evaluation of lower extremity swelling
advertisement
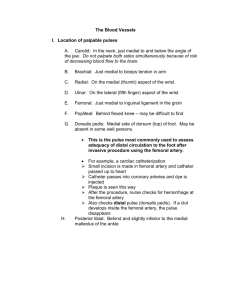
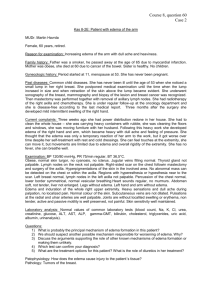
EVALUATION OF LOWER EXTREMITY SWELLING David Southwick DO Medical Director Wound Healing Center Union Hospital Terre Haute Indiana Evaluation of lower extremity can be straight forward or fraught with difficulty Evaluation is largely one of establishing a differential diagnosis OBJECTIVES • 1) Identify the most common causes of lower extremity swelling • 2)Establish a differential diagnosis for less common causes of lower extremity swelling • 3)Explain the pathophysiology of lower extremity swelling • 4)Explain the work up of the most common causes of lower extremity swelling • 5) Explain the work up of less common causes of lower extremity swelling From a practical sense most causes of lower extremity swelling is due to edema edema is defined as a palpable swelling caused by an increase in interstitial fluid volume Etiology of edema • • • • • • • • Increase in intravascular pressure Increase in vessel wall permeability Decrease in the intravascular osmotic pressure Excess bodily fluids Lymphatic obstruction Local injury Infection Medication effect Pathophysiology of edema • 1) Alteration in capillary hemodynamics favoring the movement of fluid from the intravascular to the interstitial space • 2) Retention of dietary or intravenously administered sodium and water by the kidneys • Rose, Burton MD Pathophysiology and etiology of edema I and II Aug 6 2000 Edema, other than localized edema, does not become clinically apparent until the interstitial volume has increased by 2.5 to 3 liters. The reason this is not due to intravascular causes but is due to renal function. Renal compensation • Initial movement of fluid from the vascular space into the interstitium results in reduction of plasma volume and hence tissue perfusion • Decreased tissue perfusion results in renal retention of sodium and water • Some of this fluid stays within the vascular space returning the plasma volume toward normal while most of the fluid enters the interstitium • Net effect is a marked expansion of total extracelluar volume- EDEMA • Rose Burton MD Pathophysiology and etiology of edema I and II Aug 6, 2000 Renal sodium and water retention in most edematous states is an APPROPIATE compensation in that it restores the intravascular space and hence perfusion Workup of Lower Extremity edema Basically there are two reasons for lower extremity edema • 1) Venous origin • 2) Lymphatic origin Differential diagnosis of lower extremity edema • • • • • • • • • • • Venous obstruction Venous insufficiency Deep venous thrombosis Right sides heart failure Pericardial effusion Cor pulmonale Tricuspid stenosis Pulmonary stenosis Tricuspid regurgitation Pericarditis Congenitial heart disease Differential diagnosis continued • • • • • • • Premenstrual fluid accumulation Preeclapsia-eclampsia Pregnancy Idiopathic edema Myxedema Liver diease- cirrhosis Low albumin states Differential diagnosis continued • • • • • • • • • Fluid overload Lipedema Cellulitis Compartment syndrome Baker’s cyst Malignancy Lymphatic obstruction intralumenal and extralumenal Medication effect Limb dependency in wheelchair bound or patients with contractures • • Oedema of the lower extremity- Right Diagnosis.com Dolmatch B, Lower Extremity Venous Thrombosis and Leg Swelling: The Role of CT Venography; Stanford Radiology 10th Annual Multidetector CT Symposium: May 15, 2008 Arumilli,B et al, Painful Swollen leg- Think Beyond DVT and Baker’s Cyst: World Journal of Oncology. V. 6 2008 • Approach to Patient with Edematous Lower Extremity Caveats • The most common cause of lower extremity edema is Chronic Venous Insufficiency• The most common cause of leg edema in females between menarche and menopause is Idiopathic Edema • Common, yet unrecognized, cause of lower extremity edema is Pulmonary Hypertension often associated with Sleep Apnea • Ely, J et al Approach to Leg Edema of Un clear Etiology J. of the American Board of Family Practice MAR- Apr 2006 vol 19 no 2 148-160 • Blankfield R et al Bilateral Leg Edema, Obesity, Pulmonary Hypertension and Obstrctive Sleep Apnea: Arch Intern Med/ vol. 160 Aug 14/28 2000 Caveats continued • For patients greater than 50 years of age CVI is most common cause of leg edema- CVI affects 30% of the population whereas Heart Failure affects only 1%. • Unless otherwise suspected by History and Physical assume one of the above to be true. • Exception to the rule is EARLY heart failure or pulmonary hypertension can cause leg edema before clinically obvious. HISTORY • Duration of edema: acute vs chronic • Previous history lower extremity edema: if positive- response to therapy • Overnight improvement • Other symptoms • Pain: onset, degree and nature • Drug History • History of pelvic or abdominal neoplasia • History cardiac or renal disease • History Sleep Apnea • History Radiation therapy • Travel history/ Country of origin Medications associated with edema • Antihypertensive drugs • Hormones • • • • • • • • • • Calcium channel blockers Beta blockers Clonidine Hydralazine Minoxidil methyldopa Corticosteroids Estrogen Progesterone Testosterone • Other • • • • NSAID’s Monoamine oxidase inhibitors Rosiglitazone, Piogliatazone docetaxel Painful swollen legs • Pain to palpation: DVT, RSD lipedema, ruptured Baker’s cyst or gastrocnemius tear • Acute onset: less then 72 hours duration: DVT • Consider when : history cancer, recent surgery, bed ridden, limb immobilization, hypercoagulable state • Work up DVT: Unilateral painful swollen leg with history: D-dimer: if greater than 500 ng/ml then Doppler: if positive treat • Work up for DVT: Unilateral painful swollen leg without history: Ddimer: if less then 500ng/mg and PE consistent for musculoskeletal etiol then pain control and elevation; if PE etiol still questionable the Venogram. Also consider getting abd/pelvic CT to R/O malgnancy. Travel History or country of origin • Recent travel to tropics or tropical country of origin think parasitic etiology • Elephantiasis: • Lymphatic filariasis: wucheria bancrofti, bruga malayi, bruga timori or protozoal: leischmania • Nonfilarial elephantiasis: volcanic ash residue chemical absorption via bare feet causing irritation and blockage of lymph vessels • Repeated streptococcal infection • Surgical removal lymph nodes • Hereditary birth defect Physical Examination • BMI: Elevated think sleep apnea • Distribution of edema: unilateral, bilateral or generalized • Pain on palpation • Pitting vs Nonpitting edema • Varicosities, telangectasia • Kaposi- Stemmer sign • Skin changes; waxy texture, papillomatosis, hemosiderin deposition, • Systemic signs: JVD, lung crackles, ascites spider hemangiomas jaundice Phlegmasia alba dolens right leg Phegmasia alba dolens Phlegmasia cerulea dolens right leg Unilateral right leg swelling: DVT May Thurner syndrome Compression Left greater saphenous vein by crossing Right common iliac artery Pitting Edema Ruptured Baker’s cyst Right leg Ruptured right gastrocnemius muscle Varicose veins Elephantiasis Left leg Laboratory testing few helpful • • • • • • • CBC UA Electrolytes BUN/ Creatinine Blood sugar Thyroid stimulating hormone Serum albumin If known cardiac history or if suspect cardiac disease • EKG • Echocardiogram: patient greater than 45 y.o. with edema uncertain etiology, suspect other cardiac disease • Chest Xray • Brain natriuretic peptide in dyspneic patient Other testing: base on diagnosis • D-dimer: R/O DVT • Serum lipids: nephrotic syndrome • Lymphosintography: lymphedema • Directed Plain films , MRI : if suspect tumor • Venous doppler: if suspect DVT or Chronic Venous Insufficiency- be specific when ordering test; if suspect CVI specify reflux and perforator evaluation • Arterial doppler with ABI: if suspect CVI – 30% have unsuspected PAD, also compressive therapy requires verification of adequate arterial flow • • Ely J, et al: Approach to Leg Edema of Unclear Etiology JABFM MAR-Apr 2006 vol19 no 2, 148-160 Arumilli B, et al; Painful swollen leg – think beyond deep vein thrombosis or Baker’s cyst- World J Surg Oncol 2008 6:6 Pleomorphic sarcoma post compartment Arumilli: Painful swollen leg- World J Surg Oncol 2008: 6:6 Chronic venous insufficiency • Requirements for venous return are: • Competent bicuspid venous valves • Effective calf muscle contraction: “ankle-calf pump” • Normal respiration Venous pressure deep venous system 80 mm Hg when horizontal Venous pressure superficial venous system is 20-30 mm Hg when horizontal Chronic venous Insufficiency • Characterized by: • Chronic pitting edema • Often has associated with hemosiderin deposition • Ulceration over the “gaiter area” of shins- especially over medial malleolus : shallow ulcers with irregular margins • Common findings of varicose veins, retinacular veins, ankle flaring • Atrope blanche • Stasis dermatitis • Lipodermatosclerosis Venous hemosiderin deposition Venous ulceration Shallow with irregular margins, reddish base with granulation tissue Idiopathic edema • Most common in women in 20-30 year old range • Cyclical edema but may persist throughout menstrual cycle • Pathologic fluid retention in upright position • Weight gain due to fluid retention can be greater than 1.4 kg over 24 hours • Diagnosis by exclusion in young females Summary Unilateral Acute Deep venous thrombosis Ruptured Baker’s cyst Ruptured medial head gastrocnemius muscle Compartment syndrome Chronic • Chronic venous insufficiency • Secondary lympedema • Pelvic tumor or lymphoma causing external pressure on veins • Reflex sympathetic dystrophy • May-Thurner syndrome Bilateral Acute • Bilateral DVT • Acute exacerbation of systemic etiology ie; heart failure or renal disease Chronic • • • • • • • • • • CVI Pulmonary hypertension Heart failure Idiopathic edema Lymphedema Drug effect Premenstrual edema Pregnancy Obesity Renal disease Bilateral Acute Chronic • Liver disease • Secondary lymphedema (tumor, radiation, bacterial infection, filariasis) • Pelvic tumor or lymphoma causing external pressure • Dependent edema- prolonged sitting, wheel chair bound • Diuretic –induced edema • Preeclampsia • Lipedema Bilateral Acute Chronic • Primary lymphedema • Protein losing enteropathy, malnutrition, malabsorption • Restrictive pericarditis • Restrictive cardiomyopathy • Beri beri • Myxedema Zebras • Portal hypertension with a patent paraumbilical vein connection to the leg: Sivo J:J Ultrasound Med 21: 807-809, 2002 • Bilateral peroneal compartment syndrome after horseback riding: Naidu, et al: Am J Emerg Med. 2009 Sep:27(7): 901.e3-5 • Painful leg: a very unusual presentation of renal cell carcinoma. Case report and review of the literature: Gozen et al; Urol Int. 2009;82:472-6 Recommendations • Go with the odds but keep an open mind: remember CVI comprises 30% of population while heart failure comprises only 1% • If condition is chronic you usually have time to work up and assess response to your therapy • There are only a few causes of acute unilateral or bilateral lower extremity edema: all of them are generally bad- time is of the essence for treatment especially if due to DVT or compartment syndrone Recommendations continued • If premenopausal woman without systemic disease think Idiopathic edema. • If edema is chronic and of unclear etiology think Lipedema • Use your history and physical to guide you, supplement with lab and imaging studies; remember the differential is long so can’t use a shotgun approach Recommendations continued • For cases of chronic bilateral lower extremity edema use your H&P to ascertain if Cardiac, Renal ,Liver or Gut ; supplement with labs, imaging as directed. • Think outside the box for more obscure etiologies: sleep apnea, anatomic anomalies Questions?