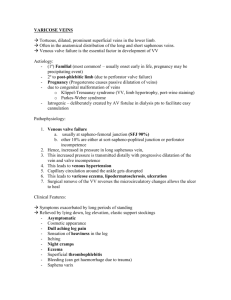
Chronic Venous Insufficiency (CVI) Biggest cause of CVI is varicose
advertisement
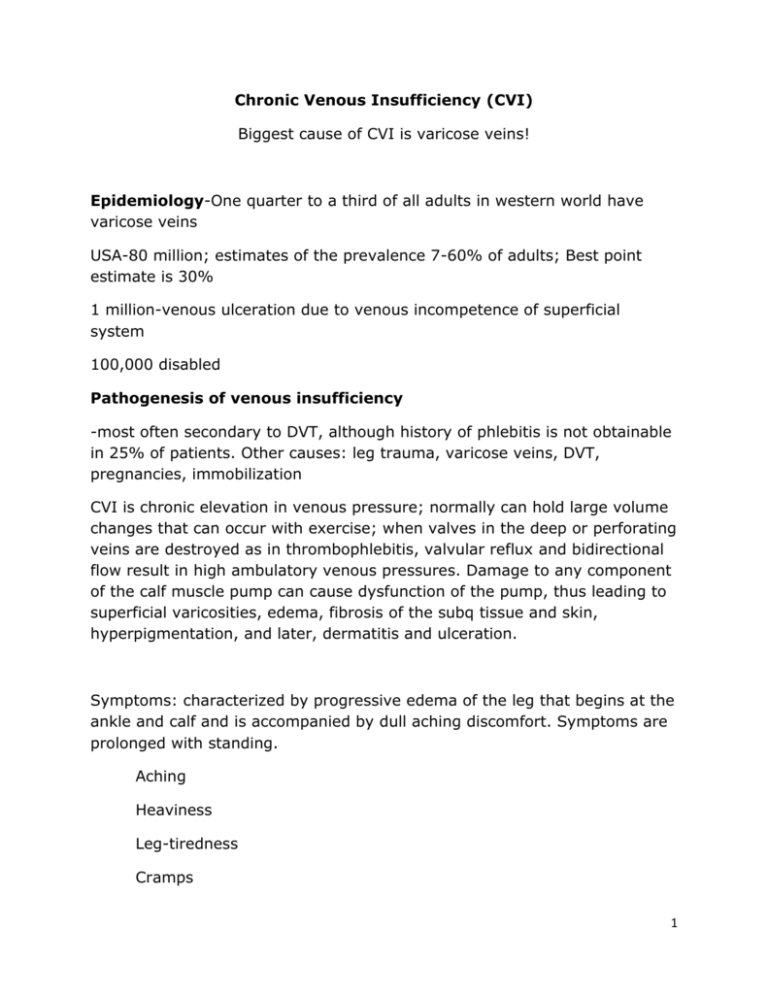
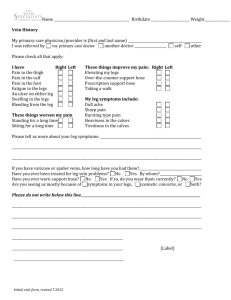
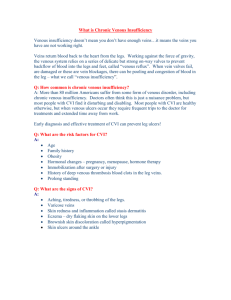
Chronic Venous Insufficiency (CVI) Biggest cause of CVI is varicose veins! Epidemiology-One quarter to a third of all adults in western world have varicose veins USA-80 million; estimates of the prevalence 7-60% of adults; Best point estimate is 30% 1 million-venous ulceration due to venous incompetence of superficial system 100,000 disabled Pathogenesis of venous insufficiency -most often secondary to DVT, although history of phlebitis is not obtainable in 25% of patients. Other causes: leg trauma, varicose veins, DVT, pregnancies, immobilization CVI is chronic elevation in venous pressure; normally can hold large volume changes that can occur with exercise; when valves in the deep or perforating veins are destroyed as in thrombophlebitis, valvular reflux and bidirectional flow result in high ambulatory venous pressures. Damage to any component of the calf muscle pump can cause dysfunction of the pump, thus leading to superficial varicosities, edema, fibrosis of the subq tissue and skin, hyperpigmentation, and later, dermatitis and ulceration. Symptoms: characterized by progressive edema of the leg that begins at the ankle and calf and is accompanied by dull aching discomfort. Symptoms are prolonged with standing. Aching Heaviness Leg-tiredness Cramps 1 Itching Burning Restless legs Signs: Go to the following website for pictures of common findings: http://www.veinclinics.com/cme/skin-findings.html -Skin changes: hyperpigmentation-hemoglobin deposited in the tissues is digested, but the iron remains in the dermis as hemosiderin and produces a brown or brown-red pigmentation in skin surrounding ulcer Edema-unlike the edema associated with salt-retaining conditions such as heart failure and nephrotic syndrome, the edema that precedes venous ulcer formation accumulates under high pressure, creating tissue damage that is tender. 2 Stasis Dermatitis-DeGowin-increased venous and capillary pressures leads to inflammation, edema, subcutaneous fibrosis, and skin atrophy with hemosiderin staining. Often mistaken for cellulitis. With chronic disease, the subcutaneous tissues become fibrotic and the edema no longer pits (brawny edema). The skin becomes thin and easily injured. Lipodermatosclerosis-“Champagne bottle” appearance- leg assumes the shape of an inverted champagne bottle – wide at knee narrow at the ankle) http://dermatlas.med.jhmi.edu/derm/IndexDisplay.cfm?ImageID=12364244 32 Eczema to ulceration Ulceration Review case study of Mr. Crabbe: http://www.worldwidewounds.com/2005/november/Doherty/Encouragepatient-Involvement-Mgt-Lymphovenous.html Review website for pictures of ulcers: http://www.bmj.com/cgi/content/full/320/7249/1589 Differential diagnosis HF CRF Lymphedema-associated with brawny thickening in the subq tissue that does not respond to elevation; edemia is particularly prominent on the dorsum of the feet, and in the toes (sausage toe); varicosities are absent, often history of recurrent cellulitis Acute DVT-need tests Other conditions: automimmune disorders, arterial insufficiency, sickle cell anemia, 3 Comparison-Table, p. 442, Adult Guidelines Comparison of 3 common types of leg ulcers Venous Arterial Neuro/DM Location Lesion features Surrounding skin Palpation findings Gaiter area of legwill break down/medial leg Shallow, partial thickness with irregular borders/shaggy Hyperpigmented, thickened, with dermatitis-stasis changes Non-pitting, tight edema; peripheral pulses may be normal Pressure sites/toes, heels, foot Punched-out, eschar (blackened if necrotic) Pressure sites/plantar, arches heels, toes Punched-out Hair low, not hyperpigmented, atrophic Hair loss, not hyperpigmented, callus Peripheral pulses decreased, capillary refill time increased Altered sensation with touch, vibration, peripheral pulses decreased History-Review Dunphy, 411-415 Physical Examination-Have patient stand or dangle leg to evaluate for edema’ examine groin to the ankle; Inspect and palpate for varicose and telangiectatic veins; Check the medial and lateral ankle regions for skin changes suggestive of chronic venous insufficiency; Inspect the abdomen for enlarged superficial veins if ilio-femoral thrombosis is suspected Pulses Look for ulcers Diagnostics-not needed for intact skin and normal pulses; Order ABI to assess for arterial disease MRI if ulcer and suggestive of osteomyelitis Labs to rule out autoimmune/blood disorders Treatment-Referral Arterial ulcers and neuropathic/DM are referred Pentoxifylline treatment-drug/drug interactions, consideration? 4 If ulcer present use the Rule of 6, see below Do not use TEDS, not enough pressure. Compression Strength 8-15mm 15-20mm 20-30mm 30-40mm 40-50, 50-60 mm Indications Leg fatigue, mild swelling, stylish Mild aching, swelling, stylish Requires prescription-Aching, pain, swelling, mild varicose veins Requires prescription-Aching, pain, swelling, varicose veins, post-ulcer Requires prescription-Recurrent ulceration, lymphedema Procedures Compression Therapy Leg Elevation Sclerotherapy Ambulatory Phlebectomy http://www.veindirectory.org/content/surgical_methods.asp Endovenous Ablation with Laser or Radiofrequency-video Subfascial Endoscopic Perforator Surgery (SEPS) Transilluminated Power Phlebectomy Surgical Stripping Combination of Procedures 5