24 Non-carious cervical tooth surface loss: A
advertisement

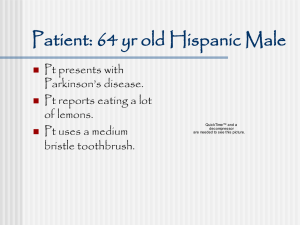
Tooth Surface Loss (TSL) can be carious and non carious. This article will concentrate on non carious TSL. TSL is experienced throughout a patients’ lifetime, but when it accelerates over the normal amount it can lead to functional and cosmetic concerns. TSL can be considered pathological if the degree of wear exceeds the level expected at any particular age1,2. TSL can be classified in 4 ways, abrasion, erosion, attrition and abfraction. Attrition due to TSL from tooth contact3. It includes TSL from restorations, eg. a porcelain restoration can cause attrition of opposing natural teeth. Attrition also includes wear of a restoration (Glass ionomer) due to the opposing natural tooth. Common causes for attrition TSL: 1. Parafunction eg bruxism4 2. Medication/medical conditions eg autism.5,6 3. physiological eg group function7 Diagnosis is by exam and questionnaire enquiring about causes. Clinical exam generally reveals flattened cusps/incisal tips with equal wear of dentine and enamel. It is known to affect approximal surfaces less. Attrition is generalised or localised. If localised it is likely due to an artificial cause such as porcelain restoration. Post Graduate Diploma in Restorative Dentistry Page 1 Figure 18 Abrasion is TSL due to mechanical wear from a foreign object3, eg. Musical instruments, floss, toothpicks, biting objects and excessive tooth brushing. Diagnosis is by questionnaire and examination. Possible questions include about habits and tooth brushing. Looking at the patient’s toothbrush, toothpaste and brushing technique is helpful. This includes time and frequency spent brushing, amount of force used, stiffness of brush/ bristles. Clinically, teeth have facial cervical TSL if due to toothbrushing. The TSL are notches/ grooves with sharp angles. TSL will be generalised to at least 2-3 or more teeth. It is unlikely one tooth with cervical TSL will be due to abrasion. It may be more evident on either left or right side depending on if the patient is left or right handed. It may have also caused a decrease in the zone of attached mucosa. Pipes, toothpicks, floss can cause localised TSL, especially if the object is repeatedly placed in the same location. Post Graduate Diploma in Restorative Dentistry Page 2 Figure 29 TSL due to acidic substances is erosion3,10. There are different methods to classify dental erosion (see tables 1, 2 and 3). Diagnosis is by questionnaire and examination. Post Graduate Diploma in Restorative Dentistry Page 3 Table 1. Scores and criteria of the Basic Erosive Wear Examination Index and the Simplified Tooth Wear Index. B.E.W.E. S-T.W.I. Score Criteria Score Criteria 0 No erosive tooth wear 0 No wear into dentine 1 Initial loss of surface texture 1 Dentine just visible (including cupping) or dentine exposed for less than 1/3 of surface 2 Distinct defect, hard tissue loss 2 Dentine exposure greater than 1/3 of surface 3 Exposure of pulp or secondary dentine <50% of the surface area 3 Hard tissue loss ≥50% of the surface area Post Graduate Diploma in Restorative Dentistry Page 4 Table 2. Pathognomic criteria of the Evaluating Index of Dental Erosion. Clinical criteria Score 0: no erosive tooth wear. Score 1: shallow defects located coronal from the CEJ or cupping of cusps, no dentine involved Score 2: shallow defects located coronal from the CEJ or cupping of cusps, dentine involved. Smith and Knight tooth wear index [30] Score Surface Criteria B/L/O/I No loss of enamel surface characteristics 0 C No loss of contour B/L/O/I Loss of enamel surface characteristics 1 C Minimal loss of contour B/L/O Loss of enamel exposing dentine for less than one third of surface 2 I Loss of enamel just exposing dentine C Defect less than 1 mm deep B/L/O Loss of enamel exposing dentine for more than one third of surface 3 I Loss of enamel and substantial loss of dentine C Defect less than 1–2 mm deep B/L/O Complete enamel loss–pulp exposure–secondary dentine exposure 4 I Pulp exposure or exposure of secondary dentine C Defect more than 2 mm deep–pulp exposure–secondary dentine exposure Post Graduate Diploma in Restorative Dentistry Page 5 Tables 1,2 and 311 Erosion pits develop with smooth enamel and little staining if active. They develop on any surface. Translucency and loss of enamel with dentine exposure occurs. Over time the pit becomes wider and deeper. Erosion commonly develops incisally/occlusally. Dentine is lost quicker than enamel, as it is easily demineralised. Cervical erosion looks differently from abrasion as it is generally wider and shallower, giving them a cupping appearance. 'Perimylolysis' is erosion of the palatal surfaces (figure 3) due to reflux or emesis (holst and Lange 1939)12. Erosion around restorations cause marginal defects and the appearance of restorations being higher than the tooth. figure 313 Erosion TSL can be further classified by extrinsic and intrinsic acids. Extrinsic Acids include food, drinks, medicines (eg Vitamin C/aspirin tablets), and environmental/occupational acids. Increasing frequency of consumption, amount, type (frozen, concentrated) and how it is consumed (less TSL if drunk quickly or through straws) increases erosion. Post Graduate Diploma in Restorative Dentistry Page 6 Environmental acids include poorly chlorinated swimming pools, illegal tooth bleaching substances, occupational hazards such as fumes from work 14, wine15 or food tasting. Intrinsic acids include physiological reasons of acids being produced internally and coming into contact with the dentition. The reasons could be due to: Anatomical defects like gastro oesophageal reflex disorders (GORD)/hiatus hernias. Side effects of medicines like NSAIDS etc Physiological conditions such as asthma can cause GORD. Diabetes can cause gastroparesis which causes GORD. Pregnancy and progesterone increases affect the function of the lower oesophageal sphincter, causing GORD. Xerostomia due to old age, medication etc invariably means the acid environment of the oral cavity is not neutralised. Psychological issues like overeating, alcoholism, anorexia and bulimia nervosa all cause acid reflux and erosion. Intrinsic causes develop erosion on the palatal/lingual aspects. Extrinsic aetiologies develop erosion labially/buccally. Abfraction is controversial cause16,17 and is heavily debated. It is stress induced TSL. Abfraction occurs cervically at the cement enamel junction (CEJ) as the tensile and compressive forces concentrate here3,18. Diagnosis is by elimination of other TSL and occlusal analysis for heavy/poor contact points. Non working side interferences should be investigated. Signs and symptoms of parafunction should be made. Abfraction is likely when there is a cervical lesion, Post Graduate Diploma in Restorative Dentistry Page 7 especially if v-shaped, subgingival and localised. Abfraction could be a sign of occlusal disharmony. If the tooth is mobile with a class 5 TSL it is unlikely to be abfraction, as the mobility dissipates the lateral forces which concentrate in the cervical region.19 Darker sclerotic TSL lesions are usually not sensitive as the lighter lesions. Figure 4 20 Management TSL management depends on the damage. Early TSL must be investigated, diagnosed and treated of any pain/sensitivity. Post Graduate Diploma in Restorative Dentistry Page 8 Identification of the disease process must be identified by starting with concise questioning of habits, diet, medical history. Dietary factors should be identified with a minimum 3 day diet sheet21. Diet analysis to control/reduce the causes can be undertaken. Generic advice can be given, as most TSL is multifactorial3. A well detailed questionnaire can be taken outlining possible habits, diet, parafunction, medical history etc until diagnosis can be made22. It is important the patient understands the cause and thus the possible treatment. This helps patient compliance. The patient must seek a medical exam if there is history of a medical condition. Suitable relevant specialists should be liased. For example if bulimia/anorexia is diagnosed, psychiatric evaluation should be undertaken. If gastric reflux is suspected, a general medical practitioner referral is appropriate. Generic advice can be given until aetiology is identified: Generic dietary advice: Consume erosive beverages through wide straw. Swallow immediately and not 'swish' around the mouth. Teeth should not be brushed following erosive substance. Finish meal with something neutral/alkaline (cheese/milk). Chew xylitol gum unless attrition/parafunctional habits. Post Graduate Diploma in Restorative Dentistry Page 9 Generic tooth brushing advice: Avoiding excessive toothbrush time, frequency, pressure Avoid abrasive toothpastes like natural or whitening/smokers toothpastes. Avoid back and forth techniques but circular or Bass techniques. Avoid hard bristled toothbrushes with no flexibility in the body. Generic parafunctional/attrition advice: Avoid chewy tough foods/objects in the mouth. Avoid chewing gum Provide hard acrylic splint Reflux/emesis advice Splints are useful in bulimics to protect their teeth during vomiting. Alkali (milk of magnesia) or high fluoride can be applied to splints to neutralise any acid pooling. Splints need extreme caution in use as there is a chance of acid being trapped beneath. High fluoride rinses, toothpastes like duraphat toothpaste (5000ppm sodium flouride) and Tooth Mousse help remineralise teeth. Acidulated phosphate fluoride should be avoided because of its acidity. All risk factors associated with the different TSL should be addressed. Post Graduate Diploma in Restorative Dentistry Page 10 If TSL is early then routine and regular monitoring can be undertaken. This is by study models, silicone putty impressions23 and photos. The dexterity of the photographer and ambient conditions affects the quality of photos and need to be considered when comparing. Radiographs may be used if pulpal involvement is suspected and possible periapical lesions. Tooth vitality tests can be undertaken. If TSL has lead to irreversible pulpitis28, then extirpation/extraction must be considered. After a few months, reassessment should be undertaken to see how the response to initial care. This should include whether the aetiology is still present or not. Patient’s long term expectations/views could be addressed. If TSL is dramatic and stabilisation is not slowing, restorative action should be undertaken, although controversial24. Advantages/disadvantages should be outlined to the patient and discussed in length. The restorations should be provided to protect existing dental tissue25. Post Graduate Diploma in Restorative Dentistry Page 11 If restoring the dentition has been decided, the treatment is dependent on the amount of TSL, age and medical history. Some papers have attempted to provide a classification for providing treatment depending on TSL types.26 (see Table 3) TSL can be treated in the conventional way. Cervical lesions being treated with composite, compomers and glass ionomer cements(GIC). Occlusal/incisal and palatal lesions are treated with composites or if posterior could also include amalgam. Exposed dentine in the occlusal and incisal areas can be be over-etched (20–30s) to enhance opening of dentinal tubules and intratubular formation of resin tags27. Composite is a good choice as it is not dissolvable by the acidic environment like GIC which can be acid soluble28. However some authors have mentioned the use of acid-etch when using composites actually exacerbates erosion TSL29,30. Restoring advanced TSL becomes more difficult and depends on a number of factors. Crown lengthening surgery, orthodontics and Dahl appliances can be utilised if there is a large TSL with insufficient room for the preparation of teeth for crowns/onlays. If there is a large amount of TSL with loss stable intercuspal position (ICP) then a reorganised approach may need to be investigated. This could include occlusal splint therapy to check stability of a new ICP (from a retruded position) and facebow analysis. The teeth are then temporised with long term provisionals restorations. Once occlusion is stable, permanent lab-based restorations are provided. If TSL is beyond restoring the teeth with laboratory restorations then overdentures can be considered. Post Graduate Diploma in Restorative Dentistry Page 12 If beyond overdentures, then extractions with provision of implants and dentures maybe the only option left. ACE CLASSIFICATION31 Table 3 PALATAL ENAMEL PALATAL DENTINE INCISAL EDGE LENGTH FACIAL ENAMEL PULP VITALITY SUGGESTED TREATMENT CLASS I REDUCED NOT EXPOSED PRESERVED PRESERVED PRESERVED NO TREATMENT CLASS II LOST IN MINIMAL PRESERVED PRESERVED PRESERVED PALATAL CONTACT EXPOSED COMPOSITES AREAS CLASS III CLASS IV LOST LOST DISTINCTIVELY LOST EXPOSED <2.1mm EXTENSIVELY LOST>2MM PRESERVED PRESERVED PALATAL COMPOSITES PRESERVED PRESERVED EXPOSED SANDWICH APPROACH (EXPERIMENTAL) CLASS V LOST EXTENSIVELY LOST>2MM EXPOSED DISTINCTIVELY PRESERVED REDUCED/LOST SANDWICH APPROACH (EXPERIMENTAL) CLASS VI LOST EXTENSIVELY LOST>2MM LOST LOST EXPOSED SANDWICH APPROACH (HIGHLY EXPERIMENTAL) There is no clear TSL index which accounts all causes like age. TSL is only pathological if it exceeds the normal amount of wear. So TSL it is difficult to quantify/qualify32,33,34. Studies on the U.K. population TSL should only be considered with tooth wear indices which account factors such as age. The actual prevalence of TSL is unclear but it is increasing in the UK population 35. Some evidence was seen in 25% of over 11 years old and on average between 58% of all age groups34,36,37. This could be attributed to a few reasons34. Post Graduate Diploma in Restorative Dentistry Page 13 There has been an increase in bruxism from occupational38,39 and student work related stress38,40. This can increase attrition and TSL. Another reason is an increase in the marketing of slim men and women. This has led to an increase in body dysmorphia and eating disorders41,42,43,44,45. As such there has been an increase in bulimia/anorexia and erosion/perimylolysis. Increases in juice/sports drinks cause erosion as people become more physically fit conscious46,47,48. Sports drink consumption can have a 2 fold problem as it is drunk during dehydration of a sports activity. Saliva buffering will be lower and erosion will increase. Refrigeration is now widely available and fruit production is plentiful throughout the year. Availability of fruit juice means they can be consumed throughout the year and is not limited to seasons. Public health messages now are focused on healthy eating of more vegetables and fruit. Patients are unlikely to be aware of the damage the acid erosion could do to their dentition. Parents feel “no added sugar” options are healthier and think young babies and children are at no harm from drinking copious amounts. Erosion is being seen in younger children. As the population becomes healthier, people are living longer and having their teeth longer. There is an increasing trend of restoring the dentition of the elderly, who obviously have a more worn set of teeth. Patients are increasingly having more aesthetic treatment, bleaching, composites, porcelain restorations, even in the posterior region of the mouth. They all can increase TSL. Porcelain causes attrition, phosphoric acids for composite and bleaching can cause erosion. So called “whitening” toothpastes are generally abrasive. Post Graduate Diploma in Restorative Dentistry Page 14 The UK has a changing population. Since the 1950’s there has been an influx of different cultures and diets. There is TSL prevalence in some communities than others. Some communities use various traditional abrasive methods to clean their teeth (miswaak49). Certain communities eat a highly abrasive diet, like high fibre rice50. Recreational drug use has been on the increase. From studies52 we are aware that that this increases TSL. If TSL is not prevented it will lead to early loss of teeth and occlusion, sensitivity and pain, loss in face height, psychological effects of a poor dentition25. Management of TSL is important. Early recognition/interception of TSL before further damage is priority. Education to patient, dentist and doctor is vital. If severe TLS is present patients should be educated on all the options. Without greater public health education there will be increasing further TSL. Post Graduate Diploma in Restorative Dentistry Page 15 References 1 British Dental Journal 186, 217 - 222 (1999) Published online: 13 March 1999 | doi:10.1038/sj.bdj.4800069 tooth surface loss: Occlusion and splint therapy N J Capp 2 Journal of Archaeological Science (2001) 28, 973–982 The Miles Method of Assessing Age from Tooth Wear Revisited A. E. W. Miles* 3 J Am Dent Assoc, Vol 135, No 8, 1109-1118. Attrition, abrasion, corrosion and abfraction revisited A new perspective on tooth surface lesions JOHN O. GRIPPO, B.S., D.D.S., MARVIN SIMRING, B.A., D.D.S. and STEVEN SCHREINER, B.S., M.S., Ph.D., P.E. 4 Dahl BL, Krogstad O, Karlsen K. An alternative treatment in cases with advanced localized attrition. J Oral Rehabil 1975;2:209-214. Post Graduate Diploma in Restorative Dentistry Page 16 5 J Indian Soc Pedod Prev Dent. 2008 Jun;26(2):82-4. Management of a child with autism and severe bruxism: a case report. Muthu MS, Prathibha KM. 6 ASDC J Dent Child. 1998 Nov-Dec;65(6):484-6, 439. Tooth wear in children: an investigation of etiological factors in children with cerebral palsy and gastroesophageal reflux. Shaw L, Weatherill S, Smith A. 7 J Am Dent Assoc. 2002 Jun;133(6):725-33. Characteristics of noncarious cervical lesions: a clinical investigation. Aw TC, Lepe X, Johnson GH, Mancl L. 8 http://bookasmile.com/A2ZDental.aspx 9 http://www.scritube.com/limba/engleza/health/ABFRACTION-ABRASION- ATTRITION-23155222.php 10 A literature review of dental erosion in children Australian Dental Journal Post Graduate Diploma in Restorative Dentistry Page 17 Volume 55, Issue 4, pages 358–367, December 2010 S Taji, WK Seow 11 Journal of Dentistry Volume 39, Issue 1 , Pages 88-93, January 2011 .Evaluation of three different scoring systems for dental erosion: A comparative study in adolescents Vasileios Margaritis, Eleni Mamai-Homata, Haroula Koletsi-Kounari, Argy Polychronopoulou 12 holst and Lange 1939, Perimylolysis- Acta Odontol Scand 1, 36-48 13http://www.google.co.uk/imgres?q=abfraction&hl=en&sa=X&qscrl=1&nord=1&rlz=1 T4SMSN_en___GB371&tbm=isch&prmd=ivns&tbnid=__i2RwMhz7mEJM:&imgrefurl =http://www.medfielddentist.com/nightguardsmouthguards.aspx&docid=_1oRXMGK D6EhLM&w=104&h=102&ei=E3c1TuVH4e3hQe119T7Cg&zoom=1&iact=hc&vpx=778&vpy=317&dur=2559&hovh=82&ho vw=84&tx=102&ty=78&page=1&tbnh=81&tbnw=83&start=0&ndsp=21&ved=1t:429,r: 18,s:0&biw=1280&bih=520 Post Graduate Diploma in Restorative Dentistry Page 18 14 Tooth surface loss and exposure to organic and inorganic acid fumes in workplace air Community Dentistry and Oral Epidemiology Volume 19, Issue 4, pages 217–220, August 1991Maija Leena Tuominen1,*, Risto Juhani Tuominen2, Frank Fubusa3, Nigodemus Mgalula3 15 SADJ. 2005 Oct;60(9):370-4. Patterns of tooth surface loss among winemakers. Chikte UM, Naidoo S, Kolze TJ, Grobler SR 16 Biomed Mater Eng. 2004;14(3):311-21. An assessment of stress analyses in the theory of abfraction. Litonjua LA, Andreana S, Patra AK, Cohen RE 17 J Oral Rehabil. 2004 Mar;31(3):225-32. Effects of occlusal load on cervical lesions. Litonjua LA, Bush PJ, Andreana S, Tobias TS, Cohen RE. 18 Eur J Oral Sci. 2004 Aug;112(4):347-52. Post Graduate Diploma in Restorative Dentistry Page 19 Undermining of enamel as a mechanism of abfraction lesion formation: a finite element study. Rees JS, Hammadeh M. 19 Grippo JO. Noncarious cervical lesions: the decision to ignore or restore. J Esthet Dent. 1992; (suppl 4): 55-64 20http://www.google.co.uk/imgres?q=abfraction&hl=en&sa=X&qscrl=1&nord=1&rlz=1 T4SMSN_en___GB371&tbm=isch&prmd=ivns&tbnid=__i2RwMhz7mEJM:&imgrefurl =http://www.medfielddentist.com/nightguardsmouthguards.aspx&docid=_1oRXMGK D6EhLM&w=104&h=102&ei=E3c1TuVH4e3hQe119T7Cg&zoom=1&iact=hc&vpx=778&vpy=317&dur=2559&hovh=82&ho vw=84&tx=102&ty=78&page=1&tbnh=81&tbnw=83&start=0&ndsp=21&ved=1t:429,r: 18,s:0&biw=1280&bih=520 21 British Dental Journal 186, 60 (1999) Tooth surface loss: Tooth surface loss: Editors' introduction R Ibbetson1 & A Eder2 22 Pediatr Dent. 2000 Nov-Dec;22(6):505-10. Post Graduate Diploma in Restorative Dentistry Page 20 The prevalence of dental erosion in a United States and a United Kingdom sample of adolescents. Deery C, Wagner ML, Longbottom C, Simon R, Nugent ZJ. 23 Analysis of Attrition in Adult Human Molars 1. C.L.B. Lavelle Journal of Dental Research 24 Non-carious cervical tooth surface loss: A literature review Journal of Dentistry Volume 36, Issue 10, October 2008, Pages 759-766 Ian Wooda, Zynab Jawadb, Carl Paisleyb and Paul Bruntonb, 25 Kelleher MGK , Bishop KA Tooth surface loss : an overview in Tooth Surface Loss. Editors Ibbottson R, Eder A Eds . BDJ Publications April 2000 3 – 8 26 Occlusal wear of teeth and restorative materials: A review of classification, etiology, mechanisms of wear, and some aspects of restorative procedures Acta Odontologica Scandinavica 1993, Vol. 51, No. 5 , Pages 299-311 BjÖRn L. Dahl1,2†, Gunnar E. Carlsson1,2 and Anders Ekfeldt1,2 Post Graduate Diploma in Restorative Dentistry Page 21 27 Van Meerbeek B, Braem M, Lambrechts P, Vanherle G. Morphological characterisation of the interface between resin and sclerotic dentine. J Dent 1994; 22: 141-146. 28 British Dental Journal 186, 109 - 113 Tooth surface loss: Eating disorders and the dentist A Milosevic 29 British Dental Journal 186, 61 - 66 (1999) Published online: 23 January 1999 | doi:10.1038/sj.bdj.4800020a1 Subject Category: Tooth surface loss Tooth surface loss: Tooth surface loss: an overview M Kelleher1 & K Bishop2 30 Journal of Oral Rehabilitation 2000 27; 875–880 Erosion of dentine and enamel in vitro by dietary acids: the effect of temperature, acid character, concentration and exposure time N. X. WEST, J. A. HUGHES & M. ADDY 31 Classification and Treatment of the Post Graduate Diploma in Restorative Dentistry Page 22 Anterior Maxillary Dentition Affected by Dental Erosion: The ACE Classification Francesca Vailati, MD, DMD, MSc* Urs Christoph Belser, DMD, Prof Dr Med Dent 32 Community Dentistry and Oral Epidemiology Volume 24, Issue 2, pages 152–158, April 1996 The tooth wear index: a flawed epidemiological tool in an ageing population group M. A. Donachie, A. W. G. Walls2 33 Clin Oral Investig. 2008 March; 12(Suppl 1): 15–19. PMCID: PMC2238784 Published online 2008 January 29. doi: 10.1007/s00784007-0184-2 The evolution of tooth wear indices Penny Fleur Bardsley 34 Acta Odontologica Scandinavica Post Graduate Diploma in Restorative Dentistry Page 23 An individual tooth wear index and an analysis of factors correlated to incisal and occlusal wear in an adult Swedish population 1990, Vol. 48, No. 5 , Pages 343-349 Anders Ekfeldt1,2†, Anders Hugoson1,2, Tom Bergendal1,2 and Martti Helkimo1,2 35 The Journal of Prosthetic Dentistry Volume 78, Issue 4, October 1997, Pages 367-372 The prevalence, etiology and management of tooth wear in the United Kingdom 36 British Dental Journal 200, 379 - 384 (2006) Published online: 8 April 2006 | doi:10.1038/sj.bdj.4813424 Non-carious tooth conditions in children in the UK, 2003 B L Chadwick1, D A White2, A J Morris3, D Evans4 & N B Pitts5 37 British Dental Journal 197, 413 - 416 (2004) Published online: 9 October 2004 Post Graduate Diploma in Restorative Dentistry Page 24 Epidemiological studies of tooth wear and dental erosion in 14-year-old children in North West England. 38 Quality in Higher Education Volume 9, Issue 1, 2003 Running Up the Down Escalator': Stressors and strains in UK academics Gail Kinmana & Fiona Jonesb 39 The Lancet Volume 359, Issue 9323, 15 June 2002, Pages 2089-2090 The causal links between stress and burnout in a longitudinal study of UK doctors ProfIC McManus FRCPa, 40 , , BC Winder PhDb and D Gordon Mscb Journal of Advanced Nursing Volume 43, Issue 1, pages 71–81, July 2003 Post Graduate Diploma in Restorative Dentistry Page 25 longitudinal cohort study of burnout and attrition in nursing students Ian J Deary BSc PhD MB ChB MRCPsych FRCPE AFBPsS CPsychol FRSE 1, Roger Watson BSc PhD RGN CBiol FIBiol ILTM FRSA2, Richard Hogston BA MSc RGN PGDipEd3 41 Journal of Psychosomatic Research Volume 42, Issue 3, March 1997, Pages 225-234 Androgenic-anabolic steroids and body dysmorphia in young men Anna-M. Wroblewska 42 Chung, Bryan. Muscle Dysmorphia: A Critical Review of the Proposed Criteria Perspectives in Biology and Medicine - Volume 44, Number 4, Autumn 2001, pp. 565-574 43 Journal of Clinical Psychology in Medical Settings Volume 10, Number 4, 297-306, Post Graduate Diploma in Restorative Dentistry Page 26 Eating Disorders in Men: Current Considerations Jeffery A. Harvey and John D. Robinson 44 The British Journal of Psychiatry (2005) 186: 132-135 Time trends in eating disorder incidence LAURA CURRIN, BA ULRIKE SCHMIDT, MD, MPhil, PhD, MRCPsych JANET TREASURE, MD, PhD, FRCP, FRCPsych HERSHEL JICK, MD 45 Eating Disorders Volume 18, Issue 1, 2009 Managing Eating Disorder Patients in Primary Care in the UK: A Qualitative Study 46 Journal of Dentistry Volume 32, Issue 7, September 2004, Pages 541-545 A comparison of enamel erosion by a new sports drink compared to two proprietary products: a controlled, crossover study in situ Post Graduate Diploma in Restorative Dentistry Page 27 S. Hoopera, N. X. Westa, N. Sharifa, S. Smithb, M. Northb, J. De'Athb, D. M. Parkerc, A. Roedig-Penmanc and M. Addy 47 British Dental Journal 190, 258 - 261 (2001) Tooth surface loss: Dental erosion in a group of British 14-year-old school children Part II: Influence of dietary intake Y H Al-Dlaigan1, L Shaw2 & A Smith 48 Medicine & Science in Sports & Exercise: January 2005 - Volume 37 - Issue 1 - pp 39-44 Clinical Sciences: Clinically Relevant Erosive Effect of a New Sports Drink on Dental Enamel during Exercise VENABLES, MICHELLE C.1; SHAW, LINDA2; JEUKENDRUP, ASKER E.1; ROEDIG-PENMAN, A3; FINKE, M3; NEWCOMBE, R G.4; PARRY, JASON2; SMITH, ANTHONY J.2 49 British Dental Journal 199, 503 - 504 (2005) The management of the Muslim dental patient S Darwish1 Post Graduate Diploma in Restorative Dentistry Page 28 50 Nutrition and Oral Medicine Nutrition and Health, 2005, III, 107-127 Oral Consequences of Compromised Nutritional Well-Being Paula J. Moynihan and Peter Lingström Post Graduate Diploma in Restorative Dentistry Page 29