Treatment of Osteoarthritis
advertisement

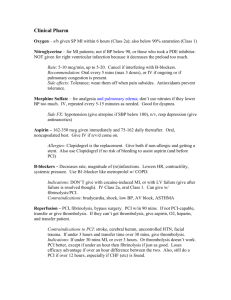
Acute Coronary Syndromes and the Role of Critical Pathway Christopher Cannon, M.D. Brigham and Women’s Hospital Boston 1 Aspirin and Thrombolysis in Acute MI % of Patients 15 35 Day Mortality 13.2 10.7 10.4 10 8.0 5 0 Placebo Aspirin ISIS-2. Lancet 1988; 2:349-60. SK Aspirin + SK 2 TIMI 2: Effect of Time to Treatment % of Patients 10 8 6 Week Mortality *P=0.05 6.2 5.2 6 3.7 4 2 1 hour faster treatment = 3.2* 10 lives saved per 1000 patients treated 0 3-4 h 2-3 h 1-2 h TIMM, et al. Circulation. 1991;84:II-230. <1 h 3 Improving Thrombolysis: t-PA vs. SK % of Patients TIMI 1: Reperfusion Occluded arteries 80 *P<0.001 60 62 0 SK t-PA Mortality 8 7.3 6 *P<0.001 6.3 4 40 20 GUSTO 1: 31 2 0 TIMI Study NEJM 1985;312:397-401. GUSTO Inv. NEJM 1993; 329:673-682. Thrombolysis vs. Primary Angioplasty 30 Day Mortality % of Patients 10 7.2 6.5 4.4 5 4.2 0 Thrombolysis PTCA t-PA Stent + IIb/IIIa Weaver WD, JAMA 1997; 278:2093-2098. Schomig A, N Engl J Med 2000; 343:385-91 5 Medical Treatment After MI Mortality During Follow-up 12.0 11.5 10.7 8.2 8.1 10 6.1 5 at in St ac eb o Pl AC E ac eb o Pl oc ke r Bb l ac eb o 0 Pl % of Patients 15 ISIS-1 Lancet 1986; 2:57-66; HOPE N Engl J Med 2000; 4S. Lancet 1994; 6 344:1383-1389. ACUTE MI GUIDELINES 11/96 Drug Rx Peri MI: Meta-Analyses Number RR Death p value Beta blocker during MI 28,970 .87 (.77-.98) 0.02 Beta blocker post MI 24,298 .77 (.70-.84) <0.001 ACEI during MI 100,963 .94 (.89-.98) 0.006 ACEI post MI if LV dysfxn 5,986 .78 (.70-.86) <0.001 Nitrates during MI 81,908 .94 (.90-.99) 0.03 Ca++ blockers 20,342 1.04 (.95-1.14) NS Magnesium 61,860 1.02 (.96-1.08) NS Lidocaine 9,155 1.38 (.98-1.95) NS Class I Antiarrhythmics 6,300 1.21 (1.01-1.44) 0.04 NEJM 335:1662, 1996 UA/NSTEMI 9/00 Class I Recommendations for Anti-Ischemic Therapy Continuing Ischemia/Other Clinical High-Risk Features • Bed rest + continuous ECG monitoring • 02 to maintain Sa02 >90% • NTG IV • -Blockers, oral • Morphine IV for pain • IABP if ischemia or BP • ACEI for HTN or LVEF (possibly all patients) (+IV if high risk) Braunwald et al. J Am Coll Cardiol. 2000;36:970-1062. 8 UA/NSTEMI 9/00 Class I Recommendations for Antithrombotic Therapy* Definite ACS With Continuing Ischemia or Other High-Risk Features† or Planned PCI Likely/Definite ACS Possible ACS Aspirin + IV heparin + IV platelet GP IIb/IIIa antagonist Aspirin + Subcutaneous LMWH or IV heparin Aspirin * Clinical data on the combination of LMWH and platelet GP IIb/IIIa antagonists are lacking. Their combined use is not currently recommended. † High-risk features were previously listed; others include diabetes, recent MI, and elevated cardiac TnT or Tnl. Braunwald et al. J Am Coll Cardiol. 2000;36:970-1062. 9 Class I Recommendations: Early Invasive Strategy 1. Early invasive strategy in patients with UA/NSTEMI and any of the following high-risk indicators: a. Recurrent angina/ischemia at rest or with low-level activities despite intensive anti-ischemic rx b. Recurrent angina/ischemia with CHF symptoms, S3 gallop, pulmonary edema, worsening rales, or new or worsening MR c. High-risk findings on noninvasive stress testing d. Depressed LV systolic function e. Hemodynamic instability f. Sustained VT g. PCI within 6 months h. Prior CABG 2. In the absence of these, either an early conservative or an early invasive strategy in hospitalized patients without contraindications for revascularization Braunwald et al. J Am Coll Cardiol. 2000;36:970-1062. 10 UA/NSTEMI 9/00 Class I Recommendations: Risk Factor Modification 1. Smoking cessation and achievement or maintenance of optimal weight, daily exercise, and diet 2. HMG-CoA reductase inhibitors for LDL >130 mg/dL 3. Lipid-lowering agent if LDL after diet is >100 mg/dL 4. Hypertension control to a blood pressure of >130/85 mm Hg 5. Tight control of hyperglycemia in diabetes Braunwald et al. J Am Coll Cardiol. 2000;36:970-1062. 11 GUARANTEE Implementation of AHCPR Guidelines for Unstable Angina in 1996: Unfortunate Differences Between Women and Men Results from the GUARANTEE Registry GUARANTEE Global Unstable Angina Registry ANd Treatment Evaluation 6 Regions 35 Hospitals 2,948 Patients GUARANTEE Men No. Pts 1788 Medical Management Women P value 1160 Adjuste d P value On Admission ASA (%) 84 Heparin (%) 66 B-blockers (%)53 80 60 49 0.018 0.001 0.039 0.016 0.080 0.086 At Discharge ASA (or Warfarin)77 69 0.001 0.001 All of above (%) 31 24 0.001 0.007 GUARANTEE Men No. Pts Cath (%) PTCA (%) CABG (%) Catheterization / Revascularization Women 1788 53 1160 44 18 10 12 7% P value Adjuste d P value 0.001 0.001 0.002 0.004 0.017 0.001 0.15 0.16 0.53 0.05 In Pts Meeting AHCRP criteria 59 CABG (% done) 46 Cath (% done) 56 36 GUARANTEE Medical Management Age Age <65 Age >65 P value No. Pts 1638 1309 Adjuste d P value On Admission ASA (%) 83 Heparin (%) 64 B-blockers (%)50 81 62 52 0.17 0.25 0.46 0.24 0.19 0.68 At Discharge ASA (or Warfarin)71 78 0.001 0.003 All of above (%) 28 28 0.92 0.60 GUARANTEE Medical Management Non-Q wave MI vs. Unstable Angina UA No. Pts 2600 NQWMI P value 300 Adjuste d P value On Admission ASA (%) 82 Heparin (%) 61 B-blockers (%)49 87 85 63 0.031 0.001 0.001 0.069 0.001 0.001 At Discharge ASA (or Warfarin)73 82 0.001 0.001 All of above (%) 26 45 0.001 0.001 GUARANTEE TIMI III Registry Pre Guideline Men No. Pts Women Post Guideline Men Women 1678 1640 1788 1160 82 63 41 77 50 35 84 66 53 80 60 49 On Admission ASA Heparin B-blockers Comparing Pre- to Post-: P values : ASA Heparin B-blocker Men 0.30 0.13 0.001 Women 0.05 0.001 0.001 Stone PH et al. JAMA 1996;275:1104; Scirica 1999 AHJ Aspirin within 24 hours 100 94% % survival 80 78% P = .002 60 40 Aspirin ( n = 189 ) 20 No aspirin ( n = 33 ) 0 0 8 16 24 32 Weeks post discharge Giugliano RP,et al. Arch Intern Med 2000;160. 40 48 Heparin within 24 hours 93% 80 85% P = .06 % survival 100 60 40 Heparin ( n = 181 ) 20 No heparin ( n = 47 ) 0 0 8 16 24 32 40 post discharge Giugliano RP,et al. ArchWeeks Intern Med 2000;160. 48 Unadjusted One Year Survival 95% Percent surviving 100 80 P = .0001 81% 60 40 Guideline ( n = 189 ) 20 Not guideline ( n = 86 ) 0 0 8 16 24 32 Weeks post discharge Giugliano RP,et al. Arch Intern Med 2000;160. 40 48 NRMI-1: NRMI-1: Medical Medical Therapy Therapy In-hospital In-hospital Thrombolysis No Thrombolysis No. Pts 84477 156512 ASA (%) 84 63 Heparin (%) 97 56 IV nitro (%) 76 50 IV B-Blockers (%) 17 6 Oral B-Blockers (%) 36 29 Ca-Blockers (%) 29 42 Rogers WJ, et al. Circulation 1994;90:2103-2114. NRMI-2: Distribution of Door-to-Needle Times N=84,423 >90 mins 12% 0-30 mins 34% 61-90 mins 14% 46-60 mins 15% 31-45 mins 25% Cannon CP ACC 2000 40% Baseline Characteristics Door-to-needle time (mins) No. Pts 0-30 28,176 31-60 61-90 33,635 11,531 Age (mean) Female (%) Non-white (%) DM (%) Prior MI (%) Anterior (%) 61.2 26 13 16 16 32 63.5 34 14 20 19 34 13 88 4 1.7 HMO (%) 14 Urban Hosp 87 Pre-hosp ECG 7 Onset-door (hr) 1.4 >90 10,244 P value 65.1 39 16 23 21 37 65.7 42 19 27 21 41 <0.0001 <0.0001 <0.0001 <0.0001 <0.0001 <0.0001 12 87 3 1.9 11 86 3 2.0 <0.0001 0.0005 <0.0001 <0.0001 (Median) 24 MV Adjusted Odds of Death NRMI-2: Thrombolysis Door-to-Needle Time vs. Mortality P=0.0001 1.4 P=0.01 P=NS 1.2 1.23 1.11 1.03 1 0.8 N=28,624 33,867 11,616 10,316 0.6 0-30 Cannon CP ACC 2000 31-60 61-90 Door-to-Needle Tim e (m inutes) >90 MV Adjusted Odds of Death NRMI-2: Primary PCI Door-to-Balloon Time vs. Mortality P=NS 2.2 P=NS P=0.01 P=0.0007 P=0.0003 1.8 1.62 1.4 1.61 1.41 1.15 1.14 1 0.6 0.2 N=2,230 5,734 6,616 0-60 61-90 91-120 4,461 2,627 121-150 151-180 5,412 >180 Door-to-Balloon Tim e (m inutes) Cannon CP, et al JAMA 2000;283:2941-2947. NRMI-2: Primary PCI Distribution of Door-to-Balloon times N=27,080 30 24.4 % of Patients 25 21.2 20.0 20 16.5 15 10 9.7 8.2 5 0 0-60 61-90 91-120 121-150 151-180 Door-to-Balloon Time (minutes) >180 US News and World Report 30-day mortality by hospital category* 30% 25% 20% 15% 10% 5% 0% US News Invasive Non-invasive Stars * 25th, 50th and 75th percentile for each category US News and World Report Aspirin in ideal candidates 100% 80% 60% 40% 20% 0% Top-ranked Invasive Non-invasive 29 US News and World Report Beta-blockers in ideal candidates 100% 80% 60% 40% 20% 0% Top-ranked Invasive Non-invasive 30 30-day Mortality US News Top-ranked vs Other Hospitals Odds ratio 1.1 1 0.9 0.8 0.7 Adjusted* +ASA Adjusted* +BB Adjusted* +RPF * Adjusted for patient, hospital and physician characteristics Quality implications – The lower mortality observed in “America’s Best Hospitals” appear to be explained in part by their higher use of aspirin and beta-blockers – Any hospital can be one of “America’s Best” by increasing their use of aspirin and beta-blockers 32 EUROASPIRE II European Action on Secondary and Primary Prevention through Intervention to Reduce Events Euro Heart Survey Programme European Society of Cardiology-ESC Wood et al. Lancet 2001; 357: 995-1001 European Society of Cardiology ESC Therapeutic control of total cholesterol at interview EUROASPIRE % reaching goal* at interview among those using lipid-lowering medication by center 39 BEL/GHE 31 CZE/PP 70 FIN/KUO 44 FRA/LLRT 41 42 GER/MUNS GRE/ATCI 48 HUN/BUD 55 IRE/DUB 49 ITA/TV 66 NET/ROT 49 POL/CRA 41 SLO/LJU 52 SPA/BAR 65 SWE/MAL 54 UK/HL 51 ALL 0 20 40 * total cholesterol < 5 mmol/l 60 80 100 European Society of Cardiology ESC EUROASPIRE % aspirin/other anti-platelets at interview by center 90 88 BEL/GHE CZE/PP 82 FIN/KUO 86 86 FRA/LLRT GER/MUNS 92 GRE/ATCI 75 HUN/BUD 93 92 IRE/DUB ITA/TV 81 NET/ROT 87 POL/CRA 82 SLO/LJU 86 SPA/BAR 92 SWE/MAL 81 UK/HL 86 ALL 0 20 40 60 80 100 Wood et al. Lancet 2001; 357: 995-1001 European Society of Cardiology ESC % beta-blockers at interview by center EUROASPIRE 77 BEL/GHE 74 CZE/PP 88 FIN/KUO 60 FRA/LLRT 68 GER/MUNS 55 GRE/ATCI 84 HUN/BUD 47 IRE/DUB 61 ITA/TV 48 NET/ROT 62 POL/CRA 66 SLO/LJU 47 SPA/BAR 64 SWE/MAL 44 UK/HL 63 ALL 0 20 40 60 80 100 Wood et al. Lancet 2001; 357: 995-1001 European Society of Cardiology ESC EUROASPIRE II EUROASPIRE Conclusions A high prevalence of unhealthy lifestyles, modifiable risk factors and inadequate use of prophylactic drug therapies is found in coronary patients across Europe Considerable potential to raise the standard of preventive cardiology exists throughout Europe in order to reduce coronary morbidity and mortality Wood et al. Lancet 2001; 357: 995-1001 European Society of Cardiology ESC National Heart Attack Alert Program (NHAAP) CRITICAL PATHWAYS FOR THE TREATMENT OF PATIENTS WITH ACUTE CORONARY SYNDROMES Critical Pathways - Definitions • Standardized protocols for care • Strict definition – Full list of all tasks, tracks variances • Broader definition – Includes clinical protocols (NHAAP 4D’s) • Diagnostic pathways - Chest Pain Centers • Treatment pathways - Thrombolysis 39 Goals of Critical Pathways • Increase use of recommended medical therapies (e.g., aspirin) • Decrease use of unnecessary tests. • Decrease hospital length of stay • Increase participation in clinical research • Improve patient care and decrease costs. 40 Need and Rationale for Critical Pathways • Underutilization of recommended medications (e.g. Aspirin) • Overutilization of procedures • Length of stay, # ICU days • Quality of care measures (door-to-drug, door-to-balloon times) 41 Development And Implementation Of Critical Pathways • Identify problems ( practice variation) • Identify working committee/task force to develop path • Distribute draft Critical Pathway to all personnel and departments involved. Revise based on approach. • Implement pathway • Collect and monitor data on pathway performance. • Modify the pathway as needed to further improve performance. 42 Methods of Implementation of Pathways • Specific case manager for each Pt – High compliance, high cost • Standardized order sheets, Pocket guides • “Championing” - Grand rounds • Recent study -> similar improvements in care with either formal or simpler pathways (Holmboe, ES et al. Am J Med 1999;107:324-31.) 43 44 Goal: < 30 Minutes NHAAP Ann Emerg Med 1994;23:311-29. 45 N R M I1 & 2 T r e n d s :D o o r t o D r u g ( t P A ) I n t e r v a l A l lH o s p i t a l s ,t P A t r e a t e d P a t i e n t s ( N = 2 4 1 , 7 5 7 ) Minut es (median) 65 60 55 50 45 40 90-b 91-a 91-b 92-a 92-b 93-a 93-b 94-a 94-b 95-a 95-b 96-a 96-b 97-a 97-b 98-a 35 W. Rogers, personal communication Speeding Time to Treatment: Brigham and Women’s Hospital Acute MI Critical Pathway in ED __:__ Door Pt. with Chest Pain. ED Arrival Time 10 mins __:__ Data Obtain ECG. Assess for ST Elevation 10 mins __:__ Decision Assess for Contraindications to Thrombolysis: Active Bleeding Prior Stroke Confirmed BP > 190/110 Major Surgery <2 Mos. Other Major Illness (cancer, etc.) 10 mins __:__ Drug Door-to-Drug Time Goal: <30 Mins NO YES o Mix and Give Thrombolytic: Primary PCI: Double-Bolus r-PA 1. Patient with high stroke/bleeding risk 2. Cardiogenic shock 3. (All patients) Cannon CP et al. J Thromb Thrombolysis 1994;1:27-34. 47 BWH Thrombolysis Critical Pathway: Effect on Door-to-Drug times Door-to-Drug Time 80 70 Minutes 60 50 40 30 20 10 0 Jun93 JulSep 93 Pre- OctDec 93 JanMar 94 AprJun 94 Post-Pathway JulSep 94 OctDec 94 JanMar 95 AprJun 95 JulSep 95 OctDec 95 Cannon CP, Clin Cardiol 1999;22:17-22 Door-to-Needle Time (Mins) BWH Thrombolysis Critical Pathway: Initial Experience 120 BEFORE Women Men 100 80 *P=0.013 60 40 20 0 Jun-Nov 20, 93 Nov 21, 93June 94 July 94- Dec 94 Jan 95- June 95 Cannon CP, et al. Clin Cardiol 1999;22:17-22 49 50 PAMI II: Early Discharge Critical Pathway for LowRisk MI Patients treated with Primary Angioplasty 6 month outcomes Early D/C (%) Standard (%) P value Death MI Unstable Angina D/MI/UA/CHF/stroke 0.8 0.8 10.1 15.2 0.4 0.4 12.0 17.5 NS NS NS NS Length of stay (days) Hospital Costs 4.2 $9,658 + 5,287 7.1 $11,604 + 6,125 p<0.001 p=0.002 BWH ED Checklist Orders for UA/NSTEMI UA/NSTEMI Hx. Good Story and/or + ECG, or + CKMB/TnI Hx MI, PCI/CABG Tests •CBC, CMP, PT/PTT CK-MB, TnI •Lipid profile Meds • ASA 325mg chew •Metoprolol IV/PO •Discuss with Cards B - Heparin IV + IIb/IIIa - Enoxaparin SQ - Cath Lab •NTG PRN 53 Hospital Lenght of Stay (Days) Effect of Critical Pathway on Median Length of Stay 6 5 5 5 4 4 4 3 3 3 3 2 2 Oct. Nov. Not On Path On Path 2 1 0 Feb (Pre) July Sept. 54 CHAMP Program to improve Secondary Prevention • Jan 1992- Dec 1995 N=256 pre- and 302 post Pre-CHAMP D/C 1 yr post-CHAMP D/C 1 yr ASA 78% 68% 92% 94% B-blocker 12% 18% 61% 57% ACE 4% 16% 56% 48% Statin 6% 10% 86% 91% LDL <100 6% 58% Fonarow GC et al. Am J Cardiol 2001;87:819-822. 55 Conclusions • Critical pathways hold great promise to improve – Quality of care, – Clinical outcomes – Cost-effectiveness • Initial studies show better quality of care and suggest improved outcomes 56