Anticoagulants - Faculty Sites
advertisement

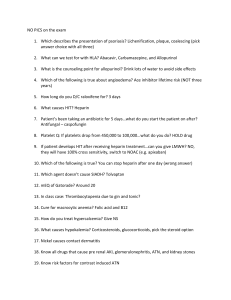
NURS 1950 Pharmacology I 1 Objective 1: identify general reasons anticoagulants are given 2 Objective 2: identify the cells in the body that release heparin Objective 3: describe the actions of heparin 3 Objective 4: list the appropriate routes to administer heparin 4 Heparin: only parenteral administration Warfarin: oral Heparin ◦ Low doses: inhibit clotting factor Xa ◦ High doses: inhibits all clotting factors ◦ Effects occur immediately 5 Preferred during pregnancy, PE, DVT Required for open heart surgery, renal dialysis 6 Side Effects Hemorrhage: observe hypotension, tachycardia, petechiae, bruises May see bloody stools, pelvic pain, headache Hypersensitivity: chills, fever, rash Antidote: protamine sulfate 7 Administration ◦ ◦ ◦ ◦ IV or subq IM causes hematoma Monitor PTT above 1.5-2 X normal is therapeutic Monitor INR: between 2-3 8 Enoxaparin (Lovenox): low molecular weight ◦ Acts so has less potential for hemorrhage, longer duration of action Subq administration Does not affect PT or APTT Do not give to clients allergic to pork byproducts 9 Do not inject IM Do not expel air bubble from syringe before injection Do not rub injection site 10 SE to expect: hematoma with improper injection technique SE to report: bleeding, thrombocytopenia Drug interactions: no clinically significant interactions ◦ Caution: antiplatelet or warfarin therapy 11 Warfarin (Coumarin) ◦ 1st oral ◦ Antidote: Vitamin K ◦ Monitor protime Needs to be 1.5 to 2X normal Monitor INR: 2-3 12 Interactions ◦ ◦ ◦ ◦ Heparin ASA Butazoladin Barbiturates 13 Objective 5: identify the antidote for heparin 14 Objective 6: name the lab tests that are the basis to determine the effectiveness and dosage of heparin ◦ ◦ ◦ ◦ PTT 60-80 PT 2.5-3.5 INR 2-3 APTT 25-35 is normal 2-3x baseline= therapeutic ; measured daily 15 Objective 7: describe the important points regarding subcutaneous administration of heparin ◦ ◦ ◦ ◦ ◦ Dose/strength Injection site Needle/syringe Aspiration Pressure 16 Objective 8: list the signs of heparin overdose ◦ ◦ ◦ ◦ Bleeding VS changes Thrombocytopenia White clot formation is a toxic reaction 17 Objective 9: identify drugs that enhance the action of heparin ◦ ◦ ◦ ◦ ◦ ◦ NSAIDs ASA Ginkgo biloba Dipyridamole Clopidogrel Ticlopidine 18 Objective 10: describe the action of Coumadin ◦ Inhibits the activity of vitamin K—needed for activation of clotting factors II, VII, IX and X 19 Objective 11: name the lab tests done to determine the effectiveness and dosage of Coumadin ◦ 12-15 sec = Normal PT 20 Objective 12: identify drugs that increase and decrease the effectiveness of Coumadin Drugs that can increase Coumadin effects: Tylenol, ASA, dong quai, ginkgo biloba, oil of wintergreen, omeprazole Drugs that can decrease the effects: St. John’s Wort, rose hip, barbiturates, griseofulvin, vitamin C, vitamin K 21 Objective 13: discuss other select anticoagulant agents ◦ Fibrinolytic agents ◦ Antiplatelet drugs 22 Suppress aggregation platelets Prevent arterial thrombus ASA single dose; 5 gr or less ◦ Doubles bleeding time for 4-7 days ◦ Reduces MI, TIAs, CVAs 23 Amicar ◦ Inactivates plasminogen ◦ USE: given IV to reduce hemorrhage in 1-2 hrs ◦ Precaution: no ASA ; DIC is likely problem 24 Streptokinase ◦ Promotes plasminogen to plasmin ◦ Uses Acute coronary thrombi DVT Massive pulmonary emboli ◦ Nursing interventions: Monitor ECG q 15 min during 1st hr of infusion Monitor LOC (intercranial hemorrhage) 25 MI: must give within 6 hours DVT: give within 3 days PE: no more than 5-7 days 26 Side Effects Hemorrhage: use Amicar Fever, allergic reaction Drug given IV 27 Urokinase ◦ Promotes plasminogen to plasmin 28 TPA: tissue type plasminogen activator (Activase) ◦ Synthetic ◦ Clears coronary artery ◦ SE: bleeding 29 Objective 14: discuss the indications for antiplatelet drugs ◦ Previous MI, CVA, TIA ◦ Conditions that predispose to clot formation Some used in combination post cardiac valve replacement Peripheral arterial disease Atrial fibrillation Unstable angina 30 Objective 15: describe the nursing responsibilities associated with a client receiving an anticoagulant, including specific safety considerations 31 Dosage schedules Hydration Lab data Preventing clot formation Patient teaching ◦ Follow-up ◦ Safety 32 ◦ Medic alert bracelet ◦ Symptoms to report ◦ Do not take OTC meds without consulting MD 33