Māori Health Business Unit
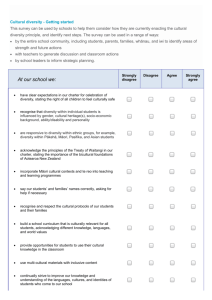
advertisement

Nga Kōrero Mai i Te Kete Hauora Māori Health Business Unit No. 14 March 2013 ISSN 1177-9128 (print) ISSN 1177-911X (online) New research project: Increasing our understanding of asthma The Asthma Foundation and the Ministry of Health have jointly funded a new research project that aims to enable better understanding and management of asthma. The project will focus on young Māori 18 years and under with asthma. It will explore more effective ways to strengthen health literacy and promote greater understanding – both among those with asthma, and those that support them. New Zealand’s incidence of asthma in children and adults is high by world standards – with asthma rates among Māori children (19%) significantly higher than national average (14%). Yet, research has shown that effective management of asthma early in life can significantly influence the effects of asthma later life.1 The research suggests there may be more effective approaches that can be taken and more effective interventions offered – it’s too important to ignore, especially for Māori and especially for young New Zealanders. The 18-month research project will be led by Bernadette Jones and Dr Tristram Ingham – both experienced Māori asthma researchers with the University of Otago. Its objectives are to: • • • • highlight any interventions or approaches that may be effective in strengthening health literacy to allow better understanding and management of asthma in New Zealand investigate and identify health literacy barriers and facilitators in the understanding and management of asthma provide evidence to inform best practice asthma management guidelines and incorporate a health literacy approach to asthma management make recommendations to improve health literacy in order to improve outcomes associated with asthma. The research will help guide our best practice approach to managing asthma in New Zealand. It will identify ways that how health practitioners can better support young sufferers and those at Nga Kōrero 1 risk of developing the condition, as well as helping provide better support and information for those that care for them. The project will run throughout 2013 and is due for completion in June 2014. 1. Ministry of Health. 2012. The New Zealand Health Survey: Content Guide 2011–2012. Wellington: Ministry of Health. From the Deputy Director-General Io Matua kore Kia tata mai koe ki a mātou Whakamanahia, hapaitia ngā tipuranga hou E pupuri nei i ngā taonga tuku iho. Tiakina, Manaaki, Atawhai tonu mai Ngā iwi Māori o te ao Tūturu whakamaua kia tina (tina) Haumi e … hui e … Taiki e! As issues relating to Māori health and wellbeing have received increased attention over recent years, we have witnessed the beginning of a range of new initiatives and programmes targeted at improving health outcomes for Māori. In this issue of Ngā Kōrero we have a look at the progress of a number of these initiatives and examine recent research findings that present something of a barometer for current and emerging health and wellbeing issues for Māori. A number of initiatives are under way to help further improve the delivery of health services for Māori. One component of this is ensuring New Zealand health workers have a basic understanding of cultural competency and health literacy. The Foundation Course in Cultural Competency was launched in June last year and since then a total of around 4000 health workers and their organisations have accessed the free online training. The Ministry is also working with Māori health providers that incorporate general practices to strengthen their clinical governance practices and principles. The aim is to support a greater degree of clinical leadership to these services. We are also undertaking some further health literacy work in 2013 – this time looking at the environments within which health services are accessed and offered, seeking to identify any unnecessary barriers and other potential improvements that can be made. Elsewhere in this issue of Ngā Kōrero we examine some of the recent research findings from three major health studies: the New Zealand Health Survey; the New Zealand Children’s Social Health Monitor 2012 Update; and The Health Status of Māori Children and Young People in New Zealand report. Nga Kōrero 2 Although these reports highlight a number of positive outcomes, they all point to continuing health disparities between Māori and non-Māori. In areas such as smoking, obesity, stroke, heart disease and asthma we still have much work to do. The evidence also suggests that Māori tend to access health services significantly less often than their non-Māori counterparts, despite having greater need for those same services. We need to develop a more precise understanding regarding the physical, financial and psychological barriers that prevent some Māori whānau receiving the support and assistance they need. We then need to address and overcome those barriers, working with providers and the whānau they serve in a much more flexible, collaborative manner. This is the essence of Whānau Ora. Alongside examining some of the challenges more closely, there is much that is celebrated in this issue of Ngā Kōrero. In particular, we congratulate the winners of the 2012 Hauora Māori Scholarships, celebrate Dr Lance O’Sullivan’s Māori of the Year award, and spend some time with Dr George Gray to learn more about the Harkness Fellowship he has been awarded. There is much to celebrate and, yet, there is much still to do. We need to make time for each of these aspects. We’ve tried to reflect that in this edition of Ngā Kōrero. May it encourage you in the work you already do and inspire us all to take it further still. Keep sharing your stories with us – both the successes and the challenges – so that we can all learn from the approach we are each taking. Strong, healthy whānau are the core of a stable, prosperous society. Everything we do must always have the support of whānau at its centre. That is our future. Message from the Associate Minister of Health It is with great pleasure and with a feeling of much success that I write to you this month following the New Zealand Government’s decision to introduce plain packaging for tobacco products. It is another positive step towards reducing the extreme harm caused by tobacco and in achieving our long term goal of a Smoke-Free Aotearoa 2025. I congratulate everyone involved in the prevention of tobacco harm – from our community workers to the medical profession and government agencies. You have worked tirelessly not only to help smokers quit the habit – but also to help reduce the uptake of tobacco use among our most vulnerable. The evidence from experimental studies, marketing experts and the tobacco industry’s own documents is overwhelming. We cannot continue to allow tobacco companies to use sophisticated packaging designs to promote their products as if they were ordinary everyday consumer goods. Let us not forget that approximately 5000 people die each year in New Zealand from smoking-related illnesses and many more suffer from illnesses that diminish their quality of life. Plain packaging for tobacco will mean cigarette packs and tobacco pouches will have much larger pictorial health warnings and be stripped of the marketing imagery tobacco companies use to promote their products. There is a risk that tobacco companies will try and mount legal challenges against any legislation as we have seen in Australia. However, I do not believe that they will succeed. Nga Kōrero 3 Along with plain packaging we will continue to work together with other tobacco control measures to discourage the uptake of smoking and encourage people to give up smoking. I am delighted that New Zealand is on track to be the second country in the world to legislate for plain packaging. I thank you all for your support for what is one of our most important health goals. I know that when we look back in 20 years, this decision will be the right one. Noho ora mai ra Whānau Ora – national update Report on the performance of general practices in Whānau Ora collectives One of the ways we are beginning to see the impact of Whānau Ora is in the way people access and respond to the health services provided by local general practices. We routinely collect data from general practices that are members of Whānau Ora and compare this against an average sample of practices across New Zealand. These evaluations form a series of quarterly reports of the performance of general practices in Whānau Ora Collectives. The report for the September 2012 quarter has now been finalised is available on the Ministry of Health website, www.health.govt.nz The report provides data on key indicators that link to major causes of morbidity and mortality for Māori and support the Whānau Ora Outcomes Framework developed by Te Puni Kōkiri. Although the trends in the report can’t be directly attributed to any single programme or initiative, they point towards positive changes in Whānau Ora service delivery as a whole, with specific improvements in the following areas: • smoking cessation advice – increased by 27 percent (from 20.8 to 47.7%) • CVD risk recording – up 13.8 percent (from 39.7 to 53.5%) • Diabetes Annual Reviews – up 7.6 percent (from 60.3 to 67.9%). General practices within the sample showed improved performances for the year-ending September 2012, across 6 of the 12 indicators. For the first time since data collection began in June 2009, the smoking cessation advice and diabetes annual review results have exceeded those of the national sample. Three of the indicators show a slight decline in performance and data is not yet available for the remaining three indicators. Overall, the Whānau Ora results for the September 2012 year are slightly lower (by 1–4%) than the national sample for the same period. Nga Kōrero 4 When you consider that the proportion of high-needs patients enrolled with general practices under the Whānau Ora Collectives is 61 percent, compared to 27 percent nationally, this is a very strong outcome. The full report offers a breakdown of the data by each individual indicator and is available on the Ministry’s website: www.health. govt.nz/publication/report- performance-general-practiceswhanau-ora-collectives Whānau Ora champions lead the way Any new initiative needs people to make it visible and help lead the way – all the more so when it requires a change in thinking as transforming as Whānau Ora. To take on this challenge, a national whānau champions network has been set up to help advocate and promote Whānau Ora to all New Zealanders. The network has been established with an initial group of four champions that have been charged with building support and visibility for the inclusive approach. The four initial Whānau Ora champions are: • Piriwiritua (Piri) Rurawhe (Rātana) • Charmeyne Te Nana-Williams – home-based rehabilitation and support service director • Brendon Pongia – former national basketball player and media personality • Pati Umaga – a Pacific and disability advocate. As well as gathering positive whānau stories of change, the champions aim to stimulate discussion, build greater understanding and encourage whānau engagement. ‘Whānau Ora is not a programme of deliverables determined by a contract, it is a kaupapa determined by whānau,’ Piri explains, pointing out that whānau are empowered to dream of a better life and a better future. He sees the champion’s role as helping clear a pathway that enables this to occur. Charmeyne sees the champion’s role as an extension of their work supporting families with complex disabilities. ‘Our challenge is to work alongside organisations, community groups and businesses to imbed the Whānau Ora philosophy into their culture so that it becomes a way of being – then help them to apply that philosophy. ‘The Whānau Ora Champions role has provided me with an opportunity to work alongside providers, communities and whānau themselves to determine a Whānau Ora philosophy that can be incorporated within their environments and systems in a way that enhances their existing strengths and kaupapa,’ Charmeyne adds. Nga Kōrero 5 ‘Many of our disabled and Pasefika people and their fanau struggle with the intricacies of the health system – including its processes and language. These unnecessary barriers prevent people accessing the support they need,’ Pati comments. ‘Whānau Ora creates an opportunity for the disabled sector and Pacific fanau to fully access services and entitlements that are available to them.’ The Whānau Ora champions will play a vital role in promoting awareness and understanding of Whānau Ora and the possibilities it represents. Keep an eye out for them in a neighbourhood near you. Health Literacy Cultural competency and health literacy: an online training tool The Foundation Course in Cultural Competency, developed by Mauri Ora Associates on behalf of the Ministry, was launched in June last year. Since then approximately 4000 people have accessed the tool, a number of those include individuals who have taken groups from their organisation through the various online modules. The tool is designed to provide a basic understanding of cultural competency and health literacy. The interactive, multimedia course has three modules, which in total takes about an hour to complete. For those who want to extend their knowledge further, there is a variety of additional online reading and resources. The materials provide an understanding of New Zealand’s culturally diverse population, with an in-depth emphasis on Māori culture. The modules also focus on the importance of health literacy and how health professionals can make a difference. Each training module is supported by videos, video transcripts, additional reading resources and library references. The online course has received very positive feedback from health professionals and providers, with a number of people commenting on how valuable they found the health literacy component. The project was initiated following research highlighting low levels of health literacy among New Zealanders. Greater cultural competency was identified as a key skill to ensure health workers are more consistently able to provide patients and their whānau with health information in a way they can understand. Although a number of providers had begun to address cultural competency as a core skill, the Foundation Course in Cultural Competency brought a consistent approach nationally for the first time. The tool can be freely accessed (following a short registration) at www.mauriora.co.nz Nga Kōrero 6 Cultural competence training can help update the knowledge, skills and attitudes of health workers, allowing them to be more ‘in tune’ with clients and patients. It provides people a much more accessible and welcoming service and can make a very positive difference to patient outcomes and experiences. Culture is about much more than superficial differences. Health professionals who understand this communicate more effectively with people from different cultures who use health services. The highest needs populations also tend to be those with the lowest health literacy. Being able to offer culturally competent care and support will mean these audiences are much more likely to go to health practitioners and health services, and follow their treatment plans. In turn, it encourages them to be more active and engaged in decisions about their health. Since June 2012 the online tool has been available to DHBs, PHOs and both regulated and nonregulated individual health practitioners. The Ministry will shortly evaluate the ongoing use and development of the tool based on what has been learnt from the initial six months. Celebrating achievements Hauora Māori scholarship awards The Ministry of Health’s Hauora Māori scholarship programme has again granted awards to exceptional students. The Hauora Māori Scholarships are funded by the Māori Provider Development Scheme and supports Māori students working towards or completing NZQA accredited health and disability courses. The funding supports some of Aotearoa’s most promising scholars to complete their studies and begin work in their communities towards achieving greater health outcomes and reducing inequalities for individuals and communities across Aotearoa. The awards ceremony in December 2012, hosted by Associate Minister of Health Tariana Turia, was a celebration of emerging talents and those already making a difference in their local communities. It was highlighted with the announcement of the John McLeod Scholarships and the Te Apa Māreikura Award. The John McLeod Scholarships are awarded to outstanding individuals who excel academically while maintaining strong links with whānau, hapū, iwi, and the wider community. Te Apa Māreikura Award acknowledges scholarship applicants who have modeled leadership in community health, academic excellence, who have strong connections and make important contribution to their communities. 2012 John McLeod Scholarships – Eugene Micheal (Ngāti Kahu, Ngāti Tūwharetoa) and Reuben Kirk (Ngāi Tūhoe) According to Eugene, it was his work in a South Auckland pharmacy that inspired him to complete his second degree. In 2012 Eugene completed the sixth year of study in his Bachelor of Medicine and Surgery degree and began a Trainee Internship at Auckland and Northland District Health Boards. He added this qualification to a Bachelor of Pharmacy. Nga Kōrero 7 Eugene works in the community promoting education and health care. As an active member of The University of Auckland’s Māori and Pacific Admissions Scheme, Eugene is often involved in cultural events and symposiums regarding Māori health, and mentors students. Eugene has previously received the Pacificare Trust Respect Award for his work delivering medications to mental health patients and reporting their concerns to health agencies. Eugene’s achievements in his field are evidence of his commitment to educating and supporting his community in order to improve the health outcomes of its members. Fellow recipient Reuben Kirk already holds a Master of Health Practice in Musculoskeletal Physiotherapy. Reuben previously practiced as a physiotherapist in public and private sectors. 2012 was Reuben’s second year of study towards a Bachelor of Medicine and Surgery at the University of Auckland. Rueben’s roles have included working as a Clinical Supervisor at Auckland University of Technology, mentoring and examining postgraduate students during clinical placements; working with Surf Lifesaving New Zealand; volunteering as a medical officer and sports physiotherapist; and acting as a liaison and support person for Māori and Pacific rangatahi. Reuben acknowledges the disparities in Māori and non-Māori health, maintaining that New Zealand health professionals and the government must work together to reduce this disparity. He believes that his cultural heritage and life experiences equip him to contribute to Māori communities and work towards improved Māori health. 2012 Te Apa Māreikura Award – Peter Flynn (Ngāti Porou, Ngāti Kahungunu) In 2012 Peter completed his fourth year of study at the New Zealand School of Acupuncture and Traditional Chinese Medicine (TCM.) He has earned a Bachelor of Health Studies (Acupuncture), with Diplomas in Tuina (TCM Massage) and Qi Gong. Peter also holds a Diploma in Pharmacy. Peter has been a longstanding iwi representative and delegate, actively contributing to a wide range of local and regional committees and rūnanga, including various aspects of Crown consultation. In 2013 Peter intends to establish his own acupuncture practice at home, between his local marae and Greytown, combining his years of experience as a pharmacist with his newly acquired knowledge of traditional Chinese medicine. In the future, Peter also hopes to pursue a newfound interest in rongoā. Māori of the Year Award Kaitāia GP Lance O’Sullivan has been awarded the supreme title Māori of the Year 2012 in the TVNZ Marae Investigates- Ngā Toa Whakaihuwaka Awards. The awards programme was broadcast on Waitangi Day, celebrating Māori excellence and achievement. Awards were made in a number of catergories with Dr O’Sullivan picking up the overall Māori of the Year award for 2012. More information about the other categories and finalists can be found on the TVNZ website, in the Marae Investigates section: http://tvnz.co.nz/marae-investigates/ Nga Kōrero 8 Dr O’Sullivan is renowned for the courage with which he has highlighted the extent of child poverty in New Zealand and its direct impact on child health and wellbeing. ‘As I got more involved in children’s health, especially the tragedy of rheumatic fever, I realised behind that lies poverty,’ he explained in an earlier interview with Northern Advocate 2 in November last year, on the eve of launching his own independent practice. ‘The issues that drive it are not medical; they’re social – poor housing, low incomes, low levels of education and poor access to health care.’ Dr O’Sullivan has been a long-time campaigner for seeing better care being made available to those in greatest need and, often, with the least means. He is well known for treating those who can’t afford it, making house calls to those who can’t come in, and reminding us all that medical practice is first and foremost about a model of care, rather than a model of business. Announcing the award at the event, Associate Health Minister Tarianna Turia congratulated Dr O’Sullivan forhis absolute commitment to his people, acknowledging him as an inspirational health provider and leader, both nationally and within Māoridom. Other award winners included: Master traditional waka navigator Hekenukumai Busby, who was recognised with a lifetime achievement award, actor Rawiri Paratene for the Toi/Arts category, and Lisa Carrington for the hākinakina/sport award. Kerikeri High School received the Rangatahi/Youth Award. For full details, visit the TVNZ Marae Investigates website. Nga Korero and the Te Kete Hauora team also wanted to extend congratulations to Dr O’Sullivan and the rest of the finalists and award winners for 2012. 2 www.northernadvocate.co.nz/news/supreme-honour-for-kaitaia- doctor/1748096/ Harkness Fellowship award Bay of Plenty Public Health Physician, Dr George Gray, is to spend 12 months working alongside leading health experts and policy specialists in the United States, after being awarded the Harkness Fellowship in Health Care Policy and Practice award. Dr Gray was awarded the scholarship in December 2012 and will spend the coming year researching the difference between high-performing public health services and those that struggle to meet the needs of their patients. He hopes to identify the underlying determinants of successful public health provision and then consider how these factors are best implemented within the context of New Zealand’s health service environment. ‘I’ve been aware of the Fellowships for several years. Many of the previous recipients have been people I’ve looked up to – and who’ve gone on to do great projects through the Fellowship,’ Dr Gray reflects. ‘Seeing those people do such great work with the Harkness Fellowship has really motivated me to emulate their example and offer my contribution.’ Nga Kōrero 9 As part of the application process, a range of suggested project themes are indicated. Innovation was one of those themes and the challenges and opportunities it presents for the health sector, resonated strongly with George. ‘If we are to improve health outcomes for Māori, then innovation is the key to doing that. More of the same isn’t going to enable the change in outcomes we need to achieve,’ Dr Gray explains. ‘My project has its basis in innovation and is aimed at learning from the top performers – identifying what it is they do that’s different and what innovations they’ve implemented. ‘Additionally, I’m also going to focus on organisations that have made the transition from operating at a low-to- average level for various health indicators and outcomes, but have successfully transitioned to sit among the high- performers. What enabled the change? What were the key factors and what barriers did they address? What are the key drivers of successful change? ‘It’s about learning from them and identifying what led to success, then looking at how we can apply that here in our context,’ he explains. ‘The differences we see in performance can be as much as two-fold at times, with our lowest performers sometimes achieving half that of the top performers. In an environment where our core organisations basically receive equivalent funding, this shouldn’t be the case. We need to change that,’ adds Dr Gray. Dr Gray argues that the evidence suggests there actually are things we can do to create these changes: ‘Inequalities in health outcomes are not inevitable, but result in differences in the social determinants of health, differential access to services, and ineffective service delivery models. ‘When you delve into this area and look closely at the top performing organisations, some really clear common features emerge in leadership, culture and service delivery models. We can learn from this.’ George is currently working with the Commonwealth Fund to identify where he will be based for the duration of his Harkness Fellowship. At this point it is most likely to be Harvard, Stanford or Kaiser Permanante. George adds that a successful application is a team effort. In particular, he wished to thank Corrina Gage, Mihi Ratima, Teresa Wall, Rhys Jones, Darren Hunt and Janet McLean. The Harkness Fellowship is provided by the Commonwealth Fund. Harkness Fellowships in Health Care Policy and Practice are for promising New Zealand health policy researchers and practitioners to conduct a policy-orientated research project and work with leading health policy experts in the US. It aims to provide a unique opportunity for mid-career health services researchers and practitioners and is open to mid-career professionals who are committed to improving health policy and practice through research, policy analysis, health services, or clinical leadership. The scholarships are co-ordinated locally by Fulbright New Zealand. More information about the scholarships can be found at: www.fulbright.org.nz/awards/ nzscholar/harknessfellowships/ Nga Kōrero 10 Research updates New Zealand Health Survey: Summary of health findings for Māori The first set of key findings from the New Zealand Health Survey (NZHS) has recently been released. The survey provides ongoing information regarding the health and wellbeing of New Zealand adults and children, and illustrates how health services such as GPs and hospitals are used. The findings highlight emerging risks and other areas that need to be considered as we continue to improve the access of quality of our health services. In many areas of healthcare and wellbeing, the findings point to a continuing disparity between Māori and non-Māori – indicating specific areas where health initiatives could be targeted, and improvements may be possible. The first annual findings of the NZHS report that in 2011/12 almost all Māori children were reported as being in good health, and more than four out of five Māori adults reported being in good health. However, Māori rates of obesity and diabetes, for example, far exceed those of their non-Māori counterparts. Additionally, risk factors that affect future health outcomes, such as tobacco use, are substantially higher among Māori. Risk factors The survey illustrates that the activity and food-related statistics are similar for Māori and nonMāori adults: 57 percent of Māori adults are physically active and 64 percent eat at least three daily servings of vegetables. It also found that vegetable intake has improved for Māori since 2006/07, although the incidence of Māori adults eating at least two daily servings of fruit has decreased to 49 percent (against a national average of 59%). One in five Māori children (17%) and two in five Māori adults (44%) are classified as obese. Although obesity rates for Māori adults have not altered since they were recorded in 2006/7, the rate for Māori boys has increased. A further risk factor recorded by the survey is the incidence of smoking. Two out of five (41%) Māori adults state that they smoke; a rate that is more than twice that of non-Māori. While the national smoking rate decreased since 2006/07, the Māori smoking rate remained constant. In terms of dental care, the NZHS indicates that Māori children visited a dental healthcare worker in the past 12 months at the same rate as other children (75%). However, the proportion of Māori adults who visited a dental health care worker in the past year (38%) was significantly lower than the national average (49%). Additionally, the proportion of Māori adults (12%) and children (6%) who reported needing to have a tooth removed, or needing treatment for infections or decay, in the past 12 months was almost twice that of nonMāori. Nga Kōrero 11 The NZHS highlights some important information regarding not only the health of adult New Zealanders, but also factors that may influence the health of succeeding generations. There is significant room for improvement in each of these risk factors towards enabling greater outcomes among Māori. Other general medical conditions The survey also depicts a range of health conditions that are more common in the Māori adult population. Stroke, ischaemic heart disease, diabetes, medicated high blood pressure, chronic pain and arthritis are less frequent in non-Māori adults. The rate of asthma is also higher in Māori adults and children: almost one in five Māori (19% of children and 17% of adults) takes medication for asthma. This rate is greater than for non-Māori, and remains unchanged since the previous findings. Psychological stress is also recorded as more common in Māori (9%), although the proportion of Māori formally diagnosed with common mental disorders is similar to that of non-Māori. These findings suggest there may be barriers that prevent Māori accessing health care for psychological conditions. This potential trend appears to be evident more generally across other areas of healthcare as well. Access to health care The finding that Māori adults (39%) and children (28%) are most likely to have experienced unmet primary healthcare needs in the past year is of significant concern. These rates were 50 percent higher than those of non-Māori participants – with almost half of Māori women (47%) experience unmet health care needs. The primary reasons that survey participants gave for having unmet health care needs included being unable to obtain a GP appointment within 24 hours of needing one and financial barriers that prevent accessing general practitioners and after-hours services. Financial barriers also prevented a significant proportion of Māori adults (18%) and Māori children (12%) from collecting one or more prescription items in the previous year. This percentage is 2.5 times that of non-Māori. These findings highlight continued challenges for Māori in terms of having easy access to the healthcare they need. This requires continuing attention. Reducing inequalities in health care The ongoing nature of the New Zealand Health Survey provides the opportunity to trace trends and improvements in the health and wellbeing of New Zealanders across time. Although these findings highlight some encouraging outcomes, there are many more areas where we need improvement. The data provided through the survey identifies key areas we need to focus on if we are to address the health needs among Māori and decrease the disparity in health status between Māori and non-Māori. As a sector, we need to continue to work with Māori to design and deliver health services that are accessible, appropriate and responsive to Māori. We must find ways to effectively address these challenges if we are to identify a sustainable approach to meeting the current and emerging health care. Nga Kōrero 12 The health of Māori children and young people in Aotearoa Two studies detailing health statistics for New Zealand infants and children were recently released. The New Zealand Children’s Social Health Monitor 2012 Update and The Health Status of Māori Children and Young People in New Zealand provide an overview of contemporary health for Māori and non-Māori in Aotearoa. The New Zealand Children’s Social Health Monitor 2012 update Significant disparities in child health continue in Aotearoa. Māori and Pacific children, and those living in economically deprived areas, continue to reflect increased morbidity and mortality rates. The Children’s Social Health Monitor recently released its 2012 findings. The 2012 update continues the approach of earlier reports, conveying these health findings within the broader economic context in which New Zealand families are living and the apparent effects on child health. Although the report points to a decrease in hospital admissions for some conditions, these findings are offset by increases in other areas. The net result is that we still see overall inequalities for hospital admission in terms of ethnicity. The number of children reliant on benefit recipients also appears to be a strong determinant for child health. Families where benefits are the primary form of income are less likely to visit a doctor, collect prescriptions, or maintain a warm, dry and mold free home. Although the proportion of children reliant on a benefit recipient fell slightly between April 2011 and April 2012, the figure is still an unfavourable one, at one in five New Zealand children (20.1%). Encouragingly, hospital admissions for socioeconomically sensitive medical conditions in Māori children declined during 2009–2011, and in Pacific children between 2009 and 2010. Admission rates for European/Other children peaked in 2010 and then decreased slightly in 2011. Unfortunately, hospital admissions for conditions such as acute upper respiratory tract infections and viral infections of unspecified site, skin infections, dermatitis and eczema and some vaccine-preventable diseases have increased in the last three years. Additionally, admissions for socioeconomically sensitive medical conditions remain much higher for Pacific and, secondarily, Māori children. The 2012 findings for infants and youth in New Zealand also include data regarding assault and Sudden Unexpected Death in Infancy (SUDI). For further information regarding these topics, the full report is available at The Child’s Social Health Monitor website: www.nzchildren.co.nz The Health Status of Māori Children and Young People in New Zealand Commissioned by the Ministry of Health and produced by the NZ Child and Youth Epidemiology Service, The Health Status of Māori Children and Young People in New Zealand is the second in a series of Te Ohonga Ake reports on the health of Māori children and young people. The first examined the health of Māori children and youth with chronic conditions and Nga Kōrero 13 disabilities, while the second provides findings on the health of Māori children and youth generally. The report demonstrates progress evident in a number of health areas: hospitalisations for meningococcal disease have decreased, as has infant mortality and some forms of death by injury. However, hospitalisations have increased for various infectious and respiratory diseases such as acute rheumatic fever, serious skin infections and asthma. The report also highlights continued significant disparities between hospitalisations and mortality for many conditions: non-Māori, non-Pacific children, and youth are less likely to appear within hospitalisation or fatality datasets than their Māori and Pacific counterparts. A strong feature of the report is the editorial by Dr David Tipene-Leach regarding Sudden Unexpected Death in Infancy (SUDI). He notes that recent initiatives to decrease the significant number of Māori infant deaths, which target co-sleeping and smoking during pregnancy, have failed to affect the disparity between Māori and non-Māori, non-Pacific SUDI. However, he highlights a number of innovations developed over the last 10 years, including promoting the use of a wahakura (a woven flax bassinette developed in conjunction with the Nukutere Weavers Collective, Gisborne) or pēpi-pods (a clothes basket that includes a cover and mattress). Research into the effect of these sleep tools continues, prompting Dr Tipene-Leach to describe New Zealand as a leader in innovation in the SUDI/safe sleeping areas. A full copy of the report is available at the University of Otago website: http://dnmeds.otago.ac.nz/departments/womens/paediatrics/research/nzcyes/maori.html Te Kete Hauora highlights Chatham Islands – health and welfare needs report In March last year, the Ministry contracted Ha¯ o te Ora o Wharekauri Trust to develop and deliver suitable Whānau Ora services to residents on the Chatham Islands. Located 800km east of Christchurch, with a population of just over 600, the Chathams present a unique environment for the delivery of health and social services. Working directly with the Chatham Islands’ communities on the development and design of Whānau Ora services will be crucial to ensuring we are able to provide the support and services they need and deliver them in the way they need it. To better understand this, the Ministry is commissioning a report on the specific health needs and context for the Islands. The information gleaned from these activities will be used to guide Hā o te Ora o Wharekauri Trust in the design and development of the Whānau Ora services. The Ministry is currently requesting proposals for this work and expects to have a confirmed provider by the end of March. Nga Kōrero 14 Supporting clinical governance in Māori health providers The Ministry is working to lift the performance of the wider health sector through greater clinical integration. Supporting effective clinical leadership is a critical component of this. With that goal in mind, the Māori Health Business Unit is looking at ways that it can support Māori health providers in their clinical governance activities. Clinical governance is a framework of organisational accountability that supports continuous quality improvement for clinical services. Clinical leadership is a subset of clinical governance. It works as a ‘bottom-up’ process, led by the clinical staff involved in delivering services and implemented in conjunction with management. Clinical governance comprises six key components: leadership, workforce, teamwork, information systems, patient involvement, and service improvement. To kick off this work at the beginning of 2013, the Māori Health Business Unit will be meeting with a number of Māori health providers to understand how their general practitioners, nurse practitioners, registered nurses, other health professionals and managers implement clinical governance practices and principles. These discussions will inform the Māori Health Business Unit’s approach. The photo above shows the Ministry meeting with managers and clinicians from Ora Toa during February. Once a number of discussions have occurred, the next step will be bringing together Māori health providers to test ideas about ways that their activities could be supported by the Māori Health Business Unit. We acknowledge that due to the flexible and localised way that Māori health providers work that a one-size-fits-all approach is unlikely to be well suited. It is for this reason that we are taking a co-production approach so that solutions developed support Māori providers within the context of their services and in a way that acknowledges their aspirations. We will provide further updates about this work programme through this newsletter but in the meantime if you want to know more, please contact Anne O’Brien who is leading this work anne_obrien@moh.govt.nz Te Kāhui Rongoā: Hui taumata – January 2013 The hui taumata held in January 2013 was a significant event in the world of rongoā. It saw the first official gathering of the Te Kāhui Rongoā Trust as they reflected on the past, and worked to shape the future of this kaupapa together over three days of dialogue and discussion. In May 2011, Ngā Ringa Whakahaere o Te Iwi Māori and Te Paepae Matua mo Rongoā, the two previous bodies that have been working to nurture Rongoā Māori across Aotearoa, commenced discussions to merge into a single entity. On 18 November 2012, Te Kāhui Tāwharautanga o Ngā Rongoā was born – the newly formed Te Kāhui Rongoā Trust. Te Kāhui Rongoā will now serve as the recognised national governance body responsible for protecting, nurturing, and promoting Rongoā Māori and Rongoā me ōna Tikanga in Aotearoa. The trust is governed by 20 elected trustees that represent the 10 rohe (regions) of Aotearoa. Nga Kōrero 15 The hui taumata in January was held at Tunohopu Marae in Rotorua and was hosted by the Waiariki Rohe. The kōrero focused on four key goals: • • • • confirming the strategic direction for Te Kāhui Rongoā providing a forum for in-depth discussion about comprehensive Rongoā matters promoting Rongoā services and products increasing Rongoā information and knowledge. The ‘future integration of Rongoā Matauranga and Western medical paradigms’ served as a further guiding theme for the discussions and dialogue across the hui taumata. A key challenge that emerged from the discussions was the importance of working alongside rangatahi and seeking to include rangatahi members on the Board, if they are to be actively engaged in the future of Rongoā Māori and Rongoā Tikanga. It was an important and productive beginning, which sets a solid foundation for the future of Te Kāhui Tāwharautanga o Ngā Rongoā and Rongoā Māori generally. Rongoā me ōna Tikanga Another area of important mahi for the Te Kāhui Rongoā Trust is the formulation of supporting tikanga to guide greater consistency and credibility for Rongoā practice across providers and practitioners. An initial Tikanga Document was prepared during 2012 and a draft copy provided to the Ministry as an initial step, drawn from the common threads of a range of tikanga documents submitted by various rohe in 2011. It was agreed during the hui taumata that this document will now be sent out to each rohe through their respective trustees. The overall tikanga document does not prevent rohe from further developing their own tikanga standards of practice, specific to the needs of their rohe, but it does provide a shared set of standards of practice for rongoā. Standards NZ has recently been engaged by the Ministry of Health to work alongside a range of key stakeholders, including Te Kāhui Rongoā, with the aim of publishing the finalised tikanga document in October 2013. Further information about the document is available either directly from the Te Kāhui Rongoā Trust, or through the representatives of each rohe. Supporting our communities Update from Tumu Whakarae – Riki Nia Nia Working in district health boards has its fair share of challenges, particularly when your aim is to improve systems that traditionally have not been as effective as they may have been (evidenced in part by the diversity of health outcomes we achieve as a system). Nga Kōrero 16 While there is still some way to go in achieving more equitable health outcomes, members of Tumu Whakarae are embracing the performance culture being implemented across the health sector through the Minister’s Health targets and the introduction of standardised Māori health indicators. As reported in the last Ngā Kōrero, Tumu Whakarae has undertaken a project to provide consolidated reports against national Māori health indicators so we can compare and contrast DHB performance in the sector, identifying areas of high performance that we can then learn from. Immunisation One excellent example where performance has lifted since the introduction of targets and indicators is the immunisation of Māori children. Hawke’s Bay DHB and Capital & Coast DHB have been particularly successful, both lifting their immunisation rates above the 95 percent target in 2012. Historically, the coverage rate nationally has been as low as 42 percent (1992). As Hawke’s Bay DHB Immunisation Coordinator Marg Dalton explains, ‘The so-called impossible target has been reached and now 97 percent of all Māori two-year-olds are vaccinated and protected from vaccine preventable diseases. The improvement in Māori immunisation rates show improving health inequalities is possible through the coordinated efforts of everyone working together.’ Working closely with Māori health providers was seen as an imperative part of this positive change; working together to identify ways to promote immunisation more effectively and remove historical barriers. Access to service has been one of the key barriers. In the end this was addressed by making changes in where the service could be delivered and also adding a number of strategies around transport. A similar approach has also adopted at Capital & Coast DHB with robust systems being put in place to ensure children are enrolled with PHOs at birth and a constant and dedicated effort to remove barriers that prevent children being immunised. Māori Capability Development Programme The central region Māori health managers within DHBs have been collaborating on the development of a common Māori capability training framework. Project Leader Lewis Ratapu (Hawke’s Bay DHB) explains, ‘As a region developing the capability of our health workforce to work more effectively with Māori and their Whānau is essential if we are to address historic and persisting disparities. Staff are our greatest asset in this quest!’ This has led to the Māori Capability Development Programme, operating across DHBs and consisting of five key modules: Health Disparities and Māori, The Treaty of Waitangi and Healthcare, Cultural Competence and Māori, Tikanga Māori and Healthcare, and Whānau Ora. The programme will be implemented within in the central DHB region initially, with a view to determining the best modes of delivery, assessment and wider implementation. Nga Kōrero 17 Tane Ora – Māori Men’s Health Conference I was fortunate at the end of last year to attend the 2nd Māori Men’s Health conference in Blenheim. You’ll hear more about Tane Ora elsewhere in this issue of Ngā Kōrero, but the korero that resonated most with me was delivered by inspirational Māori leader Buck Shelford. While Buck is best known for his uncompromising performances on a rugby field, he shared learning from his most recent battle with cancer and offered some simple but practical advice about keeping mentally and physically healthy. He encouraged us all to do three simple things: eat healthier (in particular more real food as opposed to processed food), do one thing a day for ourselves (like an activity that keeps our minds and bodies fit and happy) and finally to spend more time with the people we love. I hope everyone gets a chance to put Buck’s excellent advice into practice this year! Tāne Ora, Whānau Ora – Counties Manukau DHB update Whānau illnesses and sports related injuries became the catalyst for Karaitiana Ripaki-Tamatea to pursue a career in health. Now in his third year of a degree in Physiotherapy from the Auckland University of Technology, Karaitiana is determined to encourage other rangatahi to follow in his footsteps. ‘Growing up I saw a lot of my whānau were sick. I wanted to help them, so even from a young age I was determined to pursue health as a career. What has made me succeed is the support around me and engaging other students in a similar position as me to stay connected. We are like whānau, we are always there for each other if times get hard. That’s what has made my journey easy and I want to share that with as many rangatahi as possible.’ Key to the success of his journey through health has been the workforce development programme – Kia Ora Hauora, spearheaded by the Counties Manukau DHB. Focused specifically on encouraging Māori into the health sector, Kia Ora Hauora offers the support required by Māori students to attain health qualifications regardless of the tertiary institution where they are studying. The programme was a key component at the Mana Tāne Ora Whānau Ora conference held in Blenheim last year in December. ‘We held rangatahi sessions which provided participants with an insight into what can be expected from a career in the health sector. It’s about showing them there’s support, we’re all in the same boat and that there are so many different career options,’ said Karaitiana. Kia Ora Hauora facilitator Tuhakia Keepa said the event which focused on Mana Tāne Ora – Māori Men’s Health, was a huge success and highlighted the overwhelming interest in health that has been generated by the Kia Ora Hauora programme and role models like Karaitiana. ‘Since the inception of Kia Ora Hauora the number of those accessing the services of the programme have exceeded far beyond our expectations. The Mana Tāne Ora Whānau Ora conference showed us that rangatahi are keen to explore health as a career. That excites us and we’ve learnt that by engaging role models and speakers that can motivate and inspire, we’re on the right track. Nga Kōrero 18 ‘It’s all about supporting our rangatahi throughout their entire journey and acknowledging the relevance of health for us as Māori.’ Kia Ora Hauora facilitated rangatahi sessions alongside the main conference focussing on health career workshops, health worker couch discussions with Māori tertiary students like Karaitiana, ta moko and traditional Māori game sessions. A total of 25 rangatahi tāne from around the country were supported by Kia Ora Hauora to attend the conference. ‘The calibre of the keynote speakers which included Sir Mason Durie, Buck Shelford and other health professionals complemented what we at Kia Ora Hauora are trying to achieve. We need Māori to understand the relevance of health to our overall success as a people. And it starts with our rangatahi, giving them the tools to achieve and aspire to become leaders in their chosen course of study,’ said Tuhakia. The bi-annual conference organised by Mana Tāne Ora o Aotearoa is underpinned by a call for a more proactive response to the poor health statistics and lower life expectancy of Māori men. It is a national network designed to address the health and social issues of Māori men. The next conference is set to take place in 2014, with regional hui being held around the motu throughout this year. For more information regarding Mana Tāne Ora o Aotearoa visit their website at: www.taneora.co.nz And if you want to check out what Kia Ora Hauora has to offer you can visit their website at: www.kiaorahauora.co.nz Nga Kōrero 19