Anti-microbials
advertisement
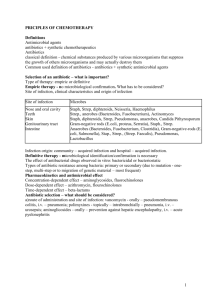
Anti-microbials By Dr.Mohamed Abd Almoneim Attia Classifications of antimicrobials A. According to their antimicrobial spectrum: *Antibiotics with narrow spectrum: Drugs primarily effective against gram-positive organisms e.g. some penicillins, cephalosporins, macrolides,…….. etc. Drugs primarily effective against gram-negative organisms e.g. aminoglycosides, monobactam, ……... *Extended spectrum: both gram –ve and +ve microorganism. *Broad-spectrum antimicrobial agents That affects most gram-positive and most gram-negative organisms and others(protozoa) e.g chloramphenicol, tetracyclines, broad-spectrum penicillins, 3rd generation cephalosporins………. B.Antimicrobial agents are also classified according to pharmacological effects as either bacteriostatic (inhibitory) or bactericidal (lethal) agents. 1-Bacterostatic (stop multiplication of microorganisms) e.g. sulfonamides, trimethoprim, chloramphenicol,…... Most of bacteriostatic drugs become bactericidal in high concentrations. 2-Bactericidal (act primarily by killing microorganism) e.g. penicillin, cephalosporins, aminoglycosides…….. C. According to the source and chemistry: 1-Synthetic Chemotherapeutic Agents: they act selectively on infective organism such as sulfonamides, isonicotinic acid hydrazide and the quinolones. 2-Antibiotics: are those compounds produced by microorganisms (bacteria, fungi) that, at high dilutions, are inhibitory or lethal to other microorganisms such as penicillin, tetracycline and chloramphenicol. D. Antimicrobial agents are also classified according to their Mechanism of action: Mechanism of action of antimicrobial agents Antimicrobials affect microbial cells by one or more of the following: 1-Inhibition of bacterial cell wall synthesis, so that the cell absorb water and bursts e.g. B lactam antimicrobials , bacitracin, cycloserine, vancomycin. 2-Increased permeability of cell membrane. So that vital metabolites escape e.g. antifungal (nystatin, amphotericin), antipseudomonas (polymyxin B, colistin). 3-Inhibition of protein synthesis by an effect on ribosome: Drugs acting on 30S subunit e.g. aminoglycosides, tetracycline. Drugs acting on 50S subunit e.g. chloramphenicol, macrolides, fucidin, lincosamides. 4-Inhibition of nucleic acid synthesis e.g. rifampicin, quinolones, metronidazole, antivirals, anticancer. 5-Inhibition of intermediary metabolism e.g. sulfonamides, trimethoprim, pyrimethamine, methotrexate. • Uses of antimicrobials:………………………………………… Adverse effects of antimicrobial agents: The adverse effects associated with the use of antimicrobial agents include: 1-Hypersensitivity or allergic reactions: In form of fever, skin rash, arthralgia, cholestatic jaundice or hemolysis. More serious reactions are agranulocytosis, bone marrow aplasia or anaphylactic reaction. 2-Resistance 3-Superinfection= (Opportunistic infection): Reactions related to alterations in normal body flora Administration of broad-spectrum antibiotics if used for long time may alter or kill bacterial flora or have incomplete absorption. So, the bacteria and fungi that are normally inhibited by bacterial flora will multiply leading to superinfection (its early manifestation may by diarrhoea). It is caused by staphylococci, Pseudomonas, proteus, Candida albicans.. etc. Superinfection may be vaginal, oral, pharyngeal or even systemic infection e.g. staphylococcal enterocolitis, candidiasis. The most serious form of superinfection if it is caused by gram+ve anaerobic organism like closterdil difficile resulting in pseudmembranous colitis. Treatment: Stop the causative agent and give drug, which kill the organisms responsible for superinfection e.g. staphylococcal enterocolitis, which is treated by vancomycin orally, or antifungal nystatin for candidiasis. If it is in the form of pseudmembranous colitis, it is treated with antianaerobic e.g. metronidazole. In addition you must give symptomatic treatment in form of adsorbants and antidiarrheal. 4-Vitamin B complex deficiency may follow the use of antimicrobials e.g broad-spectrum antibiotics. It is due to inhibition of bacterial flora that forms these vitamins. 5-Direct toxic reactions (organ toxicity), resulting from high doses or drug interactions, on hemopoietic system, liver, kidney, GIT, nervous system or CVS. Resistance to antimicrobial drugs Biochemical mechanisms: 1-Production of inactivating enzymes: e.g. -lactamases (by staph. and some gram-negative bacilli) inactivate -lactam antibiotics. 2-Reduced bacterial permeability to antibiotics: e.g tetracyclines accumulate by active transport mechanism in susceptible organisms. Resistant strains lack this mechanism. 3-Modification of the receptor site: e.g. Loss or alteration of the receptor protein on 30S ribosome causes resistance to aminoglycosides and 50S ribosome causes resistance to erythromycin. 4-Development of an alternate metabolic pathway that bypasses the reaction inhibited by the drugs: e.g. sulfonamide-resistant bacteria can utilize pre-formed folic acid. B. Genetic basis of acquired resistance: Chromosomal resistance: Extrachromosomal resistance: This results from transfer of genetic material from one bacterium to another.The genetic material may be in the form of plasmids . The genetic material and plasmids can be transferred by transformation, transduction, conjugation, or translocation. Prevention of antimacrobial resistance: 1-Choice of proper effective drug. 2-Give the proper dose for sufficient time to maintain sufficiently high levels of the drug in tissues 3-Drug combination e.g. in TB 4-Avoid unnecessary exposure of microorganism to a particularly valuable drug by restricting its use (e.g. rifampicin mainly for TB) Combinations of antimicrobials Clinical values (indications or aims) of antimicrobials combination: 1-To obtain better effect (synergism) or to increase the spectrum e.g. Sulfamethoxazole plus trimethoprim to form co-trimoxazole. clavulanic acid plus amoxicillin as clavulanic acid inhibits -lactamase. Another example is sulbactam with ampicillin Penicillin plus aminoglycoside. 2-To reduce the toxicity or incidence of adverse effects. 3-To prevent or delay the emergence of resistant strains especially in chronic infections as tuberculosis in which two or three agents are used. 4-In mixed infections as peritonitis (following colon perforation), a drug active against anaerobes and gram-positive bacteria (e.g. clindamycin) is combined with one active against gram-negative bacteria coliforms e.g aminoglycosides. 5-For emergency treatment of serious infections before laboratory studies are completed e.g. in suspected septicemia. Anti-staphylococcus (nafcillin) may be combined with a drug active against aerobic gram-negative bacilli (aminoglycosides). Results of antimicrobial combinations: Combining antimicrobial agents may result in the following: 1-Bactericidal + bactericidal results in synergism: e.g. combined use of penicillin and an aminoglycoside antibiotic (such as gentamicin) on the enterococcus. In this example, inhibition of cell wall synthesis by penicillin permits better penetration of the cell wall by the aminoglycoside and more effective inhibition of protein synthesis than either drug alone. 2-Bacteriostatic + bacteriostatic results in addition (summation): e.g. the use of tetracyclines with sulfonamides or chloramphenicol. 3-Bactericidal + bacteriostatic (antagonism): e.g. use of penicillin, with tetracyclin in group (A) streptococcal infection. This because the tetracyclines inhibit protein synthesis and are bacteriostatic. Penicillin as bactericidal affects cell wall synthesis and requires that bacteria be actively multiplying in order to be bactericidal. Disadvantages of antimicrobial combination: 1-Antagonism: This may occur if a bacteriostatic (tetracycline, chloramph-enicol) and a bactericidal (penicillin, cephalorporins, aminoglycosides) drugs are used together. 2-Increase incidence of Adverse effects and cost. 3-Efforts toward accurate diagnosis may be neglected. General principles of therapy with antimicrobials 1-Antimicrobials should only be given when necessary and after antimicrobials susceptibility test whenever possible. 2-The pharmacokinetics of the drug should be taken into consideration e.g. the state of hepatic and renal functions of the patient. 3-In serious infection it is better to start with a parentral loading of a bactericidal agent to avoid emergence of resistant strains by giving adequate dosage for sufficient duration. 4-Antimicrobials should be continued for 3 days after apparent cure is achieved to avoid relapse. 5-Bactericidal drugs should be used when there is leucopenia or the phagocytic cells can not get to the site of infection e.g. endocarditis. Causes of failure of antimicrobial therapy Drug: Inappropriate choice, in adequate duration or dose, improper route of administration, poor penetration into the site of infection. Host (patient): Poor host defenses, undrained pus (presence of dead tissue), retained foreign bodies. Pathogens: drug resistance, superinfection. SYNTHETIC ANTIMICROBIALS The synthetic chemotherapeutic agents available for clinical use include the sulfonamides, sulfones, quinolones, p-aminosalicylic acid (PAS), trimethoprim, pyrimethamine, nitrofurantoin, isoniazid and pyrazinamide. SULFONAMIDES Chemistry sulfonamides comprise a large group of compounds that are structural analogous of P-aminobenzoic acid (PABA). Pharmacokinetics Absorption and distribution: Well absorbed and distributed preparations: the best is sulphadiazine Poorly absorbed preparations: unabsorbed part is excreted in the faeces and partly is excreted in milk and bile. Metabolism and excretion: The sulfonamides are degraded in the liver by acetylation, oxidation and conjugation with a glucuronic acid. Both parent compounds and metabolites are excreted in the urine (so, it is useful for the urinary tract infection). The acetylated form is insoluble in acid medium and liable to be precipitated in renal tubules (Crystalluria). Mechanism of action The sulfonamides inhibits incorporation of PABA into folic acid and thereby preventing the synthesis of folic acid, a compound essential to bacterial growth. Humans can not synthesize folic acid and must acquire it through their diet; thus, the sulfonamides selectively inhibit microbial growth. Antibacterial spectrum They are bacteriostatic chemotherapeutic agents, effective against gram-positive organisms, some gramnegative organisms and chlamydia. They also are effective against Toxoplasma gondii &chloroquine-resistant Plasmodium falciparum. Therapeutic uses Systemic uses: shrinking uses due to……………………? Local uses: Prevention of infections in burned patients e.g silver sulfadiazine. Sulfacetamide is used topically for treatment of ocular infections. Adverse effects Mild e.g. nausea, vomiting, headache, cyanosis and arthritis. Serious: 1-Crystalluria: it is a precipitation of acetylated form or sulfonamide itself in renal tubules leading to renal colic, haematuria, oliguria and even anuria Prevention: Give excess fluids (at least 2 liters urine/day) Give alkalinizing agent e.g. citrate, bicarbonate to prevent precipitation (i.e. increase solubility of sulfonamide and its acetylated form). 2-Allergic reactions e.g. rash, fever, hepatitis, skin and mucous membrane lesions (Erythema multiform). After using long acting sulfonamides in children (Stevens-Johnson syndrome). • Bone marrow depression leading to aplastic anaemia (agranulocytosis). • Haemolytic anaemia (idiosyncrasy) • especially in patients with defective glucose-6phosphate dehydrogenase. • Kernicterus • when given in last 2 weeks of pregnancy or to neonates and infants. It occurs with long acting sulfonamides if used for long time because sulfonamides compete with bilirubin for albumin leading to high free bilirubin concentration in blood. • Superinfection (with poorly absorbed sulfa). Drug interactions Through displacement from binding sites on plasma proteins of oral hypoglycemic drugs, oral anticoagulants (warfarin), methotrexate. Preparations of Sulfonamides Well absorbed from GIT: Short acting e.g. Sulfadiazine. Long acting e.g S. Doxine. Poorly absorbed from GIT: S. Suxidine and S. Thalidine For local use only : S. Thiazole for wounds in absence of pus. Mafenide for wounds and burns in presence of pus. S. Acetamide: used as eye drops. Silver sulphadiazeine for infected burns, bed sores, etc. Others: S. Salazine for chronic ulcerative colitis. TRIMETHOPRIM Potent inhibitor of bacterial dihydro folate reductase Pharmacokinetics Absorption and distribution: Trimethoprim is well absorbed from the gastrointestinal tract. Because the drug is a weak base, so higher concentration will be trapped in acidic prostatic and vaginal fluids. It is also penetrate the cerebrospinal fluid. Mechanism of action Trimethoprim competitively inhibits dihydrofolate reductase, the enzyme that catalyzes the reduction of dihydrofolic acid (folic acid) to tetrahydrofolic acid (folinic acid) leading to decreased tetrahydrofolic acid coenzyme required for purine and pyrimidine synthesis. Antibacterial spectrum Similar to sulfonamide and more potent. It can be used alone in treatment of acute urinary tract infection,bacterial prostatitis (fluoroquinolones are preferred) and vaginitis. Adverse effects 1-Hypersensitivity to trimethoprim. 2-It produces the effects of folic acid deficiency which include megalobastic anaemia, leucopenia, and granulocytopenia. Prolonged therapy with full doses can interfere with haemopoiesis (only in those with initially low folate stores), so macrocytic anaemia is due to interference with conversion of folic to folinic acid may occur. Macrocytic anaemia can be reversed by folinic acid and this will not reverse the antibacterial action of trimethoprim since bacteria cannot utilize pre-formed folic or folinic acid because they do not absorb it. 3-Possible teratogenic risk in pregnancy. Trimethoprim is contraindicated in pregnancy because it is a folate antagonist. SULFONAMIDES COMBINATIONS: CO-TRIMOXAZOLE It is a combination of trimethoprim and S. methoxazole: Either drug alone is bacteriostatic, but in combination co-trimoxazole is bactericidal (because it inhibits two successive steps of the enzymatic pathway for the synthesis of folinic acid), less bacterial resistance develops and bacteria which were not sensitive to sulfonamides become sensitive e.g. Salmonella, Proteus. It is effective against salmonella, shigella, staphylococci, proteus, E.coli, haemophilus, Neisseria (Pseudomonas is usually insensitive). Mechanism of action Sulphamethoxazole acts on the first step in the folic acid synthesis pathway(see before). Trimethoprim acts on the second step in the folic acid synthetic pathway(see before). This step occurs in man, but the sensitivity of the enzyme that is inhibited is much greater in bacteria than in man, therefore, the drug is relatively safe. Uses of Co-trimoxazole 1-Respiratory infection due to H. influenza,pneumonia due to pneumocystitis carinii (opportunistic infection in patients with AIDS) 2-Urinary tract infection and prostatitis 3-Salmonella infection e.g. enteric fever 4-Shigellosis 5-Gonococcal urethritis. 6-Toxoplasmosis. Adverse effects Like sulfonamides and trimethoprim (see before) OTHER SULFONAMIDES COMBINATIONS 1-Sulfadoxine + pyrimethamine "Fansidar" (for treatment of chloroquine-resistant malaria which is caused by Plasmodium falciparum: 2-Sulfadiazine (or trisulfapyrimidine) + pyrimethamine for treatment of toxoplasmosis (drug of choice). 3-Silver S.diazine is applied to infected skin lesions e.g. burn. QUINOLONES Members 1-First generation: Nalidixic acid. 2-Second generation: Pipemidic acid. 3-Third generation: Most are fluorinated. They include ciprofloxacin , ofloxacin , etc… (Fluorination was found to produce compounds with greater antibacterial activity, achieving clinically useful drug levels in the blood and tissues). 4-Fourth generation: e.g. moxifloxacin, trovafloxacin . Spectrum Gram-negative organisms, e.g. E.coli, Proteus, Klebsiella, Shigella, Salmonella, coliform bacteria, Neisseria, Pseudomonus, and H. Influenza. Less active on gram-positive bacteria. Not active on anaerobes. Fourth generation: they are like third generation with enhanced gram-positive and antianaerobes activity. Fluoroquinolones generation 2nd generation 3rd generation 4th generation Nalidixic acid Pipemidic acid Ciprofloxacin Trovafloxacin Levofloxacin Moxifloxacin 1st Members Norfloxacin Ofloxacin Spectrum: Excretion More active on G -ve (E.coli, Shigella, Proteus) Renal active onG-ve & lessactive on Gm . Renal Active on G -ve, G+ve, & Pseudomonas G -ve, G+ve, Pseudomonas & anaerobes Renal & biliary Renal & biliary Mechanism of action They inhibit DNA synthesis by inhibition of DNA gyrase needed for the synthesis of bacterial DNA. Pharmacokinetics They are readily absorbed from GIT, diffuse into tissues including prostate. They are metabolized in the liver. Excretion is renal and biliary (3rd and 4th generations). Antacids (Mg & Al antacids) & sucralfate decrease their GIT absorption. Therapeutic uses 1-GIT infection caused by salmonella (enteric fever), shigella, E.coli. 2-Urinary tract infections , genital tract infection e.g gonorrhea and prostatitis. 3-Third generation can be used in severe systemic infections. 4-Ciprofloxacin is also used in treatment of meningitis (due to H. influenza, N. meningitides), respiratory tract infections. 5-Treatment of skin infections, gonorrhea and septicaemia. 6-Treatment of bone infection e.g osteomyelitis and Septicemia. Adverse effects 1-GI upset (nausea, vomiting, abdominal pain), and pseudomembranous colitis. 2-Hypersensitivity reactions and photosensitization. 3-Neurological Adverse effects (headache, drowsiness, vertigo, and seizures). 4-Fluoroquinolones should not be used in children up to 17 years as it causes arthropathies in experimental animals, also it is avoided in pregnancy and lactation. 5-Interstitial nephritis and crystalluria. 6-Decrease metabolism of theophylline, warfarin and sulphonylureas leading to increase in their blood levels.