatinine (iStat BMP) annually - Lipid panel annually Can also consider: TSH, CMP. Annual eye exam by ophthalmologist is recommended. Treatment: Goal A1c: <7% using a combination of lifestyle modification, oral therapy (DM2), and insulin. LIFESTYLE MODIFICATION Nutrition: Decrease carbohydrate intake, sugar-sweetened beverage cessation Exercise: 150 minutes / week of moderate aerobic exercise Education: Smoking cessation, regular foot care Rec’d Vaccinations: Pneumococcus (one time), Influenza (annually), Hep B (if unvaccinated) PHARMACOTHERAPY DM1: Insulin DM2: 1st line: Metformin | 2nd line: Add second oral agent | 3rd line: third oral or insulin If urine microalbumin lab is positive, begin ACE-Inhibitor to protect from further diabetic nephropathy DRUG Biguanides EXAMPLE Metformin MECHANISM hepatic gluconeogenesis NOTE C/I: kidney dysfunction SE: N/V/D, lactic acidosis (rare) Glipizide, Glyburide, Glimepiride Insulin secretion Sulfonylurea (blocks K+ efflux -> increased Ca+ SE: hypoglycemia influx -> insulin granule release) Thiazolidinediones Activate PPAR nuclear receptors -> SE: weight gain, Pioglitazone (TZDs) insulin sensitivity hepatotoxicity *Drugs in red = available in Free Clinic. **C/I = contra-indications. SE = common side effects. Other DM drugs to know about and their side effects: GLP-1 analogs (Exenatide)- bloating/pancreatitis DDP-4 inhibitors (Sitagliptin) – pancreatitis α-glucosidase inhibitors (Acarbose)– abd. gas SLGT2 inhibitors (canaglifozin) Injectable Insulin (indicated for DM1 or uncontrolled DM2) – look out for hypoglycemia TYPE EXAMPLE ONSET OF ACTION DURATION OF ACTION Rapid Lispro, aspart, glulisine 5-15 minutes 3-6 hours Short Regular (R)* 1-2 hours 6-10 hours Intermediate isophane (NPH or N) 1-2 hours 10-20 hours Long Glargine (Lantus), levemir 1-2 hours 24 hours Mixed 70% NPH / 30% regular * 2 brands of insulin available: Humulin and Novolin Insulin treatments can be managed in several modalities including sliding scale, pre-prandial, and mixed. “Carb counting” is a technique that can be taught to help patients with pre-prandial insulin dosing. Both DM1 and DM2 patients require a basal rate of insulin. DM1 patients also require post-prandial coverage. Revised 3/10/14. Email Justin.berk@ttuhsc.edu with any feedback.






