HSC 3048 - Skills for Care
advertisement

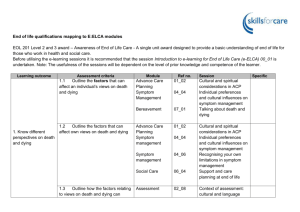
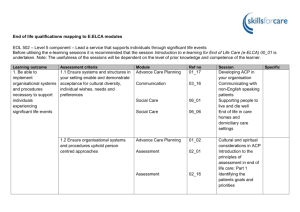
End of life qualifications mapping to E:ELCA modules HSC 3048 – Optional Level 3 – Support individuals at the end of life Before utilising the e-learning sessions it is recommended that the session Introduction to e-learning for End of Life Care (e-ELCA) 00_01 is undertaken. Note: The usefulness of the sessions will be dependent on the level of prior knowledge and competence of the learner. Learning outcome Assessment Criteria Module Ref. No Session 1. Understand the requirements of legislation and agreed ways of working to protect the rights of individuals at the end of life 1.1 Outline legal requirements and agreed ways of working designed to protect the rights of individuals in end of life care Advance Care Planning 01_01 Introduction to principles of ACP Advance Decisions to Refuse Treatment principles Mental Capacity Act: aims and principles Legal and ethical issues embedded in communication A unified DNACPR Policy Using the NHS Continuing Healthcare Fast Track Pathway Tool Hospital social work 01_05 Advance Care Planning Advance Care Planning 01_07 03_21 Communication 05_21 05_22 Integrating Learning Integrating Learning 06_05 Social Work 1.2 Explain how legislation designed to protect the rights of individuals in end of life care applies to own job role 2. Understand factors affecting end of life care 2.1 Outline key points of theories about the emotional and psychological processes that individuals and key people may experience with the approach of death Not covered Assessment 02_05 Assessment of psychological wellbeing Specific 2.2 Explain how the beliefs, religion and culture of individuals and key people influence end of life care Advance Care Planning 01_02 02_08 Assessment 03_05 Communication 04_04 Symptom Management 08_01 Cultural and spiritual considerations in ACP Context of assessment: cultural and language issues Cultural and language in communication Individual preferences and cultural influences on symptom management Spirituality and the philosophy of end of life care Spirituality 2.3 Explain why key people may have a distinctive role in an individual’s end of life care Not covered 2.4 Explain why support for an individual’s health and well-being may not always relate to their terminal condition Assessment 02_06 Assessment 02_16 Symptom Management 04_04 04_30 Symptom Management Integrating Learning 05_15 and 05_16 Assessment of social and occupational wellbeing Identifying the patients goals and priorities Individual preferences and cultural influences on symptom management Symptom management complicated by coexisting conditions These scenarios cover dying in prison or as a homeless person and may be useful 3. Understand advance care planning in relation to end of life care 3.1 Describe the benefits to Advance Care an individual of having as Planning much control as possible over their end of life care Assessment 01_03 02_16 04_04 Symptom Management 3.2 Explain the purpose of advance care planning in relation to end of life care Benefits and risks of ACP to patients, families and staff Identifying the patients goals and priorities Individuals preferences and cultural influences on symptom management Advance Care Planning 01_01 Introduction to principles of ACP 3.3 Describe own role in Advance Care supporting and recording Planning decisions about advance care planning Advance Care Planning 01_14 How to document conversations about advance care planning How to negotiate decisions which may be difficult to implement Developing your practice, clinical supervision, further reading 01_15 01_18 3.4 Outline ethical and legal issues that may arise in relation to advance care planning Advance Care Planning Advance Care Planning 01_01 01_05 Advance Care Planning Advance Care Planning Communication Communication 01_07 03_21 03_19 and 03_20 Introduction to principles of ACP Advance Decisions to Refuse Treatment principles Mental Capacity Act: aims and principles Legal and ethical issues embedded in communication These sessions cover request for organ and tissue donation as well as euthanasia that may be helpful 4. Be able to provide support to individuals and key people during end of life care 4.1 Support the individual and Advance Care key people to explore their Planning thoughts and feelings about death and dying Advance Care Planning Assessment 01_12 01_13 02_07 03_22 Communication 07_01 4.2 Provide support for the individual and key people that respects their beliefs, religion and culture Bereavement Advance Care Planning 01_02 02_08 Assessment 03_05 Communication 04_04 Symptom Management 08_01 How to get started and get the timing right How to handle patients questions and concerns Assessment of spiritual wellbeing ‘Am I dying?’ How long have I got?’ handling challenging questions Talking about death and dying Cultural and spiritual considerations in ACP Context of assessment: cultural and language issues Cultural and language in communication Individual preferences and cultural influences on symptom management Spirituality and the philosophy of end of life care Spirituality 4.3 Demonstrate ways to help Advance Care the individual feel respected Planning and valued throughout the end of life period Assessment 01_02 02_08 03_05 Communication 04_04 Cultural and spiritual considerations in ACP Context of assessment: cultural and language issues Cultural and language in communication Individual preferences and Symptom Management 08_01 cultural influences on symptom management Spirituality and the philosophy of end of life care Spirituality 4.4 Provide information to the individual and/or key people about the individual’s illness and the support available Advance Care Planning 01_14 02_17 Assessment Communication Communication 03_14 03_34 04_03 4.5 Give examples of how an individual’s well-being can be enhanced by: • environmental factors • non-medical interventions • use of equipment and aids • alternative therapies Symptom Management Assessment 02_06 Communication 03_04 Symptom Management 04_28 04_40 Symptom Management 4.6 Contribute to partnership working with key people to support the individual’s wellbeing Social Care Advance Care Planning 06_01 01_17 06_01 Social Care How to document conversations about advance care planning Documentation, communication and coordination Information giving Dealing with challenging relatives Communicating the plan of management and care Assessment of social and occupational wellbeing Talking with ill people: considering the surrounding environment in which conversations take place Non-drug interventions in symptom management Management of physical deterioration Supporting people to live and die well Developing ACP in your organisation Supporting people to live and die well 5. Understand how to address sensitive issues in relation to end of life care 5.1 Explain the importance of recording significant conversations during end of life care Advance Care Planning 01_14 02_17 Assessment 03_13 How to document conversations about advance care planning Documentation, communication and coordination Written communication Communication 5.2 Explain factors that influence who should give significant news to an individual or key people Advance Care Planning 01_11 01_15 Advance Care Planning Communication Communication Integrating Learning 03_14 03_15 05_01 to 05_04 5.3 Describe conflicts and legal or ethical issues that may arise in relation to death, dying or end of life care Communication 03_21 Bereavement 07_02 5.4 Analyse ways to address such conflicts Not specifically covered, but embedded in other sessions highlighted in this section Introduction to conducting conversations about advance care planning How to negotiate decisions which may be difficult to implement Information giving Breaking bad news These sessions cover differing scenarios around initiating conversations about end of life care that may be useful Legal and ethical issues embedded in communication Assessment of carers needs 6. Understand the role of organisations and support services available to individuals and key people in relation to end of life care 6.1 Describe the role of support organisations and specialist services that may contribute to end of life care Advance Care Planning 01_17 02_02 Assessment 06_01 Social Care 07_03 Bereavement 08_05 Spirituality 6.2 Analyse the role and value of an advocate in relation to end of life care Not covered 6.3 Explain how to establish when an advocate may be beneficial Advance Care Planning 01_07 02_11 Developing ACP in your organisation Introduction to principles of assessment in end of life care: Part 2 Supporting people to live and die well Practical support after a bereavement Spirituality and the multidisciplinary team Mental Capacity Act: aims and principles Assessment through proxies Assessment 6.4 Explain why support for spiritual needs may be especially important at the end of life Advance Care Planning 01_02 02_07 Assessment 08_01 Spirituality 6.5 Describe a range of sources of support to address spiritual needs Spirituality 08_01 to 08_06 Cultural and spiritual considerations in ACP Assessment of spiritual wellbeing Spirituality and the philosophy of end of life care These sessions make up the spirituality module and may be useful 7. Be able to access support for the individual or key people from the wider team 7.1 Identify when support would best be offered by other members of the team Advance Care Planning 01_02 04_06 Symptom Management 06_02 Cultural and spiritual considerations in ACP Recognising your own limitations in symptom management Palliative care social work Social work 8. Be able to support individuals through the process of dying 7.2 Liaise with other members of the team to provide identified support for the individual or key people Not specifically covered but embedded in a number of session already identified 8.1 Carry out own role in an individual’s care Advance Care Planning 01_18 Developing your practice, clinical supervision, further reading 8.2 Contribute to addressing any distress experienced by the individual promptly and in agreed ways Communication Symptom Management 03_33 04_26 Distress: the crying patient Managing distress during the dying phase Understanding and assessing spiritual need and spiritual distress 08_02 Spirituality 8.3 Adapt support to reflect the individual’s changing needs or responses Advance Care Planning 01_16 02_04 Assessment 02_18 Symptom How to review previous ACP decision Assessment of dying phase and after death Following up assessments and evaluating outcomes 8.4 Assess when an individual and key people need to be alone Management 04_05 Influence of transition points and crisis on decision making in symptom management Communication 03_03 Communicating with ill people 01_02 Cultural and spiritual considerations in ACP Assessment 02_14 Integrating Learning 05_19 Integrating Learning 05_20 Assessment of dying phase and after death Care after death 1 – Introduction to care after death Care after death 2 – Providing personal care after death 9. Be able to take action 9.1 Explain why it is important Advance Care following the death of to know about an individual’s Planning individuals wishes for their after-death care 9.2 Carry out actions immediately following a death that respect the individual’s wishes and follow agreed ways of working 9.3 Describe ways to support Assessment key people immediately following an individual’s death Symptom Management 02_09 04_26 05_13 Integrating Learning Integrating Learning Bereavement 05_14 07_01 to 07_06 Bereavement assessment and support Managing distress during the dying phase When the dying process is protracted or unexpectedly fast Sudden unexpected death These sessions make up the bereavement module and may be useful 10. Be able to manage own feelings in relation to the dying or death of individuals 10.1 Identify ways to manage own feelings in relation to an individual’s dying or death Assessment 02_14 Symptom Management 04_26 10.2 Utilise support systems to deal with own feelings in relation to an individual’s dying or death Not covered Assessment of dying phase and after death Managing distress during the dying phase