CARDIAC EMERGENCIES ref: Emergency Clinics of NA 1989
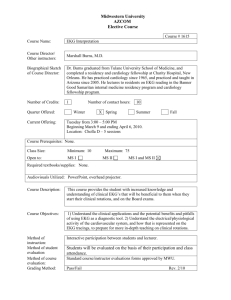
advertisement

CARDIAC EMERGENCIES for Interns Sheilah Bernard, MD 7/1/13 Pt HC • 65 yo female hospital day #2 admitted for untreated hypertension is currently on labetalol 200 tid, hctz 25 qd, and captopril 25 tid • You are called for BP of 200/110 with new chest pain going to left scapula • You ask for a 12-lead EKG and go to the bedside to examine her while reviewing her medications Review of meds/labs • Admission BP 230/120 R and 220/110 L • In the ED pertinent labs included a Cr of 1.8 with a BUN of 22, RBS 132, TnI 0.051, BNP of 312 • CXR shows mild cardiomegaly, mild pulmonary venous redistribution • EKG is unchanged: What do you focus your PE on? • Repeat BP’s manually, R + L arm, femoral pulses, carotid pulses • Appearance (uncomfortable, diaphoretic) • CV system: ?new murmur of AI, S4, S3 • Lungs: Pulmonary edema • CNS: Neurologic signs • TREATMENT Who do you call for help? • Resident • Rapid Response: Get a RN who can push meds • ICU resident for transfer to ICU for parenteral agents • CT surgery, Vascular Medicine Acute management • Control BP first with parenteral agents! – – – – Labetalol infusion Nitroprusside infusion Nicardipine infusion AVOID HYDRALAZINE Blood Pressure Classification JNC 7 BP Classification SBP mmHg DBP mmHg Normal <120 and <80 Prehypertension 120–139 or 80–89 Stage 1 Hypertension 140–159 or 90–99 Stage 2 Hypertension >160 or >100 Distribution of hypertensive emergencies • • • • • • • Acute pulmonary edema/CHF Cerebral infarction (stroke team) Hypertensive encephalopathy Acute coronary syndrome Intracerebral or SA hemorrhage Eclampsia Aortic dissection 35% 25% 16% 12% 5% 5% 2% Definitions of hypertensive crisis • Hypertensive urgency: Acute rise in BP without acute endorgan damage; diastolic BP usually >120 Patients with markedly elevated BP but without acute TOD usually do not require hospitalization, but should receive immediate combination oral antihypertensive therapy. Hypertensive emergency: Acute rise in BP with acute endorgan damage, diastolic BP usually >120 Patients with marked BP elevations and acute Target Organ Damage (e.g., encephalopathy, myocardial infarction, unstable angina, pulmonary edema, eclampsia, stroke, head trauma, life-threatening arterial bleeding, or aortic dissection) require hospitalization and parenteral drug therapy Hypertensive Emergencies Hypertensive Encephalopathy – Headache, nausea/vomiting, change in mental status, neuromuscular irritability – Normal cerebral autoregulation of blood flow is maintained at mean pressure 60-125 mmHg – Goal is to reduce DBP 10-15% or 20-25% reduction in MAP within 30-60 minutes, and to 160/100-110 within 2 hours – http://internal.bmc.org/pharmacy/guidelines/doc uments/mdg_hypertensive_crises.pdf Parenteral treatment of hypertensive emergencies • Labetalol (B-blocker with a-blocker activity) – 20 mg IV/2 min then after 15 min 20-80 mg q 15 bolus or 0.5-2 mg/min infusion – Contraindicated with SB, 2oAVB, CHF, bronchospasm • Esmolol (B1>B2 blockade) – 500 mcg/kg/min for 1 min then 4 min infusion of 50 mcg/kg/min; repeat cycle increasing by 50 mcg/kg/min – Contraindicated with CHF, bronchospasm, 2oAVB – Duration of action 4-16 minutes Parenteral treatment of hypertensive emergencies • Nitroprusside (vasodilator) – 0.25-10 mcg/kg/min to total <3.5 mg/kg – Monitor thiocyanate in CRI, cyanide in liver failure – Caution with high intracranial pressure, phosphodiesterase inhibitors • Nitroglycerin (veno>>vasodilator) – 0.2 mcg/kg/min – Higher dosage often necessary to decrease BP – Caution with high intracranial pressure Parenteral treatment of hypertensive emergencies • Nicardipine (dihydropyridine CCB) – 5.0-7.5 mg/h, slow offset of action (30-40 min) – Contraindicated with advanced AS, caution with ACS – Risk of infusion phlebitis • Enalaprilat (ACE-I) – 1.25 mg IV over 5 min followed by 1.25 mg q 6 h (to max 5 mg q 6 h) – Reduce initial dose to 0.625 mg if patient receiving diuretics, creat elevated – Avoid with AMI, Slow onset of action (hours) Parenteral treatment of hypertensive emergencies • Phentolamine (a1 blocker) – Drug of choice for pheochromocytoma – 1-5 mg IV/IM 1-2 hrs preop, repeat as necessary • Furosemide (Loop-acting diuretic) – Rapid acting, initial venodilator Parenteral treatment of hypertensive emergencies • Alpha-methyldopa (a-adrenergic inhibitor) – Use in preeclampsia – 250-1000 mg bolus IV q 6 hr • Hydralazine (arteriolar vasodilator) – Use “limited to” preeclampsia – Can cause sudden, uncontrolled drop on BP – 10-20 mg IV q 4-6 hours Parenteral treatment of hypertensive emergencies (Elsewhere) • Fenoldopam (dopamine D1 receptor agonist) – 0.1 mcg/kg/min then tititrate at 0.05 to 0.10 mcg/kg/min increments q 15 min – Caution with hypokalemia or glaucoma – No negative inotropic or chronotropic effects (tachycardia) – Flushing common Special hypertensive situations • Aortic dissection – Sodium nipride with b-blockers, labetalol • Acute ischemic stroke – Labetalol or nitroprusside • Cardiac Ischemia – Nitroglycerin with beta blocker • Catecholamine Surge – Phentolamine Chest Pain in the Emergency Department – Aortic dissection • Classification – DeBakey Type I = II + III – Stanford Type A = Type I + II Type B = Type III – Proximal Type A; Distal Type B • DX - Physical exam – Appear shocky with frequently elevated BP – Pulse deficits (25-30%) – AI (30%) – Neurologic manifestation • Imaging techniques (sens % IRAD) – TEE - Unstable pt, if AI or EKG changes (88%) – CT - If no MI/EKG changes; if MRI n/a or CI (93%) – MRI/MRA - Hemodynamically stable (100%) – Angiography - Gold Standard (87%) Pt AF • You are called to the bedside for your patient who c/o PND • The nurse tells you that the monitor has been alarming for HR > 150 for the past 15 minutes, and she is getting an EKG • Patient was admitted for ATCP with negative enzymes, and is awaiting an ETT due to CV risks of Fam hx, HTN, obesity and HL At bedside you find: • BP 165/70 R=L, HR 167 irreg irreg • JVP 9 cm difficult to assess due to obesity, lungs with bibasilar rales and end expiratory wheezing • CV irreg irreg, 2/6 HSM of MR at apex previously known • 1+ LE edema What do you do? • Call resident • Initiate parenteral agents: – – – – IV lopressor 5 mg q 10 min x 3 to slow HR IV lasix to reduce pulmonary congestion Goal HR < 100, goal SBP < 120 Consider IV diltiazem with infusion if poor response to metoprolol • Start PO agents – Start or intensify metoprolol PO How would treatment change if: • • • • • • Pt hypotensive? Pt with Acute MI by EKG with STE? Pt had hemiplegia new onset? RATE CONTROL CARDIOVERSION ANTICOAGULATION Pt ACS A 54-year-old woman is evaluated in the emergency department for jaw and shoulder pain that has occurr Electrocardiogram shows 1.0-mm ST-segment depression in leads V1 through V4 with T-wave inversions. The patient is given aspirin, intravenous nitroglycerin, low-molecular-weight heparin, metoprolol, and atorv • A 54-year-old woman is evaluated in the emergency department for jaw and shoulder pain that has occurred intermittently for the past week • The symptoms occur with activity and are relieved by rest • Physical examination shows a blood pressure of 130/68 mm Hg and a pulse of 90/min Lab data • Labs are normal except for TnI 0.851 (nl < 0.033 ng/ml) • CK’s 133 normal • BNP normal • CXR normal EKG Hospital course • The patient is given aspirin, intravenous nitroglycerin, low-molecular-weight heparin, metoprolol, clopidogrel and atorvastatin • The pain subsides after approximately 20 minutes, and she is admitted to the coronary care unit • One hour later, she has recurrent jaw and shoulder pain. She denies chest pain. A repeat electrocardiogram is unchanged Now what? • Which of the following is the most appropriate immediate treatment for this patient? • A. DC metoprolol and start verapamil • B. DC low-molecular-weight heparin and start unfractionated heparin • C. Start enalapril • D. Start glycoprotein IIb/IIIa inhibitor Pt ACS • UA/NSTEMI pts who have high risk features with recurrent ischemia while on ASA, thienopyridine and anticoagulant should be started on GP2b/3A inhibitor—31-PTCA! • Eptifibatide 180 mcg/kg IV bolus followed by 2 mcg/kg/min (decrease to 1 mcg/kg/min if CrCl < 50 ml/m) • Contraindicated in ESRD • Check plt count 4 hours later then daily Cardiac pacemakers 1957 Pacer modes Atrial pacing Ventricular pacing Pseudofusion pacing (atrial tracking) Dual-chamber pacing (A-V) Dual-chamber pacer leads Implantable cardioverters/ defibrillators (ICD’s) ICD’s--defibrillation Cardiac resynchronization therapy (CRT) www.ccbm.jhu.edu/research /cvs.php CRT pacing Pt with HTN and Stage 2 CKI on ACEI has GI bleed HD #3 Alcoholic admitted with withdrawal seizures on HCTZ K+ up to 3.3 CARDIAC PACING • External Heartstream XL pacing pads for immediate pacing with EKG cable – Atropine – Dopamine – Isoproterenol 2-10 mcg/min • Contraindication – Hypothermia (includes death!) – Late pacing (brady-asystolic > 20 minutes) – VF ICD considerations • Perform ACLS protocols as if patient did not have ICD • External defibrillation can be performed, avoid placing pads over pulse generator • Repetitive, appropriate shocks indicate electrical storm—Call EP fellow: – Active ischemia, lyte imbalance, deterioration of LVEF – Deactivate ICD with magnet placement or reprogramming Defibrillation – Current defibrillators set to pad default (hands-off) – Defibrillation charge bleeds down if not discharged within 15 secs – No EKG cables necessary Refractory Ventricular Defibrillation – Alkalosis – Respiratory acidosis (mechanical ventilation) – Excessive parasympathetic stimulation (atropine) – Excessive catecholamine stimulation – Hypokalemia – Hypomagnesemia – Hypothermia Automatic External Defibrillators • Definition – Shockable rhythm • VT >150/VF – Non-shockable rhythm • Asystole, paced, slow <100 VT/IVR, variable ventricular ectopy, SVT QRS>120, agonal HR < 20 • 5-10 sec analyze/charge time; 1 shock/2 min CPR, biphasic joules • Can be manually overridden (2 buttons in middle push simultaneously) AED FR2 vs Manual Heartstream XL • Defibrillate only, NO PACING, NO SYNCHRONIZED CARDIOVERSION • Leave pads in place, cable transfers to manual Heartstream XL • Manuals all have pad or paddle options, all are biphasic technology • All Heartstream XL have pacing option 59 yo F collapsed in choir Sun AM •Call EMS 3431324 24/7 with trip/EMT # AED AED2 Post-ACLS: Hypothermia? • Indications – S/p VT/VF arrest with <15 min time from collapse to onset of resuscitation – <60 minutes from collapse to restoration of circulation • Contraindications – – – – Trauma, recent surgery Respiratory arrest, sepsis/infections Coagulopathy, conditions predisposed to major bleeds Pregnancy Code Response at BMC (ENC/HAC) • Inpatient Code team (inpatients) – CCU/ICU resident, ICU RN, Anesthesia, Respiratory therapy, Transport, Security, Central equipment • Proceed-out team (non-inpatients) – CCU resident, ICU RN/Resource RN, Transport, Security to bring victim to ED • Rapid Response team – Respiratory therapy, resource RN/RN manager Pericardial Chest Pain – Pericarditis - Clinical diagnosis – Pericardial effusion – Pericardial tamponade • Beck’s triad (1935) of arterial hypotension, elevation of systemic venous pressure and small quiet heart Pericardial Tamponade PE – Elevated JVP with prominent X descent, absent Y descent – Pulsus paradoxus (77%) – Tachypnea (80%), Tachycardia (77%) DX – CXR – EKG – Echo/Doppler • Pericardial effusion • Diastolic RA, RV collapse • Inspiratory reduction of MV early diastolic flows – Swan Ganz/Cath TX – Pericardiocentesis • EKG and Echo guidance – Pericardiectomy/Pericardiotomy Acute endocarditis Fever, murmur, embolic manifestations (MI) DX - Blood cultures (find source) - Echocardiography RX - Medical -Surgical for CHF, persistent fever refractory to therapy, major embolic events, abscess formation, fungal infection, prosthetic valves An approach to the diagnostic use of echocardiography (echo) Baddour, L. M. et al. Circulation 2005;111:3167-3184 Copyright ©2005 American Heart Association