Epithelial Ovarian Carcinoma
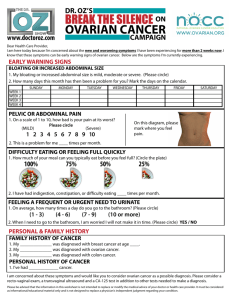
advertisement

Epithelial Ovarian Carcinoma 高雄榮總婦產科 劉文雄醫師 Introduction Malignant neoplasms of the ovary present an increasing challenge to the physician. They are the cause of more deaths than any other female genital tract cancer. It accounts for 5% of all cancers among women. In U.S, deaths from this cause occur at a rate of one every 45 min, and one in every 56 women will develop this disease. Classification The early development of the ovary may be divided into four major stages : During the first stage, undifferentiated germ cells (primordial germ cells) become segregated and migrate from their sites of origin to settle in the genital ridges. The second stage occurs after arrival of the germ cells in the genital ridges and consists of proliferation of the coelomic epithelial and the underlying mesenchyme. During the third stage, the ovary becomes divided into a peripheral cortex and a central medulla. The fourth stage is characterized by the development of the cortex and involution of the medulla. Relative Frequency of Ovarian neoplasms Type Coelomic epithelial Germ cell Specialized gonadal stroma Nonspecific mesenchyme Metastatic tumor % 50-70 15-20 5-10 5-10 5-10 Classification The majority(85 to 90% ) of malignant ovarian tumors seen in the US are epithelial. Serous cystadenocarcinoma :42% Mucinous cystadenocarcinoma : 12% Endometrioid carcinoam : 15% Undifferentiated carcinoma : 17% Clear cell carcinoma : 6% Incidence, Epidemiology, and Etiology Approximately 23 % of gynecologic cancers are of ovarian origin, but 47% of all deaths from cancer of the female genital tract occur in women who have gynecologic cancer of ovarian cancer. Approximately 12 of every 1000 women in the US older than 40 years will develop ovarian cancer, but only 2 or 3 of the 12 will be cured. Incidence, Epidemiology, and Etiology Malignant germ cell tumors are most commonly seen in females younger than 20 years, whereas epithelial cancers of the ovary are primarily seen in women older than 50 years. Incidence rate of ovarian cancer related to age : 40-44 yr : 15.7/100000. 50-60 yr : 35/100000. 75-79 yr : 54/100000. More than one third of the cases occur in patients 65 yrs or older Primary ovarian neoplasm related to age Type Up to 20 yr Coelomic epithelium Germ cell Specialized gonadal stroma Nonspecific mesenchyme 20-50 yr Over 50 yr 29% 59% 8% 71% 14% 5% 81% 6% 4% 4% 10% 9% Familial Ovarian Cancer Several reports describe families in which girls and women of the same or succeeding generations develop similar neoplasms of the ovaries. Most of these neoplasms were serous carcinomas. Cancers of the breasts, colon,and other sites were also found more commonly in female members of these afflicted families. NCI studies disclosed the number of relatives with ovarian cancer was significantly higher ( relative risk : 2.61) than the control. Familial Ovarian Cancer The lifetime risk for ovarian cancer in the population as a whole is approximately 1.4% ; with one first-degree relative, it is 5% ; with two or more first-degree relatives, it rises to 7%. Among the later group, there is 3% chance of having hereditary ovarian cancer syndrome; in those families, the lifetime risk of ovarian cancer is at least 40%. Firm guidelines for prophylactic oophorectomy have not been established. Lifetime probability of ovarian cancer by age in women with one relative with ovarian cancer Age(year) 30 35 40 45 50 55 60 Lifetime probability lifetime probability of of ovarian Ca (%) ovarian ca with one relative(%) 1.6 1.6 1.6 1.5 1.4 1.3 1.2 5 5 4.8 4.5 4.4 4.1 3.6 Familial Ovarian Cancer Three different hereditary syndromes of cancer have been identified : All three syndrome have a pattern of earlyonset cancer and vertical transmission consistent with autosomal dominant inheritance. The first is a site-specific familial ovarian cancer syndrome : women are at high risk for the development of ovarian carcinoma only. The second is a breast-ovarian cancer syndrome : 50% risk of ovarian carcinoma if their mothers or sisters had breast and/ or ovarian carcinoma. The syndrome have been associated with the BRCA-1 and BRCA-2 gene. Familial Ovarian Cancer The third is the cancer family syndrome in which both males and females are at increased risk of acquiring colon cancer, and to a lesser extent other cancers, including gastric carcinoma, thyroid carcinoma, and sarcoma. Most of the colon cancers are in the proximal colon and not easily diagnosed. Women in these families are at increased risk for carcinoam of the ovary, endometrium, and breast. Familial Ovarian Cancer Because of the AD inheritance pattern, 50 % risk can be predicted in all offspring and siblings of inflicted individuals. Prophylactic oophorectomy as soon as childbearing is completed ? Most of the cancers have been detected in women between 35 to 45 yrs; thus, if oophorectomy not done, biannual sonogram with PV plus CA-125 should be advised. Even the prophylactic oophorectomy was done; safety? Familial Ovarian Cancer It is important to distinguish women in families with hereditary ovarian cancer syndromes from those who have family members with ovarian cancer. Thorough medical history : a woman’s family history of ovarian cancer, breast cancer, endometrial cancer, and non- polyposis colorectal cancer. Determining the age of occurrence of these cancers in the family members. Family pedigree by a physician to identify the AD inheritance pattern. Familial Ovarian Cancer Suggest for these patients : Should be maintain by oral pills until such time that they desire childbearing. Patients less than 35 yrs with a history of hereditary ovarian cancer syndrome should be monitored with a PV + sonogram + CA-125 every 6 months. At the age of 35, prophylactic oophorectomy may be elective. How oral pills use affects the risk of ovarian cancer Duration of oral No. of women who pills use developed ovarian Ca Never 3-6 months 7-11 months 1-2 years 3-4 years 5-9 years >10 years 242 26 14 65 40 39 13 Controls Relative risk 1532 280 134 602 397 594 328 1.0 0.6 0.7 0.7 0.6 0.4 0.2 Etiology of Ovarian Cancer Environmental factors : physical and chemical products of industry are major causes of epithelial neoplasms. Theory of “ incessant ovulation” suggests that the epithelial lining of the ovary may be sensitive to the constant trauma of ovulation, which in turn can act as a promoting factor in the carcinogenic process. Prolonged use of fertility drugs such as Clomid may increase the risk of borderline and invasive ovarian cancer. Etiology of Ovarian Cancer Others have suggested that ovarian cancer may be initiated by a chemical carcinogen via the vagina, uterus, and fallopian tubes, and the substances promoting cancer may even be the steroid- rich antral fluid from ruptured follicles. Genital exposure to Talc : 42% Vs 28%. No evidence exists to incriminate viruses in the development of neoplasms of the human ovary. Most frequent presenting symptoms of ovarian cancer Symptom Relative frequency Abdominal swelling Abdominal pain Dyspepsia Urinary frequency Weight change XXXX XXX XX XX X Nonovarian etiology of adnexal mass Frequently encountered nonovarian causes of apparent adnexal masses : Diverticulitis. TOA. Carcinoma of cecum or sigmoid. Pelvic kidney. Uterine or intraligamentous myomas Ovarian Cancer Screening Periodic pelvic examination, ultrasonography, CA-125. 10000 PV would be required to pick up one early ovarian cancer in an asymptomatic patient population. CA-125 as a screening technique has not been rewarding especially in premenopausal women. Many conditions of a benign nature as well as most GI malignancies, may elevated the CA-125. Ultrasonography, especially the TVS ( color doppler ). Scroing System for Ovarian TumorMorphologic Index DePriest PD, Shenson D, Fried A, Hunter J, Andrews S, Gallion H, et al. A morphology index based on sonographic findings in ovarian cancer. Gynecol Oncol 1993;51:7-11. Scroing System for Ovarian TumorMorphologic Index Doppler Study In Doppler velocimetry, the flow velocity waveform obtained from a target vessel is evaluated according to standard parameters, pulsatility index (PI) and resistant index (RI). The vessels supplying benign ovarian tumors generally were peripheral in location, had high systolic flow, and a high PI (>1.0) and RI (>0.4). In contrast, vessels supplying ovarian malignancies generally had significant diastolic flow, were centrally located, and had a low PI (<1.0) and RI (<0.4). It is difficult to clearly identify ovarian malignancies on the basis of pulsed Doppler findings alone. CA-125 An ideal marker should have high sensitivity (few falsenegative results), high specificity (few false-positive results), and high accuracy. Serum levels of CA 125 are elevated (>35 u/mL) in approximately 50% of patients with stage I epithelial ovarian cancer and in more than 90% of those with advanced disease. Generally, serum CA 125 values rise over time in patients with ovarian cancer, whereas they remain stable or decrease in patients with benign ovarian tumors. Therefore, serial CA 125 determinations at 2 to 4-week intervals can be helpful in deciding whether a sonographically confirmed ovarian tumor can be monitored safely or should be removed surgically. CA-125 With advances in molecular technology, a number of candidate tumor markers for ovarian cancer have been identified including CA 15.3, CA 72.4, CA 19.9, and soluble epidermal growth factor. At present, however, there is little evidence to suggest that their use in a multimodality screening panel is superior to CA 125 alone in differentiating benign from malignant ovarian tumors. Proteomics Proteomic profiling of serum using mass spectroscopy (surface-enhanced laser desorption and ionization) has been proposed recently as a method to detect ovarian cancer. Basically, a population of proteins can be profiled according to the size and net electrical charge of the individual proteins. The discriminating proteomic pattern formed by a subset of proteins is defined by peak amplitude at key mass/charge positions along the spectrum. Ovarian Cancer Screening Improve the effectiveness of ovarian cancer screening would be to target populations at increased risk of the development of the disease, such as individuals, with a positive family history of ovarian cancer. Another strategy to improve sensitivity and specificity in screening for ovarian cancer involves the use of multiple serum tumor markers. Because less than 50% of patients with stage I ovarian cancer will have an elevated CA-125. Management Guideline Non-malignant conditions that may elevate CA125 concentrations Nongynecologic Gynecologic Active hepatitis Acute PID Acute pancreatitis Adenomyosis Cirrhosis Benign ovarian neoplasm Congestive heart failure Endometriosis DM(poor control) Functional ovarian cyst Diverticulitis Meig’s syndrome Mesothelioma Menstruation Nonmalignant ascites OHSS pericarditis Unexplained infertility Pneumonia Uterine myoma Post-op period SLE Pattern of Spread Transcelomic : The most common and earliest mode of dissemination is by exfoliation of cells than implant along the surfaces of the peritoneal cavity. Lymphatic : retroperitoneal ( pelvic and paraaortic ) LN spreading is common in advanced- stage disease. 78% with stage III disease had positive pelvic LN. And the rate of the positive paraaortic LNs was 18% in stage I , 20% in stage II, 42% in stage III, and 67% in stage IV. Hematogenous : is uncommon at the time of diagnosis, lungs and liver is the most common sites Diagnostic Techniques Pelvic examination remains the most practical means of detecting early disease. Pain is usually a late complication. Any ovary palpated in a patient 3 or more years after menopause should raise a high index of suspicious of an early ovarian neoplasm. Diagnostic paracentesis is a patients with ascites and a pelvic-abdominal mass is unnecessary and dangerous. Diagnostic Techniques Ovarian cancer is classically a serosal spreading disease, and thus all peritoneal surfaces must be carefully inspected, especially when disease is thought to limited to the pelvis. Washing cytology : 1. subdiaphragm, bil . 2. Paracolic gutter, bil. 3. Cul-de-sac . Care should be taken to visualize and palpate all peritoneal surfaces including the underside of the daiphragm, the surface of the liver and the small and large bowel mesentary. Complete Workup For Ovarian Cancer Careful history Physical examination Pelvic examination and Pap’s smear Proctosigmoidoscopy, where indicated CBC and urinalysis Blood chemistries, including CA-125 Chest film, IVP, Barium enema, or CT scan Pelvic sonogram. Surgical Therapy in Ovarian Cancer Peritoneal cytologic examination Determination of extent of disease Pelvis Peritoneal surface Diaphragms Omentum Lymph node Removal of all tumor possible Guidelines For Staging in Epithelial Ovarian Cancer 4 peritoneal washings ( diaphragm, bil paracolic gutter and cul-de-sac ). Careful inspection and palpation of all peritoneal surfaces Biopsy of smear from undersurface of bil diaphragm. Biopsy of all suspicious lesions . Infracolic omentectomy. Biopsy or resection of any adhesions Random biopsy of normal peritoneum of bladder reflection cul-de-sac, Rt and Lt paracolic gutters and both pelvic side walls. Selected lymphadenectomy of pelvic and para-aortic nodes. ATH,BSO, and excision of all masses where prudent Stage and 5-year Survival Stage Ia Stage Ib Stage Ic Stage IIa Stage IIb Stage IIc Stage IIIa Stage IIIb Stage IIIc Stage IV Overall 84% 79% 73% 65% 54% 61% 52% 29% 18% 14% 31% Early-Stage Ovarian Cancer Early-stage ovarian cancer: I-IIa The primary treatment for early stage epithelial ovarian cancer is surgical, that is, a ATH+BSO+ complete surgical staging. (24% will be upstaging to stage III) Based on the prognostic variables, early stage epithelial ovarian cancer can be subdivided into low-risk and highrisk disease. The uterus and the contralateral ovary can be preserved in women with stage IA , low-risk disease who wish to preserve fertility. Zanetta et al. BJOG,1997; Favalli et al. Int J Gyn Cancer, 2001 Prognostic Variables in Early-stage Epithelial Ovarian Cancer Low risk Low grade Non-clear cell histologic type Intact capsule No surface excrescences No ascites Negative peritoneal washing Unruptured or intraoperative rupture No dense adhesion Diploid tumor High risk High grade Clear cell type Tumor growth through capsule Surface excrescences Ascites Malignant cells in fluid Preoperative rupture Dense adhesion Aneuploid tumor Early-Stage Low-Risk Ovarian Cancer Stage IA, IB, Grade 1 and 2. GOG randomized trial of observation versus melphalan in this group of patients and the 5-year survival for each group were 94% and 96%. No further adjuvant treatment is needed for such patients. Early-Stage High-Risk Ovarian Cancer In patients whose disease is high risk ( e.g., more poorly differentiated or in whom there are malignant cells either in ascitic fluid or in peritoneal washings ) . Additional therapy in indicated. Treatment options include chemotherapy or wholeabdominal radiation Randomized Trials in Stage I Epithelial Ovarian Cancer ( since 1995) Author Young et al GOG7601 GOG7602 Bolis et al. Stages Treatment Best Arm 81 141 47 104 I(Low) I(High), II I(Low) I(High) Observation Vs. Melphalan P32 Vs melphalan Observation Vs cisplatinx6 P32 Vs cisplatinx6 Young et al. 205 GOG95 Trope et al 134 Closed/maturing GOG172 331 I(High), II Cisplatin75mg/m2/ cyclo 750mg/m2 Vs P32 Carboplatin vs. observation NP NP NP Cisplatin 79 Vs 69% Cis/cyclo 77 Vs 66% NP Ongoing Trial GOG175 Patients I(High) I(High), II Taxol 175 mg/m2/ carbo AUC 7.5 (3 vs 6 courses) I(high), II Taxol 175mg/m2/carbo AUC 6 followed by observation vs. Taxol 40mg/m2/weeklyx26wks Early-Stage High-Risk Ovarian Cancer Patients with high-risk stage I epithelial ovarian cancer be given adjuvant chemotherapy. The type depends on the patient’s overall health and status. Treatment with carboplatin and Taxol chemotherapy for 3 to 6 cycles seem desirable in most patients, whereas a short course of a single agent, either carboplatin or Taxol, may be preferable for older women. Advanced-Stage Ovarian Cancer After the introduction of cisplatin in the latter half of the 1970s, platinum-based combination chemotherapy became the most frequently used regimen in USA. Taxol become available in the 1980s, and this drug was incorporated into the combination chemotherapy in the 1990s. Cisplatin Combination Chemotherapy Combination chemotherapy has been shown to be superior to single-agent therapy. After cisplatin became available for the treatment of ovarian cancer showed that cisplatin was better than an alkylating agent , cyclophosphamide, as a single agent. Several studies recommended the platinum-based chemotherapy were shown to be superior. Most studies using the PC or PAC regimen, disclosed the same survival rates. Taxol-based Combination Chemotherapy The next major advance in the treatment of advanced stage disease was the incorporation of taxol into the chemotherapeutic regimen. Several prospective randomized trial with taxol-based arms have defined the current recommended protocol in advanced epithelial ovarian cancer. Based on the GOG111,1996 and OV10,1998 studies, Taxol should be included in the primary treatment of all women with advanced-stage epithelial ovarian cancer Platinum and Taxol Chemotherapy randomized Trials in Advanced-Stage epithelial Ovarian Cancer Author McGuire Year 1996 Group GOG 111 Status Subopt Stuart 1998 Opt/Subopt Muggia 1997 EORTC OV10 GOG132 Ozols 1999 GOG158 Opt Bois 1999 AGO Opt/subopt Albert 1996 GOG104 Opt Markman 1998 GOG114 Opt Subopt Drugs/doses T:135(3)/cis75 vs ctx750/cis75 T:175/cis75 vs ctx750/cis75 Cis100 vs T200(24) vs cis75/T135(24) Carbo7.5/T175(3) vs cis75/T135(24) Carbo6/T185(3) vs cis75/T185(3) Ipcis100/ctx750 vs Iv cis75/ctx750 Carbox2-9/Ip cis100 /T135(24) vs Iv cis 75/T135(24) Best Taxol/cis Taxol/cis Taxol/cis Taxol/carbo Taxol/carbo Ip cis/ctx Ip cis/carbo / Taxol Platinum and Taxol Chemotherapy randomized Trials in Advanced-Stage epithelial Ovarian Cancer-Ongoing Author Harper Group(Protocol) ICON3 Status Opt/Subopt GOG162 Subopt GOG172 Opt Drugs/Doses/(hrs) T135(24)/cis75 vs Carbo vs cis/ctx/doxo T135(24)/cis75 vs T120(96)/cis75 Iv T135(24)/Ipcis100 (D2)/Ip T60(D8) vs Iv T135(24)/Iv cis75 Chemotherapeutic Recommendation in Advanced Ovarian Cancer Combination chemotherapy with carboplatin and Taxol. The recommended doses and schedule are carboplatin ( AUC 5 to 6) and Taxol 175 mg/m2(3hrs) Q3W for 6 cycles. In patients who cannot tolerate the combination, singleagent carboplatin (AUC 5 to 6 ) can be given. In those who have a hypersensitivity to Taxol, an alternative active drug can be substituted ( e.g., cyclophosphamide or topotecan). In patients who cannot tolerate IV chemotherapy, an oral alkylating agent can be substituted. Combination Chemotherapy for Advanced Epithelial Ovarian Cancer : Recommended Regimens Drugs Dose Infusion time(hr) Interval No. of cycles Standard Regimen Taxol Carboplatin 175mg/m2 AUC 5-6 24 Q3W Q3W 6 cycles 6 cycles 135 mg/m2 75 mg/m2 3 Q3W Q3W 6 cycles 6 cycles Taxol Cisplatin Alternative Drugs( can be given with platinum ) Cyclophosphamide 600-750 mg/m2 Topotecan 1.0-1.25 mg/m2 Gemcitabin 800-1000 mg/m2 Q3W Daily x 5 D Q3W Q3W Administration of Chemotherapy and Amelioration of Toxicity Taxol : The principal concern of Taxol + Carboplatin is the patential for enhanced bone marrow toxicity. In general, 3 hrs infusion tend to reduce the likehood of bone marrow depression than 24 hrs infusion. The principal concern of Taxol + cisplatin is the potential for neurotoxicity. Administration of Chemotherapy and Amelioration of Toxicity Carboplatin : The renal and GI toxicities of carboplatin are modest compared with cisplatin, and therefore do not require prehydration and outpatient administration is more feasible. Carboplatin does tend to have appreciable bone marrow toxicity. G-CSF 250 ug/m2 given sc. From D2-14 may be protective . Administration of Chemotherapy and Amelioration of Toxicity Cisplatin : Is given Q3W by IV infusion not over 1mg/min . Required prehydration, 1/2 saline given iv at a rate of 300-500 ml/hr for 2-4 hours until the urine output is greater than 100 ml/hr . The principal toxicities of Taxol + cisplatin are renal, GI, hematologic, and neurologic. The renal and neurologic toxicities usually limit the duration of treatment to six cycles. Radiation Therapy An alternative to combination chemotherapy for selected patients with metastatic ovarian cancer is the use of whole-abdomimal radiation therapy. The treatment involves a radiation field that extends from 1 to 2 cm above the level of the diaphragm to include the entire pelvis. Whole-abdominal radiation appears useful in patients whose metastatic disease is microscopic or completely resected. No definite role in the treatment of ovarian cancer. Hormonal Therapy There is no evidence that hormonal therapy alone is appropriate primary therapy for advanced ovarian cancer. The us of progestational agents in the treatment of recurrent, well-differentiated endometrioid cancer is supported by the current data. The reported response rates by Rendina et al, is 57% (17/30) in recurrent epithelial cancer, with 10% (3/30) complete response, all responding patients had well differentiated , estrogen recepor-positive tumors. Immunotherapy Various trials using nonspecific immunostimulants to treat patients with ovarian cancers. Most frequently, agents such as corynebacterium parvum and bacillus Calmette-Guerin (BCG) have been used systemically in conjunction with cytotoxic chemotherapy. None as yet has demonstrated efficacy as primary treatment. The use of cytokines has been tested in a second-line setting, and the activity of interferon-a, interferon-r, and interleukin- 2 has been demonstrated Immunotherapy Trials of monoclonal antibodies directed toward ovarian cancer- associated antigens are being conducted. Antibodies directed toward CA125 and the human milk fat globulin (HMFG) tumor- associated antigens are underway. Herceptin, an antibody directed toward the extracellular protein produced when the HER-2/neu oncogene is overexpressed, has been used extensivelly in breast cancer. Trials of Herceptin in HER-2/neu overexpressing ovarian cancer are ongoing. Antibodies against the protein produced by the mutated P53 tumor suppressor gene are also undergoing clinical studies. Treatment Assessment Tumor Markers : CA-125 : a surface glycoprotein associated with mullerian epithelial tissue, is elevated in approximately 80% of patients with epithelial ovarian cancer, particularly those with nonmucinous tumors. The level of CA-125 have been correlated with the findings at second-look operations. Positive levels are useful in predicting the presence of disease, but negative levels are an insensitive determinant of the absence of disease. Treatment Assessment Tumor markers : Positive predictive value : 100% Negative predictive value : 56% The change in level usually correlates with response. Those patients with persistently elevated titers after three cycles of treatment most likely have resistant clones. Radiologic Assessment : The false-negative rate of a CT scan is approximately 45%. Treatment Assessment Second-look Operations : Is performed to determined the response to therapy on a patient who has clinical complete response after a prescribed course of chemotherapy. 5 sites (cul-de-sac, bil paracolic gutter & bil subdiaphragm ) cytology and biopsies of the peritoneal surface, particularly in any areas of previously documented tumor. Any adhesions or surface irregularities should be sampled. Biopsy specimens should be taken from the pelvic sidewalls, the pelvic cul-de-sac, the bladder, the paracolic gutters, the residual omentum, and the diaphragm. Treatment Assessment Second-look operation : A pelvic and paraaortic lymph node dissection should be performed in those patients whose nodal tissue have not been previously removed. Approximately, 30% of patients with no evidence of macroscopic disease have microscopic metastases. Also, in many patients with microscopic disease, it is detected only in the occasional biopsy or cytologic specimen. If gross tumor is disclosed at second-look operation, resected all the tumor tissue may be performed to faciliate response to salvage therapies. Second-Look Operation Has not been shown to influence patient survival, although the information obtained at second look is highly prognostic. The reported relapse rates after negative second-look operation is around 30-50 % at 5 years. Initial Stage : Patients whose tumors are initially stage I & II have negative second-look rates of 85-95% and 7080%. Whereas the rates for patients with stage III or IV disease is 30-45%. Second-Look Operation Tumor grade : The likelihood of a negative second look in patients at all stages is about 60%-70% for those with grade I tumors, 40-50% for those with grade II, and only 20% for those with grade III. Type of chemotherapy : In patients with optimally resected stage III disease treated with the taxol + platinum, the negative second look rate is about 45-50%. Second-look laparoscopy ? role Second-Line Chemotherapy The response rates for second-line chemotherapies have been 15 to 35% for most drugs tested by the oral or IV route. Single-agent drugs are sometimes used for second-line chemotherapy because of their relative ease of administration and low toxicity. Second-Line Chemotherapy in Recurrent/Persistant Epithelial Ovarian Cancer Drug Cisplatin Carboplatin Taxol Topotecan Etoposide Liposomal Doxorubicin Gemcitabine Holoxan Hexamethylmelamine Platinum Response Sensitive Resistant Sensitive Resistant Sensitive Resistant Sensitive Resistant Sensitive Resistant Sensitive Resistant Sensitive Resistant Both Both % Response 77% 28% 33% 19% 22% 13% 26% 13% 36% 27% 26% 15% 20% 13% 17% 27% Response/Patients 17/22 14/50 24/72 38/202 28/127 33/255 35/134 34/263 16/44 25/94 9/35 15/103 7/35 8/60 5/29 13/49