Heart Failure PHCL
advertisement
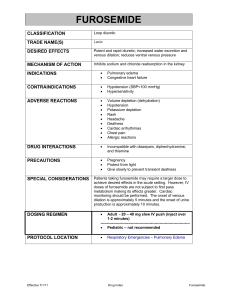
Heart Failure Dr. Emtenan AlHarbi Clinical pharmacy department Learning objectives Differentiate between the common underlying etiologies of heart failure, including ischemic, non-ischemic, and idiopathic causes. Describe the pathophysiology of heart failure as it relates to neurohormonal activation and the sympathetic nervous system Identify signs and symptoms of heart failure and classify a given patient by New York Heart Association Functional classification and ACC/AHA heart failure staging. Learning objectives the goals of therapy for a patient with heart failure. Non-pharmacological treatment plan which includes patient education for managing heart failure. Develop a specific evidence-based pharmacological treatment plan for a patient with heart failure based on disease severity and symptoms. Definition of HF HF is a complex clinical syndrome that results from any structural or functional impairment of ventricular filling or ejection of blood. The cardinal manifestations of HF are dyspnea and fatigue, which may limit exercise tolerance, and fluid retention, which may lead to pulmonary and/or splanchnic congestion and/or peripheral edema. Epidemiology Heart failure manifest most commonly in adults over the age of 60. The growing prevalence of HF! Men> women. Classifications of HF Primary underlying etiology as ischemic or nonischemic. 2. Main component of the cardiac cycle leading to impaired ventricular function. ( systolic or diastolic ) 3. Ventricular dysfunction can also involve either the left or right side or both. 1. Hypertension EF normal or increased EF < 40% , Usually from CAD Pathophysiology 3D Medical Animation Congestive Heart Failure Animation. Physiology Autonomic nervous system, where sympathetic stimulation of B adrenergic receptors CO= CO= HR 70ml\min 1. Preload (venous return) 2. Afterload (systemic pressure) 3. Contractility (inotropic state) * * SV 72 beat/min CO=5040 ml\min ~5L\min Pathophysiology Compensatory mechanisms: Preload and Frank-Starling mechanism. 2. Tachycardia and increased afterload. 3. Cardiac hypertrophy and remodeling. 1. Pathophysiology Neurohormonal pathways (RAAS + SNS) Angiotensin II Potent VC ↑SVR↑ BP↑afterload ↓SV ↓CO, it also reduces hypertrophy and the release of aldosterone, NE, ET1 and vasopressin Aldosterone Na+ -water retention ↑ preload and CO, it also cause electrolyte disturbance arrhythmia ↑HR and CO by sympathetic activation arrhythmia, ischemia, cell death. NE Endothelin Potent VC Arginine vasopressin Water retention (dilutional hyponatremia) and VC Pathophysiology Counter regulatory hormones Natriuretic Peptides (ANP, ↓Na absorption from BNP) kidney and cause VD by cGMP. Bradykinin VD peptide Nitric oxide VD and antagonize ET1 Framingham Criteria for Diagnosis of Congestive Heart Failure The concurrent presence of two major criteria or one major and two minor criteria were required for the clinical diagnosis of congestive heart failure Minor criteria were acceptable only if not attributable to another medical condition. Major criteria Paroxysmal nocturnal dyspnea Orthopnea Elevated jugular venous pulse/pressure Positive hepatojugular reflux (later renamed abdominojugular test) HF treatment (diuretic)-related 4.5 kg or greater weight loss in 5 days Rales Cardiomegaly (standing PA chest x-ray) Pulmonary edema (chest x-ray) S3 gallop Minor criteria Bilateral ankle (peripheral, dependent) edema Night cough Dyspnea on exertion/exercise Hepatomegaly Pleural effusion Tachycardia (over 120 bpm) Non-HF treatment-related 4.5 kg weight loss or more in 5 days Precipitating and Exacerbating Factors in HF Negative Prognostic Factors Clinical Increased Age, Diabetes, Smoking Laboratory Hyponatremia, Elevated neurohormones Electrophysiological A-fib, A-flutter, Ventricular ectopy, V- tach Hemodynamic Reduced EF, Increased Pulm Cap Wedge Pressure Clinical presentation and diagnosis Patient history PMH,FH and SH. Medication HX PND Clinical presentation and diagnosis* Diagnosis Signs: JVP and HJR watch this on Chest auscultation. Edema. Edema Diagnosis Laboratory tests. BNP. ECG. Scr\CBC. CXR. Echocardiogram. watch this on Tests for Patients with Suspected Heart Failure Test Indications Interpretation/considerations 12-lead ECG Routine HF unlikely if ECG completely normal; ECG may suggest the cause of HF CBC Routine Anemia may cause, exacerbate, or mimic (eg, "high-output") HF Urinalysis Routine Proteinuria indicates nephrotic syndrome or severe congestive HF; hematuria and casts indicate glomerulonephritis Serum electrolytes (including Mg, Ca) Routine Establish baseline before starting drug therapy (eg, exclude hyperkalemia) Serum creatinine, BUN Routine Elevated in renal failure/dysfunction; has major implications for HF management Liver (function) tests Routine Elevated levels may reflect hepatic congestion or alcohol-related cardiomyopathy; hypoalbuminemia may reflect protein losing enteropathy or poor nutritional status Blood glucose Routine Screen for diabetes Blood lipid profile Routine Screen for dyslipidemia TSH Routine Both hyperthyroidism and hypothyroidism can cause or contribute to HF Serum ferritin level, transferrin saturation Suspected hemochromatosis Hemochromatosis-related LV dysfunction improves with phlebotomy/chelation HIV screening test High-risk factors HF is usually a late manifestation of HIV infection Spirometry, peak flow Suspected pulmonary disease Comorbid ischemic heart disease and COPD common Chest radiograph Routine Cardiomegaly or pulmonary venous congestion suggests HF; may be first clue to underlying cardiac or pulmonary disease Echocardiography Routine (if HF still suspected after above studies) Most practical test for identifying and quantitating LV dysfunction and valvular lesions Radionuclide ventriculography Echocardiography findings inconclusive Provides highly accurate assessments of global and regional LV functions Revascularization candidate with angina Concurrent angioplasty (+/- stents), if indicated Laboratory Radiologic/imaging Invasive Coronary angiography Treatment of HF Desired therapeutic outcomes There is no cure for HF. The general management goals for chronic HF include preventing the onset of clinical symptoms or reducing symptoms. 2. preventing or reducing hospitalizations. 3. slowing progression of the disease 4. improving quality of life, and prolonging survival 1. Treatment of HF Control and treatment of contributing disorder Test for IHD. Control RF. Surgical repair if necessary. Condition \medication that exacerbate HF. Alcohol. Treatment of HF Non-pharmacologic intervention Weight self monitoring .(when to seek medical attention) Adherence.( how to improve) Dietary modification. (fluid\salt) Exercise (when? what?). Smoking cessation.(40% mortality) Immunizations. Treatment of HF Pharmacologic treatment 1. 2. 3. 4. 5. 6. 7. 8. Diuretics. ACE-inhibitor. ARBs Hydralazine\isosorbidedinitrate. B-blocker. Aldosterone antagonist. Digoxin. CCB. Stage D Inotropes — Inotropic agents are used during acute exacerbations of heart failure to improve cardiac output and to stabilize patients awaiting heart transplantation. Their effect is mediated through higher intracellular cyclic adenylate monophosphate (cAMP) levels, either by increased production (catecholamines) or by decreased degradation (phosphodiesterase III inhibition). Catecholamines — Sympathomimetic stimulation by catecholamine agents improves myocardial contractility and may have an additional beneficial effect on peripheral vascular beds .Dopamine is the preferred drug during decompensated heart failure (usually in combination with intravenous milrinone), although dobutamine has the additive effect of reducing afterload. Milrinone — Intravenous milrinone, a phosphodiesterase III inhibitor, is the preferred drug in decompensated heart failure, as it increases contractility and reduces afterload without a significant increase in myocardial oxygen consumption. Treatment of HF Diuretics Diuretics inhibit the reabsorption of sodium or chloride at specific sites in the renal tubules. Loop diuretics have emerged as the preferred diuretic agents for use in most patients with HF. Thiazide diuretics may be considered in hypertensive patients with HF and mild fluid retention because they confer more persistent antihypertensive effects. Diuretics Diuretics act at the loop of Henle Loop diuretics: Bumetanide, furosemide, and torsemide Diuritic act in the distal portionof the tubule thiazides, metolazone, and potassiumsparing agents (e.g., spironolactone) Treatment of HF Loop diuretics. Practical Diuretic Use in Heart Failure Use diuretic cautiously in patients with poorly controlled diabetes symptomatic benign prostatic hypertrophy increased risk of volume depletion Review potential drug interactions (eg, thiazides markedly increase serum lithium levels but furosemide appears to have little effect) Treat diuretic refractory patients with both a thiazide and loop diuretic; administer the thiazide 1 hr before the loop diuretic and monitor closely for symptomatic hypotension Practical Diuretic Use in Heart Failure Treat mild volume overload with a thiazide (hydrochlorothiazide 25 mg/day) Treat moderate/severe volume overload, renal insufficiency (CrCl [GFR] 15-30 mL/min/1.73 m2), or thiazide-refractory edema with a loop diuretic (eg, furosemide 20-40 mg/day). Titrate to desired effect. Titrate diuretic to achieve 0.5-1 kg weight loss daily until euvolemic, then to maintain euvolemia; if furosemide requirement is more than 160 mg furosemide, divide into 2 doses daily Caution Diuretics can cause the depletion of potassium and magnesium, which can predispose patients to serious cardiac arrhythmias Excessive diuresis may result in prerenal azotemia, hypokalemia, hypomagnesemia, inability to optimize ACEI dose, and orthostatic hypotension. Practical Diuretic Use in Heart Failure Monitor serum electrolytes (especially K and Mg), BUN, and Cr closely until values are stable and whenever medication dosages are increased Fluctuations in volume status may require frequent diuretic dosage adjustments, which in turn requires close monitoring for electrolyte imbalances and hypotension Lying supine for 1-2 hr after receiving a diuretic increases its efficacy Management of diuretic-related complications Hyponatremia: If volume overloaded, restrict fluid intake to 1 L daily; if volume depleted, reduce diuretic dosage Hypokalemia (K less than 4 mEq/L): If persistent, consider adding a K supplement or K-sparing diuretic (eg, amiloride 2.5 mg/day or spironolactone 25 mg/day) to the ACEI and diuretic regimen; recheck K and Cr levels in 5-7 days; then, slowly increase dose as required. Check K and Cr 5-7 days after any dose change. Management of diuretic-related complications Hyperkalemia (K more than 5.5 mEq/L): Assess and correct potential causes (eg, K supplementation or K-sparing diuretic, ACEI intolerance, renal insufficiency, or digoxin toxicity). Hypomagnesemia: Add oral Mg supplementation; correction often facilitates correction of associated hypokalemia . Orthostatic hypotension: Absence of congestion and a raised BUN-to-creatinine ratio (more than 20:1) suggests over-diuresis and volume depletion; if not volume depleted, consider ACEI intolerance. Hydralazine and Nitrate Hydralazine and Nitrate (Hydranit and African american population): it is to reduce cardiac preload and afterload by achieving both venous and arterial vasodilation. Hydralazine is an arterial vasodilator and nitrates are predominantly venodilators. These effects can reduce intracardiac filling pressures which may reduce adverse cardiac remodeling. Digoxin Has a positive inotropic effect (mediated by Na+/K+ ATPase inhibition and increase in intracellular Ca+). It is improved isolated myocyte contractile performance (increased shortening velocity) and overall left ventricular (LV) systolic function . Has a negative chronotropic effect, exerts an antiadrenergic action in patients with heart failure (HF) by inhibiting sympathetic outflow and augmenting parasympathetic tone. Digitalis can also be beneficial in patients with HF due to systolic dysfunction with atrial fibrillation (AF) with rapid ventricular response. There is no evidence that digoxin improves survival in HF patients. Aldosterone antagonists Decrease sodium reabsorption and potassium excretion in the collecting ducts of kidneys. Their potassium-sparing diuretic effect makes them particularly suitable for use in conjunction with loop diuretics and thiazides. Both spironolactone and eplerenone have been shown to reduce mortality in adults with heart failure when added to standard therapy . This effect is independent of their diuretic effect and is mediated by inhibition of myocardial fibrosis, an important component of LV remodeling Side effects include hyperkalemia (with both) and gynecomastia (with spironolactone). ACE inhibitor and ARBs ACE inhibitors (cornerstone) and ARBs inhibit the RAAS, thereby decreasing afterload and improving cardiac output and, on chronic use, by mediating reversal of LV remodeling. Side effects: 1. Hypotension.(diuretics) 2. Hyperkalemia. 3. Cough. ARBs: usually reserved for patients unable to tolerate ACE inhibitors due to cough or angioedema. Calcium channel blockers Amlodipine and felodipine (little or no negative inotropic activity at the usual therapeutic doses) appear to be safe in patients with HF and can be used if treatment with a calcium channel blocker is necessary for another indication, such as angina or hypertension. BB Beta-blockers counteract the maladaptive effects of chronic sympathic activation of the myocardium. In adults with heart failure, they improve patient survival, reverse LV remodeling, reduce all-cause mortality and decrease hospitalization in patients with HF and left ventricular systolic dysfunction (LVEF ≤ 35 to 40 percent and decrease myocardial fibrosis. Relative contraindications of BB in patients with HF include ●Heart rate <60 bpm ●Symptomatic hypotension ●Greater than minimal evidence of fluid retention ●Signs of peripheral hypoperfusion ●PR interval >0.24 sec ●Second- or third-degree atrioventricular block ●History of asthma or reactive airways ●Peripheral artery disease with resting limb ischemia : BB In the absence of a contraindication, our recommendation is to offer carvedilol, metoprolol succinate, or bisoprolol to patients with NYHA class II, III, or stable class IV HF with left ventricular ejection fraction less than 40 percent Treatment of HF HF with preserved LVEF. Also called diastolic dysfunction (EF 40-60%) Causes: HTN and DM. Better survival. HFpEF Outcome evaluation Major outcome parameters focus on: (1) volume status (diuretics) (2) exercise tolerance. (3) overall symptoms/quality of life. (4) adverse drug reactions. (5) disease progression and cardiac function (echo Q 6 Months) Heart Failure References VardenyO,M.H.Ng .T(2010).Heart failure.in M chisholm,Tschwinghammer,BWells,PMalone,JKolesar.JDipiro. Pharmacotherapy principles and practice (2ed).McGraw Hill companies,Inc. 2013 ACCF/AHA Heart Failure Guideline: Full Text.Yancy et al. JACC Vol. 62, No. 16, 2013