Metabolic stone disease and medical management
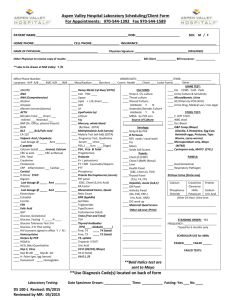
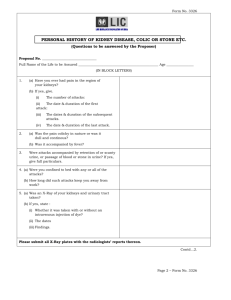
advertisement

Metabolic aspects of stone disease and metabolic management 16/07/2015 M Smolski Mr A Parnham Mr T Gunendran Source • EAU guidelines, Update March 2015 • Metabolic Evaluation and Recurrence Prevention for Urinary Stone Patients: EAU Guidelines. E Urol. 2015 • Calcium Kidney Stones. NEJM 2010 • Pearle at al. Medical management of stones. 2nd edition. • AUA guidelines • General metabolic tests for stone formers • Low risk and high risk patients • Evaluation of recurrent stone formers and patients at risk • Evaluation of patient based on stone composition • Non-medical and medical treatment in stone patients Case 1 • 50 female • Right colicky pain Case 1 • Hx – Mother had stones • Examination – mild tenderness R renal angle • Urinanalysis – pH 6.5, bld++, leuc++ Case 1 Management ? Basic metabolic testing Emergency and non-emergency setting: – Urinary dipstick + MSU – U+E, FBC, CRP, coagulation screen – Calcium – Uric acid – Stone for analysis UROLITHIASIS - LIMITED UPDATE MARCH 2015 Stone analysis • • • • IRS (infrared spectroscopy) XRD (x-ray diffraction) Polaristaion microscopy Wet chemistry – obsolete? Repeat stone analysis • Recurrence under pharmacological prevention • Early recurrence after interventional therapy with complete stone clearance • Late recurrence after a prolonged stone-free period Mandel et al. J. Urol. 2003 Patients with stones of unknown composition Medical history Stone history (former stone events, family history) Dietary habits Medication chart Diagnostic imaging Ultrasound Unenhanced helical CT in cases of a suspected stone Blood analysis Calcium (ionized calcium or total calcium + albumin) Uric acid Creatinine Urinalysis Dipstick test: leukocytes, erythrocytes, nitrite, protein, urine pH, specific weight Urine culture Urine pH profile Microscopy of urinary sediment (morning urine) Cyanide nitroprusside test (exclusion of cystinuria) Case 1 • • • • • URS U+E NAD Ca, Uric acid NAD Stone analysis - CaC2O4 or Ca (COO)2 FU? Case FU 1 Evaluation of patient’s risk • Low risk stone formers – general fluid and nutritional intake guidelines, lifestyle modification advice • High risk stone formers – extended metabolic evaluation Evaluation of patient’s risk • • • • • General factors Diseases associated with stone formation Genetically determined stone formation Drugs associated with stone formation Anatomical abnormalities associated with stone formation Skolarikos et al. E. Urol 2015 Extended metabolic evaluation • Basic metabolic evaluation • Plus stone type individualised specific metabolic evaluation: – 2 x 24-h urine collection – Spot urine sample where urine collection difficult i.e. children Timing • First timer - when the patient stone-free, 20 days after stone passage, on normal diet • For follow ups: – 8-12/52 after commencing prophylaxis/treatment – Then 12 monthly 24-H urine collection test • Liaise with local laboratory regarding the day of urine collection, as collection finished on the weekend may be difficult for lab analysis • Liaise with local laboratory re: number of bottles used and preservatives in bottle • In UK – usually use 2 bottles – Bottle 1- Hydrochloric Acid to maintain pH 2-2.5 to prevent precipitation of calcium oxalate or calcium phosphate, to test calcium, oxalate, phosphate, citrate and magnesium – Bottle 2 – plain, to test for uric acid and pH • Variation such as – Bottle 1 – Hydrochloric acid (reason as above), Bottle 2 – Alkali preservative to achieve pH=9 to prevent or reduce risk of uric acid precipitation and same specimen can be use for cystine analysis 5% Thymol in isopropanol stored at 8o C 24-H urine collection test • First 24-hr Urine Collection (Container with preservatives) • • Get up at normal time in the morning First urine sample in the morning flush down the toilet. Note the exact time (This will be the start time of the urine collection). Do not collect this sample. Write down the start date and time on bottle Collect every drop of urine passed during the day and night into the bottle provided. At exactly the same time the following morning, empty bladder again (i.e. 1st urine in the morning) and add this sample to the collection container. Write down collection finish date and time • • • • Second 24-hr Urine Collection (Container without preservatives) • Repeat the same procedure as above • The urine bottles should be brought into the lab on the same morning when the second urine collection is finished. Recommendations for general preventative measures • • • • • • • Diuresis 2.0-2.5L/day Limit NaCl – 4-5 g/day Limit animal protein 0.8-1.g/kg/day Normal Ca content 1-1.2g/day Diet rich in fibre Retain normal BMI level Adequate physical activity Case 2 • 16 female • f/h of stones • Lt renal colic • • • • USS NAD CT KUB URS Stone analysis Case 2 • Carbonate apatite phosphate/ Calcium oxalate monohydrate • 80/20% • Further tests? Stone specific metabolic evaluation Calcium oxalate stone disease Calcium oxalate stone • Calcium oxalate monohydrate/ dihydrate • 90% idiopathic • 10% metabolic abnormality Tests • Plasma Creatinine, Na, K, Cl, Ca, uric acid, PTH (if Ca high) • Urinanalysis – volume, pH, specific weight, Na, Ca, Oxalate, uric acid, citrate, magnesium Hypercalcaemia -HPT -Sarcoidosis (Calcitriol) -Malignancy Urine pH • “Acidic arrest” (urine pH constantly < 6) may promote co-crystallisation of uric acid and calcium oxalate. Similarly, increased uric acid excretion (> 4 mmol/day in adults or > 12 mg/kg/day in children) can act as a promoter • Urine pH levels constantly > 5.8 in the day profile indicate renal tubular acidosis (RTA), provided urinary tract infection (UTI) has been excluded. UROLITHIASIS - LIMITED UPDATE MARCH 2015 Results EUROPEANUROLOGY67(2015)750–763 Hypercalcuria – 4mg/kg/24hrs – >7mmol (men) or >6mmol (women) – 250mg/day • with normocalcemia (idiopathic hypercalciuria, or granulomatous diseases) • with hypercalcaemia (hyperparathyroidism, granulomatous diseases, vitamin D excess, or malignancy Hypercalcuria-classification • Absorptive – Type1 – Type2 – Type3 • Renal leak • Resorptive • Idiopathic Hypercalcuria Absorptive Renal leak Resorptive Fasting Ca/Cr <0.11 >0.11 >0.11 Calcium load Ca/Cr >0.22 >0.22 >0.22 Serum calcium normal normal increased Serum PTH normal marginal increased Hypercalcuria-treatment EUROPEANUROLOGY67(2015)750–763 Hypercalcuria-management • Thiazides (chlortalidone, indapamide, hydrochlorothiazide) – Prevent exchange Na and Ca in distal tubules – Proven 50% reduction of Ca stone recurrence rate during a 3 year period in placebo controlled trials • Potassium citrate – inhibits growth and aggregation of calcium oxalate Ettinger et al. J. Urol. 1988 Hypocitrituria • • • • Urinary citrate < 320mg/day Implicated in up to 50% stone formers Reflects acid/base balance Common in RTA Hypocitrituria - treatment • Potassium Citrate EUROPEANUROLOGY67(2015)750–763 Hyperoxaluria • Dietary, Enteric, Primary • >40mg/day oxalate in the urine • <80mg/day – dietary hyperoxaluria • >80mg/day enteric or primary hyperoxaluria Causes • Dietary hyperoxaluria Reduce intake of rhubarb, tea, chocolate, nuts, spinach and strawberries Eliminate megadoses of vitamin C • Enteric hyperoxaluria (most common) Malabsorption syndromes (Crohn’s etc.) Bile salts increase permeability of intestinal mucosa to oxalate and calcium soap formation results in increased free gut oxalate • Primary hyperoxaluria Rare autosomal recessive disease Mutated alanine-glycoxylate aminotransferase (AGT) leads to very high levels of urinary oxalate (>100mg/day), causing CaOx stone disease, nephrocalcinosis and renal impairment (liver and kidney transplant required) Hyperoxaluria-treatment • Lifestyle modification - fluids, low oxalate diet • Pharmacological - K Citrate, Calcium supplements • Piridoxine at specialist centres? EUROPEANUROLOGY67(2015)75 0–763 Hyperuricosuria • Uric acid >700mg/day • Associated with excessive dietary intake of animal protein • Decrease the solubility of calcium oxalate and thus can increase the incidence of calcium oxalate stones Hyperuricosuria-treatment • Allopurinol • Alkaline Citrate or sodium bicarbonate EUROPEANUROLOGY67(2015)750–763 Ettinger at al NEJM 1986 Other recommendation • High sodium excretion • Restricted intake of salt • Small urine volume - Increased fluid intake • Urea level indicating a high intake of animal protein - Avoid excessive intake of animal protein • No abnormality identified - High fluid intake Stone specific metabolic evaluation Calcium Phosphate stone disease Calcium Phosphate stone disease • Calcium hydroxyl phosphate - Carbonite apatite - Ca5(PO3)3(OH) • b-tricalcium phosphate - Whitlockite Ca3(PO4)2 • Carbonate apatite phosphate - Dahllite Ca5(PO4)3OH • Calcium hydrogen phosphate - Brushite PO4.2H2O Calcium Phosphate stone disease • Apatite – may be associated with infection • Brushite – crystallises at high urinary concentration of calcium and phosphate. Not related to UTI. Very hard hence difficult to treat • Possible causes include HPT, RTA, UTI Tests • Plasma Creatinine, Na, K, Cl, Ca, PTH • Urinanalysis – volume, pH, specific weight, Ca, P, Citrate Carbonate apatite stones EUROPEANUROLOGY67(2015)750–763 RTA • Renal tubular acidosis is caused by severe impairment of proton or bicarbonate handling along the nephron • Kidney stone formation most probably occurs in patients with distal RTA type I. EUROPEANUROLOGY67(2015)750–763 RTA RTA - Management • The main therapeutic aim is restoring a normal acid-bas equilibrium • Alkaline citrates or sodium bicarbonate is key to normalising the metabolic changes (intracellular acidosis) responsible for stone formation Brushite stones Stone AUA guidelines in a snapshot Uric acid stones Overview • • • • • • 15% of urinary stones Elderly i.e >60 or young chubsters Uric acid stones form in acidic conditions Diet rich in proteins and purines and alcohol 20-40% of gout patients will form uric acid stones Uric acid dihydrate forms in really acidic urine <5.5 • Only stones that can be dissolved medically • Different from Urate stones Uric acid vs Urate stones Low urine pH High urine pH High conc of uric acid High conc. Of urate and cation Uric acid stone Urate stone Notes • Medical history – Disturbances in metabolism of uric acid • Cell death – Anaemia, neoplastic conditions, intoxication, cardiac infarct, irradiation, cytotoxics • Enzyme defects – Primary gout, Lesch-Nyhan • Alterations in the excretion – Renal insufficiency, metabolic acidosis – Medications • Uricosurics, diuretics, analgesics, vitamin C Programme for testing • Urine analysis – pH <5.8 – Crystals with whetstone appearance or right angles. Fine crystalline ‘brick-meal’ in sediment • Serum analysis – Uric acid >380υmol/l (6.4mg/100ml) • Establishing diagnosis – Stone analysis Biochemical investigations • Serum uric acid – Man 155-404 υmol/l – Women 119-375 υmol/l • Blood pH is slightly alkaline and the risk of precipitation is determined by the solubility of sodium urate • The solubility limit at pH 7.4 @ 37oC is 380υmol/l • Therefore values above 380 are considered as hyperuricaemia and require therapeutic measures • If uric acid is persistently between 300 and 380 suspicion of latent hyperuricaemia in dietetic purine loading Urine analysis • The lower the pH and the higher the uric acid, the greater the risk of uric acid precipitation • The reason for an extremely low pH should be investigated Urine analysis • Spot urine – pH <5.8 suspect constantly acidic urine • pH day profile – Patient records urine pH every time voids for 24 hrs (check vision) – pH constantly <6.0 establishes diagnosis of acid urine • 24 hr urine – Uric acid ≥4.0mmol/24hrs (672mg) Treatment • Chemolysis • Metaphylactic Treatment- Chemolysis • Stone dissolution (Chemolysis) – Stone free rates ~90% – Clearance rate depends on size, purity and diuresis – Remember uric acid stones form in low pH and high concentrations of uric acid so… 1. Increase urinary pH 2. Decrease uric acid excretion 3. Increase urine dilution 1. Chemolysis Urine alkalinisation – Aim for pH 7.0-7.2 • Medicinal agents – Alkaline citrate(potassium citrate, Uralyt U, Lithurex) • Dose depends on pH – Sodium Bicarbonate • Drinks – Mineral water with high concentration of bicarbonate (>1500mg HCO3-/L) – Citrus juices (beware energy load) 2. Chemolysis- Reduction of uric acid excretion Inhibiting endogenous production of uric acid – Aim for <4.0mmol uric acid/24hrs – Allopurinol • Dose 300mg OD if serum uric acid >380 and urine uric acid >4.0mmol/24 hrs • Dose 100mg OD if urine only >4.0mmol/24hrs • CI: reduce dose in renal insufficiency. Pregnancy and liver disease • SE: Increased xanthine excretion (xanthine stones in pts with Lesch-Nyhan. Altered blood cell formation, hypersensitivity, interactions with anticoag and antihistamine Adenine Hypoxanthine Allopurinol Xanthine oxidase Guanine Xanthine Xanthine oxidase Uric acid Oxypurinol 2. Chemolysis- Reduction of uric acid excretion Reduce purine intake • Restrict meat, fish, sausage, bean and mushrooms • Avoid innards, sardines, anchovies, sprats, herring, shellfish, skin from poultry and fish • Prefer eggs, dairy, fruits, veg, cereals – Plants have a lower purine content and can have an alkalising effect 3. Chemolysis- Increased diuresis • Aim for 2.5l of urine in 24 hr period • Mineral water rich in bicarbonate (>1500mg HCO3-/L • Citrus juice Metaphylaxis General measures • Weight loss – Avoid extreme fasting as increases uric acid excretion • Avoid large losses of fluid – Sweating, laxative abuse, sauna Urine dilution • Alkalising beverages- as previous • Urine neutral- kidney tea, bladder tea and fruit tea, dilute apple juice, mineral water with low mineral content • Suitable in limited amounts- coffee (max 2/day), black tea (max 2/day) – Stimulate metabolism and therefore can increase uric acid excretion • Unsuitable- all alcohol but beer worst, cola, lemonade and soft drinks with sugar – Increase uric acid excretion and acidify urine Metaphylaxis Diet • As previous Medical • Alkaline citrate or sodium bicarbonate – Increase urinary pH – CI: recurrent UTI, hypertension (control!), Phosphate stones, renal insufficiency, metabolic alkalosis, hyperkalaemia – SE: GI disturbances – Long term admin of Na-K-Citrate to patients with reduced renal function can lead to potassium intoxication. Replace with calcium citrate – Try to reduce dose with generous intake of alkalinsation beverages Long term Goals • Increased pH (6.5-6.8), • Reduced excretion of uric acid (<4mmol/24hrs), • Sufficient urine dilution ≥2.5L/24 hrs Struvite Overview • • • • 4-6% Always caused by UTI with urease producing bacteria 2x more common in females than males Stones in infants are mostly struvite, whereby boys are afflicted • UTI high ammoniapH>7.0 reduced solubility of phosphatesstruvite ad carboonate apatite crystallisation • High urine volume and acidification mainstays of treatment Notes Medical history – Fertile women and during pregnancy, <15 yrs old at first presentation – Recurrent UTIs (commonly found in association with anatomical and functional abnormalities) Programme for testing • Urine analysis – pH >7.0 – Leucocytes and nitrites – Sediment with coffin lid like crystals • Serum analysis – Creatinine possibly increased • Establishing diagnosis – Stone analysis Biochemical investigations pH day-profile • pH constant >7.0 (keep in mind RTA) 24 hr urine collection • Ammonium ≥50mmol/24hrs • Phosphate ≥35 mmol/24hrs Diagnosis of UTI • Test strips • Number of bacteria • Bacterial strain, resistance pattern and urease activity – Proteus, klebsiella, pseudomonas, providencia, serratia, staph Metaphylaxis • Complete removal of stone – Residual concrements not only hinder recovery but inevitably result in relapse – General measures • UTI prevention measures • Avoid excessive fluid losses (see before) • Avoid immobilisation – Increased calcium and phosphate excretion as a result of osteolysis, reduced urine flow Metaphylaxis • Urine dilution – 2.5-3L/day – Preferably acidifiying and neutral beverages • HCO3- poor mineral water • Dilute cranberry juice? (1L cranberry juice contains 480Kcal) – Unsuitable • Citrus juices (alkalising) • HCO3-rich mineral water (>500mg HCO3-/l) • Cola, lemonades, soft drinks with sugar, alcohol Metaphylaxis Diet • Balanced diet • Avoid pure vegetarian diet as can cause alkalization • Animal foodstuffs cause acidification Metaphylaxis Medical • Long term infection therapy • Acidification of urine (beware complete RTA) – Monitor pH daily – L-methionine (Acimethin) • Dose: pH dependent 200-500mg TDS (to pH 5.8-6.2) • Metabolism of sulforous amino acids produces sulfate and protons pH decreases – Ammonium chloride • Dose: pH dependent 200-500mg TDS (to pH 5.8-6.2) • Modulation of acid base metabolism • Reduction of phosphate excretion – If proven hyperphosphateamia >35 mmol/24hrs – Aluminium hydroxide • Dose 2.2-3.5g/day • Inhibits intestinal phosphate absorption by formatinoof insoluble aluminium phosphate salts • SE: GI upset Cysteine Overview • Frequency 1-2 % • Autosomal recessive hereditary transport defect of the amino acids cystine, lysine, arginine and ornithine (COLA) • Cystine is poorly soluble • Although can present in infancy usually seen in 2nd decade • High urine volume, alkalinisation and educing excretion are mainstays of treatment Notes Medical history • <15 yrs old, 15-20 yrs old at first manifestation • Family history Programme for testing • Urine analysis – pH normal – Sediment with hexagonal, plain crystals • Serum analysis – Normal values • Establishing diagnosis – Cystine test positive – Stone analysis Biochemical investigations 24 hr urine collection • Quantative cystine analysis – – – – – Normal 0.17-0.33mmol/24hrs (40-80mg/24hrs) Homozygous often >4.16 mmol/24hrs (1000mg/24hrs) Start treatment ≥0.8 mmol/24hrs (192mg/24hrs) Limit of solubility 1.33 mmol/l (320mg/L) @ pH 6.0 If diagnosed should arrange family screening • Analysis according to quality standard – Accompanying metabolic disorders can occur. Therefore calcium, oxalate and urate should be checked • Bacteriology – As urine alkalinisation is required a urinary tract infection should be excluded Chemolysis • The solubility of cystine rapidly increase with pH greater than 7.0 • Although possible it is difficult to achieve and may require support of ESWL and visa versa – ESWL + THAM solution (tris-hydroxymethylaminomethane) and acetylcysteine Metaphylaxis 1. Reduction of cystine concentration by extensive urine dilution 2. Reduction of cystine excretion by reducing protein and sodium in the diet 3. Increasing the solubility of cystine by urine alkalinisation 4. Medicinal reduction of urine concentration with sulphide containing compounds General measures • Patient monitored control of pH and close control of relevant serum and urinary parameters – Serum • Creatinine, uric acid – Urine • Volume, density, cystine, pH, nitrite, calcium and phosphate (risk of phosphate stone formation with high pH), oxalate (important with ascorbic acid therapy), uric acid (accompanying metabolic disease possible) • Prevention of infections • Avoid excessive fluid loss Metaphylaxis Urine dilution • To remain below the critical 1.3mmol cystine/L (300mg/l) with excretion of >4.2 mmol/24 hr (1000mg/24hrs) the mean urine volume should be at least 3.5L/day. This needs to be evenly distributed throughout the 24 hr period. • Preferable drinks – HCO3- rich mineral water (Na as low as possible), Citrus juice • Avoid – cola, lemonade, soft drinks with sugar, alcohol Metaphylaxis Diet • Cystine is formed from the metabolism of methionine. However to remove methionine from the diet completely is awful. • Should have a low protein diet <0.8g protein/kg/ day • Vegetarian diet has low protein content and causes urinary alkalinisation and therefore should be the mainstay. – Note in children need iron and iodine so can have 1-2 meat meal and 1 fish meal weekly • Cystine excretion increase with a high sodium intake and therefore NaCl should be limited Metaphylaxis Medical treatment • Alkalinisation (aim for pH >7.5) – Alkaline citrate or sodium bicarbonate • Increase urinary pH • CI: recurrent UTI, hypertension (control!), Phosphate stones, renal insufficiency, metabolic alkalosis, hyperkalaemia • SE: GI disturbances • Long term admin of Na-K-Citrate to patients with reduced renal function can lead to potassium intoxication. Replace with calcium citrate Metaphylaxis • Reduction of cystine excretion – α-Mercaptopropionylglycine (tiopronin, Thiola) • • • • • • Use when cystine excretion >3.0-3.5 mmol/24hrs (720-840mg/24hrs) Start slowly with 250mg/day and increase dependent on cystine excretion to 2g/day Transforms cystine to one molecule cysteine and one molecule cysteine+drug SE:dysgeusia, gastritis, dermatosis, nephrotic syndrome Need to check serum and urine values regularly Tachyphylaxis- loses efficacy during long-term therapy – Ascorbic acid • Changes the redox balance between cystine and cysteine in favour of the latter whichis more soluble • Dose 3-5g/day • SE: Increased excretion of oxalate • Use effervescent tablets as they support alkalinisation, unlike pure ascorbic acid which might result in acidification • Note cystine monitoring and directed therapy not possible by routine analysis a cystine and cysteine are assessed together as total cystine (oxygen oxidises back to cystine) Need to ask for separate measurement 2,8-Dihydroxyadenine stones Overview • Normally 2,8-dihydroxyadenine does not occur as a metabolic product • Autosomal recessive hereditary defect of adenine phosphoribosyltransferase adenine cannot be converted to AMP. • Alternatively adenine is oxidised to 2,8dihydroxyadenine by xanthine oxidase • Usually found in infancy • Ca be confused with uric acid stones • Treatment is with allopurinol Notes • First manifests in infancy • Possible history of stones in the family • Progressive renal insufficiency Programme for testing • Urine analysis – pH normal – Sediment with circular brown crystals • Serum analysis – Normal uric acid • Establishing diagnosis – Stone analysis Biochemical investigations 24 hr urine collection • Quantative 2,8-dihydroxyadenine analysis – If diagnosed should arrange family screening • Analysis according to quality standard – Accompanying metabolic disorders can occur. Therefore calcium, oxalate and urate should be checked Serum • Measurement of APRT activity in the erythrocyte lysate. – Normal 24.7±4.8nmol adenine/mg Hb/H – Homozygous grave or complete loss – Heterozygous moderate loss APRT defect adenine AMP Xanthine oxidase 8-hydroxyadenine Xanthine oxidase 2,8-hydroxyadenine Metaphylaxis Urine dilution • 2.5-3l/day • Can check urine density (>1.010g/cm3 should increase fluid intake) Diet • Reduce purine intake • Ovo-lacto-vegetarian diet Medical • Dose 5-10mg/kg/day in paeds, 200-600mg/day adults • Titrate by measuring the excretion of unmetabolised allopurinol Xanthine stones Overview • Vanishingly rare • Autosomal recessive hereditary defect of xanthine oxidase • Xanthine can not be oxidised to uric acid so excretion of hypoxanthine and xanthine increases • Treatment: hydration, ovo-lacto-vegetarian diet Notes Medical history • Stones in family • Treatment with high dosed of allopurinol • Lesch-Nyhan • Chemo • Mostly presents in infancy Programme for testing • Serum analysis – Markedly decreased serum uric acid <119μmol/l (2mg/100ml) • Establishing diagnosis – Stone analysis Biochemical investigations 24 hr urine collection • Quantative GMP – Xanthine- significantly higher than normal (<40μmol/24hrs) – Hypoxanthine- normal or increased (normal <70μmol/24hrs) – If diagnosed should arrange family screening Serum • Significantly low uric acid Guanosine Guanine Inosine Adenosine AMP Hypoxanthine Xanthine oxidase xanthine Xanthine oxidase Uric acid Metaphylaxis Urine dilution • 2.5-3l/day • Can check urine density (>1.010g/cm3 should increase fluid intake) Diet • Reduce purine intake • Ovo-lacto-vegetarian diet Ammonium Urate Overview • 0.5% • Rare in industrial nations and are normally caused by infections • Unbalanced diet, reduced phosphate intake (from milk and meat) results in a low urinary phosphate buffer increased transformation of glutamine to ammonium. • Low pyrophosphate and a high urinary pH and uric acid excretion results in ammonium urate stone formation Notes Medical history • Unbalanced diet • Phosphate malnutrition • Laxative abuse • Anorexia Programme for testing • Urine Analysis – pH >6.5 – Possible nitrite positive • Serum analysis – Uric acid possibly increased – Hypokalaemia • Establishing diagnosis – Stone analysis Biochemical investigations pH day profile • pH>7.0 infection + increased uric acid excretion • pH6.5-7.0 reduced phosphate excretion 24 hr urine collection • Quantative – – – – – Uric acid >4mmol/24hrs Ammonium >50mmol/24hrs Phosphate very much decreased Sodium decreased Potassium decreased Bacteriology Metaphylaxis General • Treatment of UTI Urine dilution • 2.5-3l/day • Can check urine density (>1.010g/cm3 should increase fluid intake) Diet • Reduce purine intake • Ovo-lacto-vegetarian diet Metaphylaxis Medical • Acidification – Keep pH >6.2 – L-methionine – Ammonium Chloride • Reduction of uric acid excretion – Allopurinol (see uric acid)