Lymphedema - Alverno College Faculty
advertisement
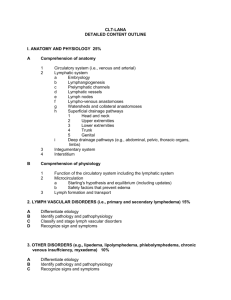
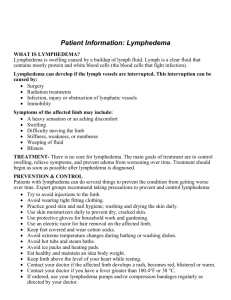
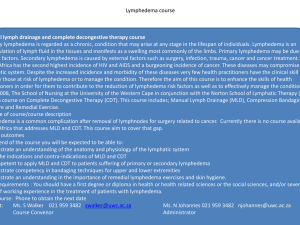
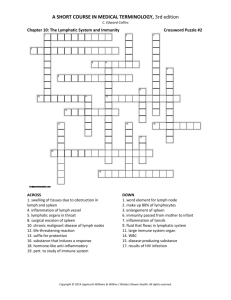
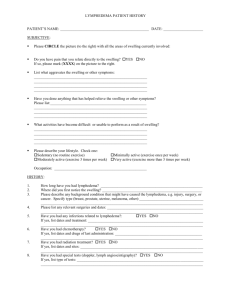
Lymphedema Emily Richter, RN, BSN, OCN Alverno College Spring 2007 Click on arrow for next slide Directions for Tutorial Use the arrows at the bottom of the page to move about the tutorial. This arrow moves you forward This arrow takes you back one page This button will take you back to the main menu Objectives Understand/describe the normal structure and function of the lymphatic system. Identify risk factors affecting the normal drainage of the lymphatic system. Discuss diseases or procedures that could predispose a patient to lymphedema. Explain assessment of a patient with lymphedema. Describe nursing interventions to promote lymphatic drainage for a patient with lymphedema. Participate in a case study Table of Contents Choose a topic listed below to go to that section of the tutorial. 1. Pathophysiology 2. Risk Factors 3. Diagnosis 4. Prevention and Treatment 5. Nursing Diagnoses 6. Case Study What is lymphedema? Lymphedema is an abnormal accumulation of high-protein concentrated fluid, usually in the arms and legs. Dell & Doll, 2006 Image reproduced with permission from vascularsociety.org The Lymphatics The lymphatic system filters and collects lymph and large molecules in the interstitial space that come from the intravascular space. Golshan & Smith, 2006 Used with permission from lymphacare.com Normally, the heart pumps so strongly that it causes 20-30 liters of plasma per day to leak from the capillaries. This is the interstitial fluid, which the lymphatic system drains, filters, and returns to the heart. Nazarko, 2006 This interstitial fluid contains proteins, lipids, water, and products from cellular breakdown. Golshan & Smith, 2006 Lymphatic vessels are similar to veins, but with thinner walls to allow larger proteins to permeate through. Holcomb, 2006 National Cancer Institute, 2006 Lymph vessels usually do not have a large basement membrane, which allows large molecules to enter that cannot be reabsorbed readily by the venous system. Golshan and Smith, 2006 Used with permission by www.med-ars.it Once this interstitial fluid is absorbed, it moves through the lymphatic vessels, and is considered lymph fluid. As lymph fluid moves through the lymphatic system, it passes through lymph nodes. Lymph nodes filter harmful substances and contain lymphocytes that activate the immune system. National Cancer Institute, 2006 Used with permission from Lymphnotes.com The lymph system carries the lymphocytes throughout the body to respond to antigens and communicate responses to other parts of the body. Lacovara & Yoder, 2006 Lymph then travels through multiple lymphatic channels and nodes before returning to the venous system by the thoracic duct. Golshan and Smith, 2006 Used with permission by med-ars.it Under normal conditions, the entry of fluid and other materials into the interstitial space is balanced by outflow of the lymphatic fluid from the limb, which maintains standard volume. Golshan and Smith, 2006 Used with permission from www.med-ars.it Lymphedema occurs when there is an interruption or obstruction of the lymphatic system that causes an accumulation of fluid in the limb. Golshan & Smith, 2006 Used with permission from lymphacare .com A healthy adult has approximately 600-700 lymph nodes. Lacovara & Yoder, 2006 The main areas are: Supraclavicular Retroperitoneal (deep abdomen and pelvis) Trachea Thoracic (adjacent to the lung) Thiadens, 2005 Abdominal (near the intestine) Axilla The pelvic area Inguinal Also found in tonsils, spleen, intestinal wall, and bone marrow. Thiadens, 2005 Identify Major Lymph Nodes Click on the body Spleen Cervical Nodes Axillary Nodes Inguinal Nodes Used with permission from cancerbackup.org Review of the “Flow” Click on the screen Interstitial fluid has diffused from blood capillaries The lymph capillaries absorb this interstitial fluid The capillaries join to form vessels that carry the lymph fluid back to the heart. Thoracic Duct The lymph fluid then enters either the thoracic duct or right lymphatic duct On the trip back, the lymph fluid passes through lymph nodes, where it is cleaned and filtered Mader, 1994 www.lymphacare.com The fluid is then enters the subclavian veins and is returned to the circulatory system. Why is the lymphatic system so important? (Click on all correct answers) A. The lymph system collects excess tissue fluid. B. It plays a major role in the body’s defense against disease. C. It circulates blood throughout the body Right! The lymph system absorbs interstitial fluid and returns it back to the blood circulation. Click here to return to question Correct! The lymph system circulates lymphocytes, such as T Cells, B Cells, and NK Cells. Click here to return to question Incorrect This is a different system…. the lymphatic system contains fluid, not blood. Click here to return to question Risk Factor: Surgery Any surgery that dissects or removes lymph nodes increases the risk of lymphedema by impairing the lymph flow. Marrs, 2007; Lacovara & Yoder, 2006 Common cancers that may require surgical alterations of the lymph nodes include breast cancer, melanoma, gynecological cancers, head and neck, prostate, testicular, bladder, or colon cancer. Thiadens, 2005 Risk Factor: Obstruction Tumors themselves may cause lymphedema by obstructing the lymphatic vessels. Dell & Doll, 2006 This is can be seen with cervical cancer, prostate cancer, or head and neck cancer. Nazarko, 2006; Romero, 2007. Risk Factor: Radiation Radiation therapy to the axillary or groin region around the lymph node can cause fibrosis and scarring of the tissue and therefore cause lymphedema to occur. Golshan & Smith, 2006 Risk Factor: Lymphedema and Breast Cancer It is estimated that 15-20% of patients with breast cancer will experience lymphedema. Lacova & Yoder, 2006 The tumor bed in the breast may drain into the lymphatics. Dow, 2002 The sentinel lymph node is the first lymph node draining from this tumor bed. Tumor Dow, 2002 Sentinel Node Used with permission from www.med-ars.it A technique called Sentinel Node Biopsy can be performed, which the surgeon finds and removes this first node and sends it for a pathologic examination. Dell, 2005 If the sentinel node is benign, no further lymph node removal is needed. Thaidens, 2005 However if the sentinel node is positive, the axillary nodes may need to be removed, which increases the chances of lymphedema by 30-60%. Golshan and Smith, 2006 Used with permission from Bocaradiology.org Other Risks: Infection and Injury Things such as infections, bug bites, and bee stings may lead to lymphedema in a high-risk patient. Trauma to the extremity at risk may also cause lymphedema. The rationale is lymphatic flow increases to the affected site, however there is an obstruction or defect in the lymphatic system, causing lymph fluid to leak. Dell & Doll, 2006 Other Possible Risks: Other causes that may lead to lymphedema include: Scarring from a vesicant extravasation Local burns Lymph node metastasis Itano & Taoka, 2005 Review: What cancers can be associated with lymphedema? Malignant Melanoma Gynecological Cancers Head and Neck Colon Prostate/Bladder Sarcoma Click on all of the correct answers Correct! Malignant Melanoma can lead to lymphedema. Here’s how: Malignant melanoma can metastasize to regional lymph nodes. Treatment for malignant melanoma may involve surgical resection; depending on location and extent of disease, the lymph nodes may need to be removed. Click here to return to question Itano & Taoka, 2005 Possible risk areas: Axillary Nodes Inguinal Nodes www. cancebackup. org Right! Here’s how: When you think of gynecologic cancers (ovarian, uterine, cervical), think location. Surgical removal of the inguinal lymph nodes puts the patient at risk for lower extremity lymphedema. Click HERE to return to question www. cancebackup. org Inguinal Nodes Correct! Head and Neck cancer can cause lymphedema. Here’s how: Squamous cell carcinoma occurring in the head and neck may obstruct lymph nodes or require removal of near by nodes. A common treatment of head and neck cancer also includes radiation. Romero, 2007 Click HERE to return to question Right! Here’s how colon cancer can lead to lymphedema: Tumors can invade beyond the submucosal layer and have direct access to the lymphatic system. Itano & Taoka, 2005 Treatment for colon cancer includes surgery and radiation, which may damage regional lymph nodes. Click HERE to return to question Good! Let’s look at how prostate and bladder cancer can lead to lymphedema: In advanced bladder cancer, a cystectomy may be performed, removing the bladder, prostate (men) and hysterectomy (women). Itano & Taoka, 2005 Radiation is also a method of treatment for advanced stages, putting regional lymph nodes at risk. This patient would be at risk for lower extremity lymphedema. Click HERE to return to question Yes! Sarcoma can lead to lymphedema. Here’s how: The goal of treatment for sarcoma is surgical removal. Itano & Taoka, 2005 Depending on location, lymph nodes may be damaged of removed Radiation may be used to reduce tumor size. This also puts lymph nodes at risk for fibrosis. Click HERE to return to question Diagnosing Lymphedema Painless swelling of the arms or legs, which may get worse during the day and better at night. Warmth or achiness in the extremity. A feeling of tightness, heaviness, tingling, numbness, or weakness in the affected extremity. Redness of the affected extremity. Bracelets, rings, or shoes may become tight. Lacovara & Yoder, 2006 Diagnosis, Continued… A 2 cm difference between affected extremity and non-affected extremity is a general classification. Bicego, et al, 2006 Tends to occur distal to proximal Increased pigmentation/superficial veins Secondary cellulitis Itano & Taoka, 2005 Infection Infection may be common in lymphedema; pooling of protein-rich lymph fluid increases cellulitis. Lacovora & Yoder, 2006 Low prophylactic doses of antibiotics may be used if patients develop cellulitis frequently. Thiadens, 2005 Cellulitis: used with permission from www.med-ars.it Stages of Lymphedema: Stage I Considered reversible There is pitting and the tissue is soft Arm girth may or may not be increased. Treatment = elevation Lacovara & Yodder, 2006 There is > 3 cm difference between extremities Itano & Taoka, 2005 Used with permission from lymphacare.com Stage II Considered irreversible May be non-pitting and fibrotic Elevation does not reduce swelling. Lacovara and Yoder, 2006 There is 3 to 5 cm difference between extremities. Itano & Taoka, 2005 Used with permission from lymphacare.com Stage III Tissues are hard and may have cartilage formation developing. Swelling is severe and may form deep crevices. Lacovara and Yoder, 2006 There is a > 5 cm difference between extremities. Itano & Taoka, 2005 Photo Courtesy of Lymph Notes (www.lymphnotes.com) Stage II Lymphedema is reversible TRUE Click on correct answer FALSE Correct! Stage II lymphedema is not reversible. With treatment, lymphedema may be minimized, but it is never truly “cured”. Continue on with the tutorial to learn about treatment options! No, unfortunately Stage II lymphedema is not reversible. With treatment, it is possible to minimize the effect. Continue with the tutorial to learn about treatment options! Click here to return to QUESTION Prevention No blood draws, IVs, blood pressures, or injections should be taken on the affected extremity. Thiadens, 2005 This includes all needle sticks, such as sub-q/IM injections and finger pricks for blood sugar testing. Cole, 2006 The rationale is if any foreign object, such as a needle, is placed in the affected extremity, it will cause an inflammatory response. This puts the lymphatic system under more stress, which may cause swelling to occur. Cole, 2006 Anything that may cause pressure needs to be avoided, including: Blood pressure cuffs Tourequets Tight clothes (waist bands, bra straps, socks) This constricts collateral circulation Dell & Doll, 2006 Good skin care: Keep the skin clean and dry Apply moisturizer daily Protect skin with sunscreen and insect repellant Use care with razors Wear gloves when gardening, etc to protect the skin Keep cuts clean and dry – monitor closely for S & S of infection Contact physician immediately for rash, redness, pain, increased swelling, etc. Thiadens, 2005 Avoid extreme temperatures. Heat may cause vasodilatation, which causes more fluid to move from the blood vessels into the tissues. Avoid hot showers and saunas. Dell & Doll, 2006 Cold may cause rebound swelling or chapped skin Thiadens, 2005 Air travel > 2 hours increases the risk of swelling because of continuous reduction of cabin pressure. It is recommended to wear a compression stocking while flying. Dell & Doll, 2006 Thiadens, 2005 Avoid carrying a purse, briefcase, or other heavy item with the affected extremity. If the lower extremity is affected, avoid standing or sitting for long periods of time and do not cross legs. Marrs, 2007 What would be a good method to identify an effected/at risk extremity? (Click on all of the correct answers) A. Have the patient carry a wallet card that identifies affected extremity. Use an ID bracelet or arm band to identify affected extremity. Tie a string around the affected extremity. Click here to move to TREATMENT OPTIONS Correct! Many patients carry wallet cards to remind themselves and healthcare provider of the affected extremity. Here is an example of what it looks like: Courtesy of www.lymphnotes.com Click here to return to question Yes! Many patients will wear ID bracelets on the affected extremity to alert healthcare providers to avoid venipunctures, blood pressures, and fingersticks on this extremity. Here is an example: Click here to return to question. Incorrect This is not an effective method of identification. If the string is too tight, it may constrict collateral circulation and cause lymphedema or make existing lymphedema worse! Click here to return to question Treatment Used with permission by www.bellisse.com Manual Lymph Drainage (MLD) Performed by specially trained therapist Massaging connective tissue rather that deep muscles Stimulates the weakened lymphatic system and decongests the affected area to encourage formation of new pathways to unimpaired lymph nodes to reduce swelling. May also be taught to patient to perform on self. Thiadens, 2005; Dell & Doll, 2006 Used with permission from lymphacare.com Compression Bandaging Bandages may be applied to increase tissue pressure and counteract the elastic insufficiency of the connective tissue. Thiadens, 2005 Used with permission from lymphacare.com Once a manageable size has been achieved from wrapping, a compression stocking may be worn to maintain the size and prevent increased swelling. Thiadens, 2005 Used with permission By knueppels.com There are no medications available at this time to treat lymphedema. Diuretics should not be used to help lymphedema because they draw off excess water in the interstitial spaces, not the excess protein. Once the diuretic is out of the system, it pulls more water into the affected area. Holcomb, 2006 Nursing Diagnosis Impaired physical mobility Disturbed body image Risk for infection Risk for impaired skin integrity Itano & Taoka, 2005 Case Study: A 49 year-old woman diagnosed with infiltrating or invasive ductal carcinoma of the right breast is scheduled for a mastectomy. To test the lymph node involvement, a sentinel node biopsy is performed, showing positive involvement. A modified radical mastectomy is then performed, removing all breast tissue and 15-20 axillary lymph nodes. How does this procedure put the patient at risk for lymphedema? (Click on the correct answers) A. There is minimal risk with this procedure. B. The lymphatic system needs time to heal itself, putting the patient at risk during this time. C. This impairs the lymphatic flow in the axillary region, making her more susceptible to lymphedema in the right arm. Incorrect Any time there is surgical removal of any lymph node, the patient is at risk for lymphedema. Please try the question again! Click here to return Incorrect The lymphatic system is not able to heal itself; therefore, the risk of lymphedema is always present. Please try the question again! Click here to return to the question Correct! When the lymphatic flow is impaired or obstructed, the risk of lymphedema increases. Area of concern Click here to go to the next question Used with permission from cancerbackup.org How much is the patients risk for lymphedema increased due to axillary node involvement? (Click on the correct answer) A. No increase B. 5% C. 10 - 15% D. 30 - 60% Golshan & Smith, 2006 Nope! Any time there is lymph node involvement, there is a risk of lymphedema Try again! Click here to return to the question Incorrect 5% seems a bit low…. Please try again! Click here to return to question. Try Again 5-10% is not the correct answer. Please try again. Click here to return to the question. Correct! The risk is 30-60%, which is pretty high! This is why it is so important to educate your patients and fellow nurses on prevention! Click here to go to the next question. Identify methods of prevention you will want to teach your patient: (Click on screen for answers) Good skin care Clean and dry Moisturize Use sunscreen Use electric razors Wear gardening gloves Keep cuts clean and dry Contact MD for any S & S of infection Avoid extreme temperatures Encourage caution with air travel Avoid carrying heavy things/extreme motions No blood draws/IVs/BPs/finger sticks in R arm!!! Click here to go to the next question After receiving chemotherapy, she is admitted for a neutropenic fever. When doing a physical assessment, what things should you be watching for with her right arm? Swelling in the right arm only Any edema (pitting or non-pitting) Watch for any redness and tight rings, watches, or bracelets. A feeling of heaviness, achiness, tingling, numbness, or weakness in the R arm reported by the patient. Click on screen for answers Click HERE to go to the next question You observe these signs and symptoms in her R arm. What are her treatment options? (Click on all correct answers) A. MLD – Manual Lymphatic drainage B. Wrapping the extremity C. Compression garment Click HERE to go to next question YES! MLD – Manual lymph drainage is a gentle massage performed in the affected area to help move the lymph fluid back in the appropriate direction. It should be performed at least once a day for about 10-15 minutes. Academy of Lymphatic Studies, 2006 Used with permission by www.bellisse.com Click HERE to return to question Correct! After MLD is performed, the extremity should be wrapped to reduce and soften fibrotic tissue. Academy of Lymphatic Studies, 2006 Used with permission from lymphacare.com Click HERE to return to question Right! Once the extremity is a manageable size, a compression stocking should be worn to maintain this size. Thiadens, 2005 Click HERE to return to question Used with permission By knueppels.com What are some possible nursing outcomes? (Click on all possible answers) A. Impaired physical mobility B. Disturbed body image C. Risk for infection D. Risk for impaired skin integrity Itano & Taoka, 2005 Click HERE to END tutorial Right! Lymphedema can make mobility difficult, especially lower extremity lymphedema. It is important to assess your patient and refer to physical therapy for exercises and activity restrictions. Click HERE to return to question Used with permission from lymphacare.com Correct! A patient with lymphedema may have a disturbed body image from such things as wearing over-sized clothes or two different sized shoes. It is important to address these things with your patient. Click HERE to return to question Yes! Infection may be common in lymphedema; pooling of protein-rich lymph fluid increases cellulitis. Lacovora & Yoder, 2006 Low prophylactic doses of antibiotics may be used if patients develop cellulitis frequently. Thiadens, 2005 Cellulitis: used with permission from www.med-ars.it Click HERE to return to question Correct! Skin on the affected arm may be more dry than normal. Academy of Lymphatic Studies, 2006 Good skin care is essential to prevent infection; wraps and compression stockings may retain moisture against the skin. Click HERE to return to question CONGRATULATIONS! You have successfully completed the tutorial!! Click HERE to view REFERENCES References Academy of Lymphatic Studies (2006 ) The source for research based lymphedema management. CD Rom. Sebastian, FL. ACOLS Bicego, D., Brown, K., Ruddick, M., Storey, D., Wong, C., Harris, S.R. (2006). Exercise for women with or at risk for breast cancer-related lymphedema. Physical Therapy. 86 (10). pp. 1398-1405. Cole, T. (2006). Risks and benefits of needle use in patients after axillary node surgery. British Journal of Nursing 15(18) pp. 969-979. Dell, D.D. (2005). Spread the word about breast cancer. Nursing2005 35(10). pp56-63 Dell, D.D., Doll, C. (2006). Caring for a patient with lymphedema. Nursing2006. 36(6). pp. 49-51. Dow, K.H. (2002). Pocket guide to breast cancer (2nd ed). Sudbury, MA: Jones and Bartlett Publishers. Golshan, M., Smith, B. (2006). Prevention and management of arm lymphedema in the patient with breast cancer. Supportive Oncology 4(8). pp. 381-386 Holcomb, S.S. (2006). Putting the squeeze on lymphedema. Nursing Made Incredibly Easy! 4(2). Pp26-34. Itano, J.K., Taoka, K.N. (2005). Core curriculum for oncology nursing (4th ed) Philadelphia, PA: Elsevier Saunders. Lacovara, J.E., Yoder, L.H. (2006). Secondary lymphedema in the cancer patient. MEDSURG Nursing. 15(5). pp. 302-306. Lewis, M.S., Heitkemper, M.M., Dirsken, S.R. (2000). Medical-surgical nursing: assessment and management of clinical problems. St. Louis, MO: Mosby. Mader, S. (1994). Understanding human anatomy and physiology (2nd ed). Dubuque, IA: Wm. C. Brown Publishers. Marrs, J. (2007). Lymphedema and implications for oncology nursing practice. Clinical Journal of Oncology Nursing. 11(1). pp. 19-21. National Cancer Institute (2006). www.cancer.gov. retrieved 4/5/07 Nazarko, L. (2006). Understanding lymphedema in older people. Nursing & Residential Care. 8 (6). Pp.254-258. Porth, C.M. (2005) Pathophysiology: concepts of altered health states (7th ed). Philadelphia, PA: Lippincott Williams & Wilkins. Romero, R. (2007). Bandaging options for head and neck edema. eLymphnotes. Retrieved from www.elymphnotes.org Thiadens, S.R.J., (2005). Lymphedema: an information booklet. (8th ed). Oakland, CA: National Lymphedema Network. Special Thanks To The Following For Permission To Use Graphics! Bellisse.com Bocaradiology.com Cancerbackup.org Knueppels.com Lymphacare.com Lymphnotes.com Med-ars.it Vascularsociety.org Special thanks to Ann from lymphnotes.com for sending wallet cards and handouts and to my preceptor, Julie Griffie, for all of her support.