Sulfonamides trimethoprim and Quinolones
advertisement
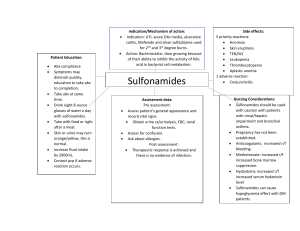
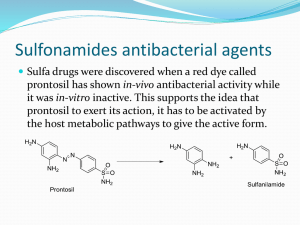
Sulfonamides, trimethoprim and Quinolones By S. Bohlooli, PhD School of Medicine, Ardabil University of Medical Sciences Antifolate drugs Sulfonamides Trimethoprim Trimethoprim & Sulfamethoxazole mixture Sulfonamides: chemistry Sulfonamides: mechanism of action Inhibition of dihydropetroate synthase Sulfonamides: antimicrobial activity Gram positive and negative bacteria Nocardia, chlamydia trachomatis Some protoza Some enteric bacteria Rickettisiae stimulated! Sulfonamides: resistance Overproduction of PABA Low affinity dihydropetroate synthase Loss of permeability to sulfonamides Sulfonamides: pharmacokinetics Oral absorbable Short Medium Long Oral, nonabsorbable topical Serum protein bind 20 ~ 90% Excreted into urine Pharmacokinetic Properties of Some Sulfonamides and Trimethoprim Drug Half-Life Oral Absorption Sulfacytine Short Prompt (peak levels in 1–4 hours) Sulfisoxazole Short (6 hours) Prompt Sulfamethizole Short (9 hours) Prompt Sulfadiazine Intermediate (10–17 hours) Slow (peak levels in 4–8 hours) Sulfamethoxazole Intermediate (10–12 hours) Slow Sulfapyridine Intermediate (17 hours) Slow Sulfadoxine Long (7–9 days) Intermediate Intermediate (11 hours) Prompt Sulfonamides Pyrimidines Trimethoprim Sulfonamides: clinical uses Oral absorbable agents Sulfisoxazole, sulfamethoxazole Sulfadiazine: toxoplasmosis Sulfadoxine: long acting, in a combination for treatment of malaria Oral nonabsorbable agents To treat urinary tract infection Ulcerative colitis, enteritis, other inflammatory bowel disease Topical agents Sulfacetamide: ophthalemic Mafenide & silver sulfadiazine: topically Sulfonamides: adverse reactions Cross allergenic sulfonamide drugs: Urinary tract disturbances Thiazide, furosemide, diazoxide, sulfonylurea hypoglycemic agents, and others Fever, skin rashes, exfoliative dermatitis,photosensivity, urticaria, nausea, vomiting, diarrhea Stevens-Johnson syndrom Crystalluria, hemturia, obstruction Hematopoietic disturbance Hemolytic or aplastic anemia Granulocytopenia, thrombocytopenia, leukmoid reaction Hemolysis in G-6PDH deficient patients Kernicterus in newborn of mothers have taken near the end of pergnancy Trimethoprim: chemistry Trimethoprim: resistance Reduced cell permeability Overproduction of DHF reductase Altered affinity of reductase Trimethoprim: pharmacokinetics Usually given orally alone or in combination with sulfamethoxazole Mainly excreted into urine More antibacterial activity in prostatic and vaginal fluids Clinical use Oral trimethoprim Oral trimethoprim-sulfamethoxazole P jiroveci pneumonia, shigellosis, systemic salmonella infection, complicated urinary tract infection, Active against many respiratory pathogens Intravenous trimethoprim-sulfamethoxazole Acute urinary infection Gram negative sepsis, pneumocystis pneumonia Shigllosis, typhoid fever Oral pryrimethamine with sulfanamide With sulfadiazine in Leishmaniasis, toxoplasmosis With sulfadoxine in malaria Adverse effects Megaloblastic anemia Leukopenia, granulocytopenia Can be prevented by folinic acid The AIDS patients have high frequency of unwanted reactions DNA gyrase inhibitors Fluoroquinolones Nalidixic acid and cinoxacin Fluoroquinolones: chemistry Fluoroquinolones: chemistry-2 Fluoroquinolones: antibacterial activity Block of bacterial DNA synthesis by Inhibiting topoisomerase II, IV Gram positive & negative bacteria Mycoplasma & clamydia, legionella Some mycobacteria Anaerobic bacteria Fluoroquinolones: resistance Change in permeability Loss of affinity Fluoroquinolones: pharmacokinetics Well absorbed after oral administration Good distribution Divalent cations impair absorption Pharmacokinetic Properties of Fluoroquinolones Drug HalfLife (h) Oral Bioavailability (%) Peak Serum Concentration (mcg/mL) Oral Dose (mg) Primary Route of Excretion Ciprofloxacin 3–5 70 2.4 500 Renal Gatifloxacin 8 98 3.4 400 Renal Gemifloxacin 8 70 1.6 320 Renal & nonrenal Levofloxacin 5–7 95 5.7 500 Renal Lomefloxacin 8 95 2.8 400 Renal Moxifloxacin 9–10 > 85 3.1 400 Nonrenal Norfloxacin 3.5–5 80 1.5 400 Renal Ofloxacin 5–7 95 2.9 400 Renal Fluoroquinolones: clinical uses Urinary tract infection Bacterial diarrhea Even with multi-drug resistant organisms Shigella, salmonella, toxigenic E. coli Infections of soft tissues, bones and joints Intra-abdominal and respiratory tract infections Gonococcal infection Chlamydial urethritis and cervicitis Legionellosis Tuberclusis and atypical mycobacterial infections Fluoroquinolones: adverse effects Nausea, vomiting & diarrhea Headache, dizziness, insomnia, skin rash, abnormal liver test Acute hepatitis & hepatic failure: trovafloxacin Photosensivity: lomefloxacin, pefloxacin QT prolongation: sparfloxacin Hyperglycemia or hypoglycemia May damage growing cartilage: arthropathy Tendinitis Nalidixic acid & cinoxacin Excreted too rapidly Useful for urinary tract infections