Primary Care Providers - Appalachia Community Cancer Network
Understanding the Cancer
Information Needs of
Appalachian Cancer Survivors and Primary Care Providers
Robin C. Vanderpool, DrPH
NCI’s Cancer Information Service – Mid South Region
University of Kentucky College of Public Health
May 7, 2008 • ACCN Steering Committee Meeting
Funding received by NCI (3U01CA114622-03S3)
UK IRB Protocol No. 07-0529-P3H
Co-Investigators
• Dr. Mark Dignan – Mentor
• Dr. Nancy Schoenberg – Mentor
• Dr. Margaret Love – UK Family Medicine,
Kentucky Ambulatory Network
• Dr. Archana Kudrimoti – UK Family Medicine
(Hazard)
Community Partners
• Shirley Coleman – Nurse, Pikeville Medical Center; breast cancer survivor
• Sherry Payne – American Cancer Society Community
Representative; colon cancer survivor
• Jaime Caudill and Shirley Balman – KY AHEC
• Leigh Ann Bolinsky – Mountain Laurel Cancer Support and Resource Center @ MEOC
• Martha DeReamer and Allison Robinson – The Matrix
Group
Study Rationale
• Cancer continues to become a curable and manageable chronic disease – 10.5 million survivors
• An obvious source of cancer survivorship information and care are primary care providers (e.g., physicians, nurse practitioners, physician assistants).
• However, a recent IOM report (2006) reveals that there is a significant disconnect between cancer survivors and the healthcare system, including primary care clinicians.
• Once treatment is completed, patients frequently get
“lost in transition”.
Study Rationale
PCPs Providing Cancer Survivorship Care
Advantages
• Established, long-term relationships with patients and their families
• Local availability (routine care and emergencies)
• Coordination of care / referrals
• Preventive care
• Want to be involved in all stages of cancer care, including survivorship
• Less expensive medical care
• Safe and acceptable alternative
(Grunfeld, et al. 2006)
Disadvantages
• Inadequate oncology education and training
• Lack confidence to manage complexities of survivorship care
• Focus on acute medical problems
/ time constraints
• Small % of survivors in practice
• Lack of access to oncology-related
CE activities
• Inadequate patient histories related to cancer treatment
• Unclear role for follow up care and surveillance
Study Rationale
• Trans-HHS Cancer Health Disparities Progress
Review Group (March 2004) and Healthy People
2010
▫ “identify areas of strength, gaps, opportunities, and priorities to address cancer health disparities in research”
• The call for more cancer survivorship research related to provider-patient communication (IOM,
2006)
▫ Addresses rural issues in cancer survivorship, specifically in Appalachia
Study Goal
• To improve understanding of the dynamics of communication and information sharing between
Appalachian cancer survivors and their primary care providers.
▫ Help improve patient-provider and providerprovider communication, reduce cancer morbidity and mortality, and improve quality of life, and ultimately impact cancer disparities in Appalachia.
Specific Aims
1) Identify the cancer information and communication needs of Appalachian cancer survivors and their primary care providers.
2) Determine Appalachian cancer survivors’ experiences with and perceptions of their primary care provider in providing cancer survivorship care and information.
3) Identify the strategies used and challenges faced by
Appalachian primary care providers in managing the care and information needs of cancer survivors in their practices.
Theoretical Framework:
Patient-Provider Communication
Ong, et al., Soc Sci Med 1995; 40(7):903-918.
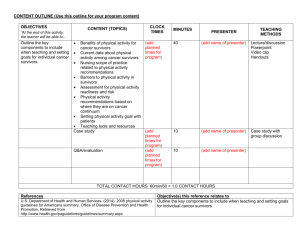
Research Design & Methods
• Modeling Duffey-Lind and colleagues’ (2006) recent work at the Dana-Farber Cancer Institute with pediatric cancer survivors, their parents and primary care providers, we proposed an exploratory, qualitative research study which utilized focus groups and in-depth interviews with Central Appalachian cancer survivors and primary care providers
Journal of Pediatric Oncology Nursing 2006; 23(6):335-343.
Recruitment – Survivors
• Community partners were integral in recruiting and referring cancer survivors to the study as well as focus group logistics
• Eligibility:
▫ Residence in an Appalachian-designated county
▫ Completion of their primary cancer treatment
▫ Not currently under physical or mental distress
• Varied lengths of survivorship, cancer diagnoses, ages, race/ethnicities, relationships with primary care providers
• $30 compensation, dinner, NCI materials
Cancer Survivors
• 3 Focus Groups
▫ Mountain Laurel Cancer Support Center –
Big Stone Gap, VA
▫ Pikeville Medical Center – Pikeville, KY
▫ Union College – Barbourville, KY
• 6 In-depth Interviews
▫ St. Claire Medical Center – Morehead, KY
▫ Survivor’s place of business - Norton, VA
▫ Mountain Laurel Cancer Support Center –
Big Stone Gap, VA
Cancer Survivors
Cancer Survivors
Cancer Types –
• Breast
• Thyroid
• Colon
• Bladder
• Brain
• Hodgkin Disease
• Cervical
• Leiomyosarcoma
• Endometrial
• Testicular
• Prostate
N=27
Age: Range 41-75 yrs, Mean 59.6 yrs
Marital Status:
• 19 Married
• 4 Divorced
• 3 Widowed
• 1 Never Married
Only 3 had children under age 18
Education:
• 8 HS Graduates
• 11 Some College
• 8 College Graduates
Cancer Survivors
Annual Household Income:
• 5 Less than $24K
• 8 $25-49K
• 9 $50-74K
• 5 $75K
Occupation:
• 11 Employed
• 8 Retired
• 5 Homemaker
• 3 Unable to work
N=27
General Health Perception:
• 1 Poor
• 9 Fair
• 8 Good
• 9 Very Good
If they thought their cancer was
coming back they would contact:
• 8 PCP
• 13 Cancer specialist(s)
• 5 Both
• 1 Neither
Cancer Survivors
N=27
• Oncology provider visits – Range from every 3 months to released from care
• PCP visits – Range from monthly / once a year / only for urgent problems / no PCP
• 18 feel their care was very or somewhat coordinated between oncology specialists and PCP.
• 23 feel their PCP is very or somewhat capable of addressing their physical and mental cancer-related side effects.
• Family members, friends, Internet – sources of cancer information
Cancer Survivors
• Treatment late effects
▫ Weight gain / loss, broken teeth, loss of taste, depression, fatigue
• Reliance on medical records
▫ “My folder says it all”
• PCP / patient relationships vary
▫ limited interaction → familial
• “Box” phenomenon
• PCP expectations
▫ Coordination of care; basic knowledge of cancer; referrals when appropriate
• Faith / Community Support
• Support groups & community resources; resources to help the family; nutrition and prevention; empathy from providers
Recruitment – Primary Care Providers
(MDs, NPs, PAs)
• Kentucky Ambulatory Network (KAN) membership list; Kentucky Medical Licensure Board directory;
Leigh Ann Bolinskey @ MEOC
• Eligibility:
▫ Practice in an Appalachian-designated county
▫ Minimum of 5 cancer survivors in current practice
▫ Family Medicine / Practice, Internal Medicine, General
Practice, OB/GYN*
• Varied practice sizes and sites, races/ethnicities, ages
• $100 compensation, dinner, NCI resources
Primary Care Clinicians
(MDs, PAs, NPs)
• 4 Focus Groups
▫ Pikeville Medical Center – Pikeville, KY
▫ UK Center for Rural Health – Hazard, KY
▫ London Country Club – London, KY
▫ Mountain Laurel Cancer Support Center –
Big Stone Gap, VA
• 3 In-depth Interviews
▫ St. Claire Medical Center – Morehead, KY
▫ Red Bird Mission Clinic – Clay County, KY
Primary Care Clinicians
Primary Care Clinicians
N=21
• 18 MDs, DOs
• 2 Physician Assistants
• 1 Nurse Practitioner
Age: Range 32-70 yrs; Mean 49.7 yrs
Practice Size: Range: One physician to larger residency clinics; most offices have at least one PA and/or one NP
Years Practicing: Range 2.5-40 yrs;
Mean 19.4 yrs
Practice Settings:
• Private practice
• Federally-qualified health centers
• Rural health clinics
If their patients thought their
cancer was coming back:
• 11 PCP
• 1 Cancer Specialist(s)
• 6 Both
Primary Care Clinicians
N=21
• 13 thought their patients’ care was very or somewhat
coordinated between providers
• All but one thought both oncology and primary care providers are responsible for the coordination and management of survivors’ care
• “Somewhat” – adequate oncology training; confidence in managing complexities of survivorship care; capable of addressing physical and mental cancer-related side effects
• Medical literature, colleagues, Internet – sources of cancer information
PCPs Managing Care and Information Needs of
Survivor Patients
Strategies
• Regular office visits
• Open inquiry
• Provide information from the
Internet
• Communication with oncologists
• Telephone follow-up
• Medical literature
• Connect patients to other survivors
• Refer to support groups, therapists, nurse
• Home visits
Challenges
• Patients’ fear, denial, fatalism
• Cancer treatment information
– constantly changing; hard to stay up-to-date
• Communication between PCPs and oncologist;
• Plans for follow-up
• Patient mis-information from media / family
• Getting patients to adopt healthy lifestyles (smoking, diet, etc)
• Barriers to care: finances, insurance, and transportation
Primary Care Providers
• Reliance on medical records
• No established guidelines or a “transition plan”
▫ “Just recognizing it as a transition would probably be a start…”
• PCPs want to be involved in survivors’ follow-up care
• Lack information on community cancer resources
• Recognize the verbal communication channels in the community
• Want to learn more about survivorship issues
Interesting Experiences Along the Way
Limitations
• Small sample sizes
• Male / Ethnic minority representation
• Self-selection / Self-report
• Generalizability
• Research precludes the perspective of oncologists and family members
Concluding Comments
“…we belong to a very unique club that nobody chooses to be a member of, but because we are cancer survivors, it has made us all better people. We look at every day and everything in life; it’s just so different than it was before.
It really does change you.”
“I think our relationship has changed since the cancer…he [the primary care provider] sees it as a learning experience too.”