03. Critical Thinking in Nursing Practice, Nursing Assessment

CRITICAL THINKING IN NURSING PRACTICE
NURSING
ASSESSMENT
DEFINITION OF CRITICAL THINKING
Cognitive process during which an individual reviews data and considers potential explanations and outcomes before forming an opinion or making a decision
“Critical thinking in nursing practice is a discipline specific, reflective reasoning process that guides the nurse in generating, implementing, and evaluating approaches for dealing with client care and professional concerns.”
Critical thinking involves the use of a group of interconnected skills to analyze, creatively integrate, and evaluate what you read and hear. To become a critical thinker you must be able to decide whether an author’s opinions are true or false, whether he or she has adequately defended those ideas, whether certain recommendations are practical, as well as whether particular solutions will be effective
CRITICAL THINKING SKILLS
To learn how to think critically, one must learn skills that build upon each other. Only by concentrating on and practicing these basic skills can mastery of critical thinking be achieved. The author lists three basic characteristics of the skills required to think critically: they are interconnected ( review a sample list of these skills), they build on each other, and they are goal-oriented in that we can constantly apply them to situations in everyday life.
CHARACTERISTICS OF CRITICAL
THINKING
Critical thinking involves the use of a kind of thinking called reasoning, in which we construct and/or evaluate reasons to support beliefs. Critical thinking also involves reflection — the examination and evaluation of our own and others’ thoughts and ideas. Finally critical thinking is practical. Actions are more rational if they are based on beliefs that we take to be justified. Critical thinking then, is the careful, deliberate determination of whether we should accept, reject or suspend judgement about the truth of a claim or a recommendation to act in a certain way.
CRITICAL THINKING STEPS
Knowledge
In terms of critical thinking, the basic level of acquisition of knowledge requires that you be able to identify what is being said: the topic, the issue, the thesis, and the main points
Comprehension
Comprehension means understanding the material read, heard or seen. In comprehending, you make the new knowledge that you have acquired your own by relating it to what you already know. The better you are involved with the information, the better you will comprehend it. As always, the primary test of whether you have comprehended something is whether you can put what you have read or heard into your own words.
Remember that comprehending something implies that you can go beyond merely parroting the material back but instead that you can give the material your own significance.
Application
Application requires that you know what you have read, heard, or seen, that you comprehend it, and that you carry out some task to apply what you comprehend to an actual situation.
Analysis
Analysis involves breaking what you read or hear into its component parts, in order to make clear how the ideas are ordered, related, or connected to other ideas. Analysis deals with both form and content.
Synthesis
Synthesis involves the ability to put together the parts you analyzed with other information to create something original.
Evaluation
Evaluation occurs once we have understood and analyzed what is said or written and the reasons offered to support it. Then we can appraise this information in order to \ whether you can give or withhold belief, and whether or not to take a particular action. Never put evaluation ahead of the other steps in critical thinking steps; otherwise, you will be guilty of a "rush to judgement." When emotion substitutes for reasons, evaluation incorrectly precedes analysis.
FORMULA FOR CRITICAL THINKING
Start Thinking
Why Ask Why
Ask the Right Questions
Are you an expert?
ASPECTS OF CRITICAL THINKING
Reflection
Language
Intuition
LEVELS OF CRITICAL THINKING
Basic
Complex
Commitment
Critical Thinking Competencies
Scientific method
Problem Solving
Decision Making
Diagnostic Reasoning and Inferences
Clinical Decision Making
Nursing Process
Components Of Critical Thinking
Scientific Knowledge Base
Experience
Competencies
Attitudes
Standards
Nursing Process is a systematic, rational method of planning and providing care which requires critical thinking skills to identify and treat actual or potential health problems and to promote wellness.
It provides a framework for the nurses to be responisble and accountable.
It consists of five sequential and interrelated steps or phases:
Assessment
Diagnosis
Planning
Implementation
Evaluation
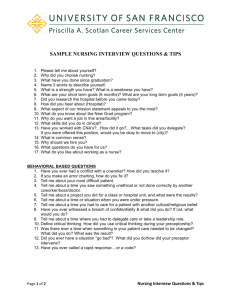
NURSING ASSESSMENT
Assessment is the first step in the nursing process and includes systematic collection, verification, organization, interpretation, and documentation of data for use by health care professionals. The accompanying display presents the essential elements of the assessment process. Effective planning of client care depends on a complete database and accurate interpretation of information. Incomplete or inadequate assessment may result in inaccurate conclusions and incorrect nursing interventions. Proper collection of assessment data directs decision-making activities of professional nurses.
The goal of assessment is the collection and analysis of data that are used in formulating nursing diagnoses, identifying outcomes and planning care, and developing nursing interventions. This chapter discusses the purpose of assessment, types of assessment, and the use of data in the assessment process.
Types of assessment
Comprehensive assessment
Focused assessment
Ongoing assessment
COMPREHENSIVE ASSESSMENT
A comprehensive assessment is usually completed upon admission to a health care agency and includes a complete health history to determine current needs of the client. This database provides a baseline against which changes in the client’s health status can be measured and should include assessment of physical and psychosocial aspects of the client’s health, the client’s perception of health, the presence of health risk factors, and the client’s coping patterns.
FOCUSED ASSESSMENT
A focused assessment is an assessment that is limited in scope in order to focus on a particular need or health care problem or potential health care risks. Focused assessments are not as detailed as comprehensive assessments and are often used in health care agencies in which short stays are anticipated (e.g., outpatient surgery centers and emergency departments), in specialty areas such as labor and delivery, and in mental health settings or for purposes of screening for specific problems or risk factors (e.g., well-child clinics). See the accompanying display for sample questions used to assess a client experiencing labor .
ONGOING ASSESSMENT
Systematic follow-up is required when problems are identified during a comprehensive or focused assessment.
An ongoing assessment is an assessment that includes systematic monitoring and observation related to specific problems. This type of assessment allows the nurse to broaden the database or to confirm the validity of the data obtained during the initial assessment. Ongoing assessment is particularly important when problems have been identified and a plan of care has been implemented to address these problems.
Systematic monitoring and observations allow the nurse to determine the response to nursing interventions and to identify any emerging problems.
DATA COLLECTION
The nurse must possess strong cognitive, interpersonal, and technical skills in order to elicit appropriate information and make relevant observations during the data collection process. This process often begins prior to initial contact between the nurse and the client, primarily through the nurse’s review of biographical data and medical records.
Upon meeting the client, the nurse continues data collection through interview, observation, and examination. A variety of sources and methods are used in compiling a comprehensive database.
TYPES OF DATA
Subjective data are data from the client’s point of view and include feelings, perceptions, and concerns. The data (also referred to as symptoms) are obtained through interviews with the client. They are called subjective because they rely on the feelings or opinions of the person experiencing them and cannot be readily observed by another.
Objective data are observable and measurable (quantitative) data that are obtained through observation, standard assessment techniques performed during the physical examination, and laboratory and diagnostic testing.
SOURCES OF DATA
The client should always be considered the primary source of information; however, other sources should not be overlooked.
The client’s family and significant others can also provide useful information, especially if the client is unable to verbalize or relate information. In addition, other health care professionals who have cared for the client may contribute valuable information. Medical records should also be reviewed, including the medical history and physical examination; results of laboratory and diagnostic tests and various health care professionals should also be consulted .
Secondary Source - physical exam, nursing history, team members, lab reports, diagnostic tests…..
Subjective
-from the client (symptom)
“I have a headache”
Objective - observable data (sign)
Blood Pressure 130/80
METHODS OF DATA COLLECTION
The nurse collects information through the following methods: observation, interview, health history, symptom analysis, physical examination, and laboratory and diagnostic data. These approaches require systematic use of assessment skills that are discussed below.
OBSERVATION
The nurse uses the skill of observation to carefully and attentively note the general appearance and behavior of the client. These observations occur whenever there is contact with the client and include factors such as client mood, interactions with others, physical and emotional responses, and any safety considerations.
Observation helps the nurse determine the client’s status, both physical and mental. By carefully watching the client, the nurse can detect nonverbal cues that indicate a variety of feelings, including presence of pain, anxiety, and anger. Observational skills are essential in detecting the early warning signs of physical changes (e.g., pallor and sweating).
INTERVIEW
An interview is a therapeutic interaction that has a specific purpose The purpose of the assessment interview is to collect information about the client’s health history and current status in order to make determinations about the client’s health needs. Effective interviewing depends on the nurse’s knowledge and ability to skillfully elicit information from the client using appropriate techniques of communication. Observation of nonverbal behavior during the interview is also essential to effectivem data collection.
Closed questions are questions that can be answered briefly or with one-word responses. For example, the question “Have you been in the hospital before?” is a closed question that can easily be answered by a one-word response. Questions about the dates of and reasons for the hospitalizations are also closed questions that require brief answers.
Open-ended questions are questions that encourage the client to elaborate about a particular concern or problem.
For example, the question “What led to your coming here today?” is open-ended and allows the client flexibility in response. Both closed and open-ended questions can be effective in collecting information
Assessment Techniques:
Inspection
INSPECTION is the most frequently used assessment technique. When you are using inspection, you are looking for conditions you can observe with your eyes, ears, or nose. Examples of things you may inspect are skin color, location of lesions, bruises or rash, symmetry, size of body parts and abnormal findings, sounds, and odors. Inspection can be an important technique as it leads to further investigation of findings.
Assessment Techniques: Auscultation
AUSCULTATION is usually performed following inspection, especially with abdominal assessment.
The abdomen should be auscultated before percussion or palpation to prevent production of false bowel sounds.
When auscultating, ensure the exam room is quiet and auscultate over bare skin, listening to one sound at a time. Auscultation should never be performed over patient clothing or a gown, as it can produce false sounds or diminish true sounds. The bell or diaphragm of your stethoscope should be placed on your patient’s skin firmly enough to leave a slight ring on the skin when removed.
Be aware that your patient’s hair may also interfere with true identification of certain sounds.
Remember to clean your stethoscope between patients.
Assessment Techniques: Palpation
PALPATION is another commonly used physical exam technique, requires you to touch your patient with different parts of your hand using different strength pressures. During light palpation, you press the skin about ½ inch to 3/4 inch with the pads of your ingers. When using deep palpation, use your finger pads and compress the skin approximately 1½ inches to 2 inches. Light palpation allows you to assess for texture, tenderness, temperature, moisture, pulsations, and masses. Deep palpation is performed to assess for masses and internal organs.
Assessment Techniques: Percussion
PERCUSSION is used to elicit tenderness or sounds that may provide clues to underlying problems.
When percussing directly over suspected areas of tenderness, monitor the patient for signs of discomfort. Percussion requires skill and practice.
The method of percussion is described as follows: Press the distal part of the middle finger of your non-dominant hand firmly on the body part. Keep the rest of your hand off the body surface. Flex the wrist, but not the foreman, of your dominant hand. Using the middle finger of your dominant hand, tap quickly and directly over the point where your other middle finger contacts the patient’s skin, keeping the fingers perpendicular. Listen to the sounds produced.
NURSING CARE PLANS
STUDENT____________________________________PATIENT INITIALS____________ROOM NUMBER__________DATES________________
ASSESSMENT NURSING DIAGNOSIS PLANNING IMPLEMENTATION EVALUATION
(supportive data) (patient's need) (nursing care needed) (documentation of care) (status of goal)
FACTUAL DATA PROBLEM STATEMENT
Supports your problem. This This is the name you give the information has to be current, or perhaps past history and NOT “make believe”. Think of it as problem. Ask yourself,
“What is the problem?”
You can use the NANDA list of problem statements OR if supportive data that proves you have an actual or potential problem. It must none apply, make a problem statement using one of the words: have at least 2 pieces of information to support problem.
Ask yourself, “Why do I think this is a problem?”
Alteration Impaired
Deficit Ineffective
Dysfunction Intolerance
Excess
Refrain from using:
Think about your pt’s:
1. Medical Diagnoses
Decreased Cardiac Output*
Disuse Syndrome
Impaired Gas Exchange*
Impaired Physical Mobility
Decreased Mobility (of any kind)
S & S from Dx that your pt is having right now Risk for Infection**
If no S&S right now, just
Risk of Ineffective Management of
Therapeutic Regimen* list the Dx as support
2. Medication List
Side effects?
3. Abnormal Lab?
*These problems must have specific data, measurements, lab tests, etc. in order to use these problems.
**There may be some very specific cases where it may be applicable.
Think, what can an “infection” can cause? Use that as a problem instead.
Goal : What do you plan to accomplish? Must be pt centered, AND specific, measurable, attainable, realistic, & time-sequenced.
NURSING PLAN FOR PROBLEM
Ask yourself, “What can I do for the problem?”
DOCUMENTATION
Ask, “What will I document?”
Any information that pertains to
These are not to be numbered. the problem.
This is your actual narrative charting notes just like on your
Think about the following:
O bservations you make related to this problem, (include assess-
Assessment Sheet in Level 1 or charted observations in the nurses ment of the pt re: to the body system re: this problem, diagnostic tests, and reporting of findings to charge nurse.
(Use notes in the chart. NOTE : This is
NOT a restatement of your plan in the past tense! Also it DOES NOT have to address each part of the plan. DO your senses).
T asks you can do (things you can
NOT number this section or leave spaces.
Also any conclusions , or judgments that are improper in charting are not proper here. do to prevent, repair, or reduce the problem). This includes medication adm., oxygen, dressing changes, turning, enema, catheter insertion,
Students have best results in learning how to word this section when they do not even look at the planning section.
Document: Date/Time nutrition, fluids, etc.
T eaching of patient & family
(includes not only what the doctor orders but what you as the “nurse” will teach the patient. Also should include how you will determine the patient’s understanding of the
1.
2.
3.
O
R
C bservations you made eporting observations and changes in condition to appropriate personnel are given to the patient how much, frequency (how often), etc. teaching.)
Be very SPECIFIC and very
THOROUGH. Include details like
4.
R esponse of the pt to the care
5. R esults of your actions, diagnostic tests, medications
6. T administered, etc. eaching specific to patient meds, needs, problems, preventative care.
DATE REVISIONS OR
ADDITIONS EVERY DAY!
DATE ENTRY EVERY DAY!
STATUS OF THE GOAL
Ask yourself, “Did I accomplish my goal?”
1. Look at your goal & ask yourself a question related to it - whether your Goal was met completely, met partially, or not met at all.
Write this down.
2 . Answer the question in a
Summarized Evaluation
Statement and relate it to the Measurable Part of the
Goal.
Write this down.
3. Does the problem or potential for the problem still exist?
Write this down.
4. Then, state if you will
Continue with your plan either as stated or as revised or Discontinue Plan.
Write this down.
NOTE : You must have something to back up this evaluation in your documentation in the
Implementation column
(Implementation supports or proves your evaluation statement).
Examaple:
Goal was partially met. The patient washed his face but did not brush his teeth himself. The problem still exists. Continue with the plan as revised.
Revised 0705 – 0495